Ewing Sarcoma—Diagnosis, Treatment, Clinical Challenges and Future Perspectives
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pediatric Soft Tissue Tumors of Head and Neck – an Update and Review
IP Archives of Cytology and Histopathology Research 2020;5(4):266–273 Content available at: https://www.ipinnovative.com/open-access-journals IP Archives of Cytology and Histopathology Research Journal homepage: https://www.ipinnovative.com/journals/ACHR Review Article Pediatric soft tissue tumors of head and neck – An update and review Shruti Nayak1, Amith Adyanthaya2, Soniya Adyanthaya1,*, Amarnath Shenoy3, M Venkatesan1 1Dept. of Oral Pathology and Microbiology, Yenepoya Dental College, Yenepoya University, Mangalore, Karnataka, India 2Dept. of Pedodontics, KMCT Dental College, Kozhikode, Kerala, India 3Dept. of Conservative and Endodontics, Century Dental College Poinachi, Kasargod, Kerala, India ARTICLEINFO ABSTRACT Article history: Pediatric malignancies especially sarcomas are the most common and predominant cause of mortality in Received 01-12-2020 children. Such ongoing efforts are crucial to better understand the etiology of childhood cancers, get better Accepted 17-12-2020 the survival rate for malignancies with a poor prognosis, and maximize the quality of life for survivors. Available online 30-12-2020 In this review article we authors aim to discuss relatively common benign and malignant connective tissue tumors (soft tissue tumor), focusing on current management strategies and new developments, as they relate to the role of the otolaryngologist– head and neck surgeon. Other rarer paediatric head and neck tumors Keywords: beyond the scope of this review Pediatric Sarcoma © This is an open access article distributed under the terms of the Creative Commons Attribution Soft tissue License (https://creativecommons.org/licenses/by/4.0/) which permits unrestricted use, distribution, and Tumor reproduction in any medium, provided the original author and source are credited. -

Advances in Immune Checkpoint Inhibitors for Bone Sarcoma Therapy T Pichaya Thanindratarna,B, Dylan C
Journal of Bone Oncology 15 (2019) 100221 Contents lists available at ScienceDirect Journal of Bone Oncology journal homepage: www.elsevier.com/locate/jbo Review Article Advances in immune checkpoint inhibitors for bone sarcoma therapy T Pichaya Thanindratarna,b, Dylan C. Deana, Scott D. Nelsonc, Francis J. Horniceka, ⁎ Zhenfeng Duana, a Department of Orthopedic Surgery, Sarcoma Biology Laboratory, David Geffen School of Medicine, University of California, 615 Charles E. Young. Dr. South, Los Angeles, CA 90095, USA b Department of Orthopedic Surgery, Chulabhorn hospital, HRH Princess Chulabhorn College of Medical Science, Bangkok, Thailand c Department of Pathology, University of California, Los Angeles, CA, USA ARTICLE INFO ABSTRACT Keywords: Bone sarcomas are a collection of sporadic malignancies of mesenchymal origin. The most common subtypes Immune checkpoint include osteosarcoma, Ewing sarcoma, chondrosarcoma, and chordoma. Despite the use of aggressive treatment Immunotherapy protocols consisting of extensive surgical resection, chemotherapy, and radiotherapy, outcomes have not sig- Bone sarcoma nificantly improved over the past few decades for osteosarcoma or Ewing sarcoma patients. In addition, chon- Anti-PD-1/PD-L1 drosarcoma and chordoma are resistant to both chemotherapy and radiation therapy. There is, therefore, an Anti-CTLA-4 urgent need to elucidate which novel new therapies may affect bone sarcomas. Emerging checkpoint inhibitors have generated considerable attention for their clinical success in a variety of human cancers, which has led to works assessing their potential in bone sarcoma management. Here, we review the recent advances of anti-PD-1/ PD-L1 and anti-CTLA-4 blockade as well as other promising new immune checkpoint targets for their use in bone sarcoma therapy. -

The Role of Cytogenetics and Molecular Diagnostics in the Diagnosis of Soft-Tissue Tumors Julia a Bridge
Modern Pathology (2014) 27, S80–S97 S80 & 2014 USCAP, Inc All rights reserved 0893-3952/14 $32.00 The role of cytogenetics and molecular diagnostics in the diagnosis of soft-tissue tumors Julia A Bridge Department of Pathology and Microbiology, University of Nebraska Medical Center, Omaha, NE, USA Soft-tissue sarcomas are rare, comprising o1% of all cancer diagnoses. Yet the diversity of histological subtypes is impressive with 4100 benign and malignant soft-tissue tumor entities defined. Not infrequently, these neoplasms exhibit overlapping clinicopathologic features posing significant challenges in rendering a definitive diagnosis and optimal therapy. Advances in cytogenetic and molecular science have led to the discovery of genetic events in soft- tissue tumors that have not only enriched our understanding of the underlying biology of these neoplasms but have also proven to be powerful diagnostic adjuncts and/or indicators of molecular targeted therapy. In particular, many soft-tissue tumors are characterized by recurrent chromosomal rearrangements that produce specific gene fusions. For pathologists, identification of these fusions as well as other characteristic mutational alterations aids in precise subclassification. This review will address known recurrent or tumor-specific genetic events in soft-tissue tumors and discuss the molecular approaches commonly used in clinical practice to identify them. Emphasis is placed on the role of molecular pathology in the management of soft-tissue tumors. Familiarity with these genetic events -

Imaging of Pediatric MSK Tumors
Imaging of Pediatric MSK Tumors Kirsten Ecklund, M.D. Boston Children’s Hospital Harvard Medical School [email protected] Tumor Imaging Goals Diagnosis Treatment Surveillance • Lesion • Size, extent • Local recurrence characterization • Treatment response • Metastatic search • Benign vs malignant – Tissue characterization • DDX (necrosis vs growth) – RECIST guidelines • Extent of disease • Surgical planning – Relationship to neurovascular structures – Measurements for custom reconstruction Current MR Imaging Goals • Highest resolution – even at small FOV • Tissue characterization – Functional imaging – Metabolic imaging • Decrease sedation – Motion correction • Increase acquisition speed Diagnosis: Normal RM Stress fx EWS Leukemia Tumor Mimics/Pitfalls • Inflammatory lesions – Osteoid osteoma – Chondroblastoma – Infection – Myositis ossificans – Histiocytosis – CRMO (CNO) • Trauma/stress fracture 19 y.o. right elbow mass Two 15 year olds with rt knee pain D. Femur stress fx, p. tibia stress reaction Primary bone lymphoma Primary Osseous Lymphoma • 6% of 1° bone tumors, <10% of NHL • Commonly involves epiphyses and equivalents • MR - “Infarct-like” appearance, sequestra • 10-30% multifocal • 10-15% metastases at dx 90% of malignant pediatric bone tumors Osteosarcoma ES family of tumors • ~ 400 new cases/yr in U.S. • ~ 200 new cases/yr • #1 malignant bone tumor < 18 y.o. • Caucasian predominance • Peak age: 13-16 y.o., boys > girls • Peak age: 10-15 y.o • Sites: d. femur (75%), p. tibia, p. • Sites: axial (54%), appendicular -

Malignant Bone Tumors (Other Than Ewing’S): Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up by Spanish Group for Research on Sarcomas (GEIS)
Cancer Chemother Pharmacol DOI 10.1007/s00280-017-3436-0 ORIGINAL ARTICLE Malignant bone tumors (other than Ewing’s): clinical practice guidelines for diagnosis, treatment and follow-up by Spanish Group for Research on Sarcomas (GEIS) Andrés Redondo1 · Silvia Bagué2 · Daniel Bernabeu1 · Eduardo Ortiz-Cruz1 · Claudia Valverde3 · Rosa Alvarez4 · Javier Martinez-Trufero5 · Jose A. Lopez-Martin6 · Raquel Correa7 · Josefina Cruz8 · Antonio Lopez-Pousa9 · Aurelio Santos10 · Xavier García del Muro11 · Javier Martin-Broto10 Received: 7 July 2017 / Accepted: 15 September 2017 © The Author(s) 2017. This article is an open access publication Abstract Primary malignant bone tumors are uncommon of a localized bone tumor, with various techniques available and heterogeneous malignancies. This document is a guide- depending on the histologic type, grade and location of the line developed by the Spanish Group for Research on Sar- tumor. Chemotherapy plays an important role in some che- coma with the participation of different specialists involved mosensitive subtypes (such as high-grade osteosarcoma). in the diagnosis and treatment of bone sarcomas. The aim is In other subtypes, historically considered chemoresistant to provide practical recommendations with the intention of (such as chordoma or giant cell tumor of bone), new targeted helping in the clinical decision-making process. The diag- therapies have emerged recently, with a very significant effi- nosis and treatment of bone tumors requires a multidiscipli- cacy in the case of denosumab. Radiation therapy is usually nary approach, involving as a minimum pathologists, radi- necessary in the treatment of chordoma and sometimes of ologists, surgeons, and radiation and medical oncologists. other bone tumors. Early referral to a specialist center could improve patients’ survival. -

Sclerostin Inhibition Alleviates Breast Cancer–Induced Bone Metastases and Muscle Weakness
Sclerostin inhibition alleviates breast cancer–induced bone metastases and muscle weakness Eric Hesse, … , Hiroaki Saito, Hanna Taipaleenmäki JCI Insight. 2019. https://doi.org/10.1172/jci.insight.125543. Research In-Press Preview Bone biology Oncology Breast cancer bone metastases often cause a debilitating non-curable condition with osteolytic lesions, muscle weakness and a high mortality. Current treatment comprises chemotherapy, irradiation, surgery and anti-resorptive drugs that restrict but do not revert bone destruction. In metastatic breast cancer cells, we determined the expression of sclerostin, a soluble Wnt inhibitor that represses osteoblast differentiation and bone formation. In mice with breast cancer bone metastases, pharmacological inhibition of sclerostin using an anti-sclerostin antibody (Scl-Ab) reduced metastases without tumor cell dissemination to other distant sites. Sclerostin inhibition prevented the cancer-induced bone destruction by augmenting osteoblast-mediated bone formation and reducing osteoclast-dependent bone resorption. During advanced disease, NF-κB and p38 signaling was increased in muscles in a TGF-β1-dependent manner, causing muscle fiber atrophy, muscle weakness and tissue regeneration with an increase in Pax7-positive satellite cells. Scl-Ab treatment restored NF-κB and p38 signaling, the abundance of Pax7-positive cells and ultimately muscle function. These effects improved the overall health condition and expanded the life span of cancer-bearing mice. Together, these results demonstrate that pharmacological -

Ewing's Sarcoma and Primary Osseous Lymphoma
36 Ewing’s Sarcoma and Primary Osseous Lymphoma: Spectrum of Imaging Appearances Marc-André Weber, MD, MSc1 Olympia Papakonstantinou, MD2 Violeta Vasilevska Nikodinovska, MD, PhD3 Filip M. Vanhoenacker, MD, PhD4 1 Institute of Diagnostic and Interventional Radiology, University Address for correspondence Marc-André Weber, MD, MSc, Institute Medical Center Rostock, Rostock, Germany of Diagnostic and Interventional Radiology, University Medical Center 2 Second Department of Radiology, National and Kapodistrian Rostock, Ernst-Heydemann-Str. 6, 18057 Rostock, Germany University of Athens “Attikon” Hospital, Athens, Greece (e-mail: [email protected]). 3 Department of Radiology, University Surgical Clinic “St. Naum Ohridski,” University “Ss. Cyril and Methodius,” Skopje, Macedonia 4 Department of Radiology, AZ Sint-Maarten Mechelen, University Hospital Antwerp, Ghent University, Mechelen, Belgium Semin Musculoskelet Radiol 2019;23:36–57. Abstract Ewing’s sarcoma (ES) is a rare, highly malignant anaplastic stem cell tumor. Histolo- gically, the tumor consists of uniform densely packed small monomorphic cells with round nuclei. The typical appearance at hematoxylin and eosin (H&E) staining is small blue round cells without any matrix formation. On conventional radiography, ES typically presents as a permeative lesion in the diaphysis of a long bone in a child. A Keywords large soft tissue component is another characteristic feature, best depicted by ► Ewing’sSarcoma magnetic resonance imaging. ► primary osseous Primary osseous lymphomas are most commonly highly malignant B-cell lymphomas. lymphoma At H&E histologic staining, the tumor stroma consists of diffuse round-cell infiltrates ► radiography that resembles the appearance of ES. Although there is no typical imaging appearance ► magnetic resonance of an osseous lymphoma, it should be considered in an adult presenting with a Lodwick imaging grade II or III lesion in the metaphysis or diaphysis of a large long bone, the pelvis, or the ► review vertebral column. -

Primary Bone Cancer a Guide for People Affected by Cancer
Cancer information fact sheet Understanding Primary Bone Cancer A guide for people affected by cancer This fact sheet has been prepared What is bone cancer? to help you understand more about Bone cancer can develop as either a primary or primary bone cancer, also known as secondary cancer. The two types are different and bone sarcoma. In this fact sheet we this fact sheet is only about primary bone cancer. use the term bone cancer, and include general information about how bone • Primary bone cancer – means that the cancer cancer is diagnosed and treated. starts in a bone. It may develop on the surface, in the outer layer or from the centre of the bone. As a tumour grows, cancer cells multiply and destroy The bones the bone. If left untreated, primary bone cancer A typical healthy person has over 200 bones, which: can spread to other parts of the body. • support and protect internal organs • are attached to muscles to allow movement • Secondary (metastatic) bone cancer – means • contain bone marrow, which produces that the cancer started in another part of the body and stores new blood cells (e.g. breast or lung) and has spread to the bones. • store proteins, minerals and nutrients, such See our fact sheet on secondary bone cancer. as calcium. Bones are made up of different parts, including How common is bone cancer? a hard outer layer (known as cortical or compact Bone cancer is rare. About 250 Australians are bone) and a spongy inner core (known as trabecular diagnosed with primary bone cancer each year.1 or cancellous bone). -

What Is Bone Cancer?
cancer.org | 1.800.227.2345 About Bone Cancer Overview and Types If you have been diagnosed with bone cancer or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is Bone Cancer? Research and Statistics See the latest estimates for new cases of bone cancer and deaths in the US and what research is currently being done. ● Key Statistics About Bone Cancer ● What’s New in Bone Cancer Research? What Is Bone Cancer? The information here focuses on primary bone cancers (cancers that start in bones) that most often are seen in adults. Information on Osteosarcoma1, Ewing Tumors (Ewing sarcomas)2, and Bone Metastases3 is covered separately. Cancer starts when cells begin to grow out of control. Cells in nearly any part of the body can become cancer, and can then spread (metastasize) to other parts of the body. To learn more about cancer and how it starts and spreads, see What Is Cancer?4 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Bone cancer is an uncommon type of cancer that begins when cells in the bone start to grow out of control. To understand bone cancer, it helps to know a little about normal bone tissue. Bone is the supporting framework for your body. The hard, outer layer of bones is made of compact (cortical) bone, which covers the lighter spongy (trabecular) bone inside. The outside of the bone is covered with fibrous tissue called periosteum. Some bones have a space inside called the medullary cavity, which contains the soft, spongy tissue called bone marrow(discussed below). -

Immunological Status of Peripheral Blood Is Associated with Prognosis in Patients with Bone and Soft-Tissue Sarcoma
ONCOLOGY LETTERS 21: 212, 2021 Immunological status of peripheral blood is associated with prognosis in patients with bone and soft-tissue sarcoma YOUNGJI KIM1‑3, EISUKE KOBAYASHI1, YOSHIYUKI SUEHARA2, AYUMU ITO4, DAISUKE KUBOTA1,2, YOSHIKAZU TANZAWA1, MAKOTO ENDO1, FUMIHIKO NAKATANI1, TETSUYA NAKATSURA3, AKIRA KAWAI1, KAZUO KANEKO2 and SHIGEHISA KITANO3,5,6 1Division of Musculoskeletal Oncology, National Cancer Center Hospital, Tokyo 104‑0045; 2Department of Orthopedic Surgery, Juntendo University School of Medicine, Tokyo 113‑8431; 3Division of Cancer Immunotherapy, Exploratory Oncology Research and Clinical Trial Center, National Cancer Center Hospital, Tokyo 104‑0045; Departments of 4Hematopoietic Stem Cell Transplantation, and 5Experimental Therapeutics, National Cancer Center Hospital, Tokyo 104‑0045; 6Division of Cancer Immunotherapy Development, Advanced Medical Development Center, The Cancer Institute Hospital of Japanese Foundation for Cancer Research, Tokyo 135‑8550, Japan Received June 27, 2020; Accepted October 23, 2020 DOI: 10.3892/ol.2021.12473 Abstract. Immune‑checkpoint inhibitors have shown Multivariate Cox regression analysis demonstrated that the promising antitumor effects against certain types of cancer. number of Tim‑3+ CD8+ T cells was associated with lower However, specific immune‑checkpoint inhibitors for patients DFS time. A significant association was also found between with sarcoma have yet to be identified, whereas the immu‑ the number of M‑MDSCs and progression‑free survival (PFS) nological status of peripheral blood in patients with bone time in patients with metastasis. The results suggested the sarcoma and soft‑tissue sarcoma (STS) remains unknown. occurrence of immune surveillance, which indicated that the In addition, it is unclear whether the immunological status host immune reaction against cancer existed in patients with from the peripheral blood could be used as a prognostic bone sarcoma and STS. -
Conventional Chondrosarcoma James C
Conventional Chondrosarcoma James C. Wittig, MD SSSarcoma Surgeon Orthopedic Oncologist General Information Ma lignant mesenc hyma l tumor o f cart ilag inous different iat ion. Conventional Chondrosarcoma is the most common type of chondrosarcoma (malignant cartilage tumor) Neoplastic cells form hyaline type cartilage or chondroid type tissue (Chondroid Matrix) but not osteoid If lesion arises de novo, it is a primary chondrosarcoma If superimposed on a preexisting benign neoplasm, it is considered a secondary chondrosarcoma Central chondrosarcomas arise from an intramedullary location. They may grow, destroy the cortex and form a soft tissue component. Peripheral chondrosarcomas extend outward from the cortex of the bone and can invade the medullary cavity. Peripheral chondrosarcomas most commonly arise from preexisting osteochondromas. Juxtacortical chondrosarcomas arise from the inner layer of the periosteum on the surface of the bone. It is technically considered a peripheral chondrosarcoma. Chondrosarcoma Heterogeneous group of tumors with varying biological behavior depending on grade, size and location Cartilage tumors can have similar histology and behave differently depending on location. For instance a histologically benign appearing cartilage tumor in the pelvis will behave aggressively as a low grade chondrosarcoma. Likewise, a histologically more aggressive hypercellular cartilag e tumor localized in a p halanx of a dig it may behave in an indolent, non aggressive or benign manner. There are low (grade I), intermediate (grade II) and high grade (grade III) types of conventional chondrosarcoma. Low grade lesions are slow growing and rarely metastasize . Low grade chondrosarcomas can be difficult to differentiate from benign tumors histologically. Clinical features and radiographic studies are important to help differentiate. -
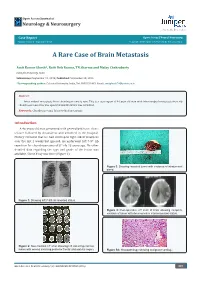
A Rare Case of Brain Metastasis
Open Access Journal of Neurology & Neurosurgery . key to the Researchers Case Report Open Access J Neurol Neurosurg Volume 1 Issue 2 - September 2016 Copyright © All rights are reserved by Katarina Matic A Rare Case of Brain Metastasis Amit Kumar Ghosh*, Rafit Deb Barma, TN Sharma and Malay Chakrabarty Calcutta University, India Submission: September 19, 2016; Published: September 28, 2016 *Corresponding author: Calcutta University, India, Tel: ; Email: Abstract Intracerebral metastasis from chondrosarcoma is rare. This is a case report of 46 year old man with intracerebral metastasis from rib chondrosarcoma who was operated and literature was reviewed. Keywords: Chondrosarcoma; Intracerebral metastasis Introduction A 46 years old man presented with generalised tonic clonic seizure followed by drowsiness and admitted in the hospital. History revealed that he had developed right sided weakness over the last 2 weeks but ignored. He underwent left 7-9th rib resection for chondrosarcoma of 8th rib 13 years ago. No other detailed data regarding the type and grade of the lesion was available. Chest X-ray was done (Figure 1). Figure 3: Showing resected tumor with evidence of intratumoral bleed. Figure 1: Showing left 7-9th rib resected status. Figure 4: Post-operative CT scan of brain showing complete excision of tumor with decompresive craniectomised status. Figure 2: Non-contrast CT scan showing left sided hyperdense lesion with edema involving posterior frontal and parietal region. Figure 5A: Histopathology showing malignant cartilage. Open Access J Neurol Neurosurg 1(2): OAJNN.MS.ID.55560 (2016) 001 Open Access Journal of Neurology & Neurosurgery differentiated chondrosarcoma (Figure 5A, 5B, 5C, 5D, 5E).