Apoptosis: an Introduction for the Endodontist
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DUKE UNIVERSITY School of Medicine Pathologists' Assistant
DUKE UNIVERSITY School of Medicine Pathologists’ Assistant Program Department of Pathology Academic Programs The Department of Pathology at Duke University offers a wide array of training programs to fit individual requirements and goals. The Residency Training program is an ACGME approved program and is available as an Anatomic Pathology/Clinical Pathology combined program, a shorter Anatomic Pathology only program, or an Anatomic Pathology/Neuropathology program. Subspecialty fellowships in Cytopathology, Dermatopathology, Hematopathology, Medical Microbiology, and Neuropathology are also ACGME approved. These programs provide the highest quality of graduate medical education by drawing on the depth and breadth of faculty expertise in the Department in all aspects of anatomic and clinical pathology and the availability of a wide variety of often complex clinical cases seen at Duke University Health System. For medical students interested in a career in Pathology pre-doctoral fellowships, internships and externships are available. Research Training in Experimental pathology can be obtained through Pre- and postdoctoral fellowships of one to five years. All pre-doctoral fellows are candidates for the Ph.D. degree in pathology. The Ph.D. is optional in postdoctoral programs, which provide didactic and research training in various aspects of modern experimental pathology. A two year NAACLS accredited Pathologists’ Assistant Program leads to a Master of Health Science degree, certifies graduates to sit for the ASCP Board of Certification examination, and leads to exciting career opportunities in a variety of anatomic pathology laboratory settings. Pathologists’ assistants are analogous to physician assistants, but with highly specialized training in autopsy and surgical pathology. This profession was pioneered in the Duke Department of Pathology 50 years ago, and is one of only twelve such programs in existence today. -
Teeth What Do I Need to Know?
Teeth What do I Need to Know? Enamel Enamel is a semitranslucent, highly mineralized crystalline solid which covers the crowns of teeth and acts as a barrier to protect the teeth. Dentin Dentin is less mineralized than enamel, but more mineralized than bone; it acts as a cushion for the enamel and a further barrier to the pulp. Pulp Questions? The pulp is the area in the middle of the tooth containing the blood vessels and nerves for that tooth. If you would like more Pulp Horns information or have any The projections of the pulp underneath the taller parts of the tooth, or the “cusps.” specific questions, contact*: These are the areas of the pulp which are closest to the functional (or “occlusal”) part of the tooth which is used to chew food. Leslie Blackburn Cementum XLH [email protected] Protects the dentin and pulp of the roots the and way enamel protects it in the crown. or [email protected] My Teeth XLH Network contact: Raghbir Kaur, DMD; [email protected] Scientific Advisory Board *Please include XLH in the subject line of the email. Challenges Yale-New Haven Pediatric Dental Center 1 Long Wharf Dr, Suite 403, New Haven, CT 06510 Suggestions http://www.ynhh.org/medical-services/dental_pediatric.aspx What is the Most Important Thing to Know? It is not your fault. People with XLH have unique dental challenges. Sometimes even when you are doing everything right you may still have dental problems. While it is important to do everything you can to keep your mouth healthy, it is also important to remember that you some things about your oral health are out of your control. -

Pulpotomy Treatment for Primary Teeth
2010 National Primary Oral Health Conference October 24-27 Gaylord Palm, Orlando, Florida Pulpotomy treatment for primary teeth Enrique Bimstein Professor of Pediatric Dentistry University of Florida College of Dentistry. Pulpotomy treatment for primary teeth Goal The participants will become familiar with the basic knowledge and procedures required for the performance of the pulpotomy treatment in primary teeth. Pulpotomy treatment for primary teeth Topics Introduction Definition and rationale. Indications and contraindications. Materials and techniques. Pulpotomy technique (clinical procedures). Pulpotomy follow up. Summary and conclusions. Pulpotomy treatment for primary teeth Topics Introduction Definition and rationale. Indications and contraindications. Materials and techniques. Pulpotomy technique (clinical procedures). Pulpotomy follow up. Summary and conclusions. Preservation of the primary teeth until their time of exfoliation is required to: a. Maintain arch length, masticatory function and esthetics. Preservation of the primary teeth until their time of exfoliation is required to: a. Maintain arch length, masticatory function and esthetics. Preservation of the primary teeth until their time of exfoliation is required to: a. Maintain arch length, masticatory function and esthetics. b. Eliminate pain, inflammation and infection. Preservation of the primary teeth until their time of exfoliation is required to: a. Maintain arch length, masticatory function and esthetics. b. Eliminate pain, inflammation and infection. c. Prevent any additional pain or damage to the oral tissues. Despite all the prevention strategies, childhood caries is still a fact that we confront every day in the clinic. The retention of pulpally involved primary teeth until the time of normal exfoliation remains to be a challenge. Primary teeth with cariously exposed vital pulps should be treated with pulp therapies that allow for the normal exfoliation process. -

Department of Experimental Pathology, Immunology and Microbiology 531
Department of Experimental Pathology, Immunology and Microbiology 531 Department of Experimental Pathology, Immunology and Microbiology Interim Chairperson: Zaatari, Ghazi Vice Chairperson: Matar, Ghassan Professors: Abdelnoor, Alexander; Khouri, Samia; Matar, Ghassan; Sayegh, Mohamed; Zaatari, Ghazi Associate Professor: Rahal, Elias Assistant Professors: Al-Awar, Ghassan; El Hajj, Hiba; Shirinian, Margret; Zaraket, Hassan The Department of Experimental Pathology, Immunology and Microbiology offers courses to medical laboratory sciences (MLSP) students as well as nursing, medical, and graduate students. It offers a graduate program (discipline of Microbiology and Immunology) leading to a master’s degree (MS) or doctoral degree (PhD) in Biomedical sciences. The requirements for admission to the graduate program are stated on page 33 of this catalogue. IDTH 203 The immune System in Health and Disease 37.28; 3 cr. See Interdepartmental Courses. IDTH 205 Microbiology and Infectious Diseases 37.28; 5 cr. See Interdepartmental Courses. MBIM 223 Parasitology for MLSP Students 39.39; 4 cr. Second semester. MBIM 237 Microbiology and Immunology for Nursing Degree Students 32.64; 3 cr. A course on the fundamental aspects of medical microbiology and immunology for nursing students. Second semester. MBIM 260 Elective in Infectious Diseases for Medicine III and IV 0.180 A course on basic evaluation, diagnosis, and management of infectious diseases. One month. MBIM 261 Elective in Immunology for Medicine III and IV 0.180 A course that is an introduction to immunological research and its application to clinical practice. One month. MBIM 310 Basic Immunology 32.32; 3 cr. A course on innate and adaptive immune mechanisms, infection and immunity, vaccination, immune mechanisms in tissue injury and therapeutic immunology. -
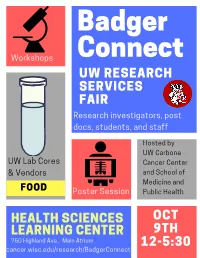
Badgerconnect 2019 Program
Badger Connect Workshops UW RESEARCH SERVICES FAIR Research investigators, post docs, students, and staff Hosted by UW Carbone UW Lab Cores Cancer Center & Vendors and School of Medicine and FOOD Poster Session Public Health HEALTH SCIENCES OCT LEARNING CENTER 9TH 750 Highland Ave., Main Atrium 12-5:30 cancer.wisc.edu/research/BadgerConnect BadgerConnect Research Services Fair October 9th, 2019 12:00 – 5:30 PM, HSLC Atrium AGENDA 12:00 – 12:30pm Registration / Networking Registration table and networking at booths open at 12pm 12:30 – 2:00pm Flash Talks Lunch (Rm 1306 HSLC) ~4 minute flash talks by research services throughout lunch 15’ Break/Networking 2:15 – 2:45pm Workshop Session I Rm 1220 HSLC Rm 1222 HSLC Rm 1244 HSLC Reference Grade De Novo Assemblies and Whole Team Science 101: How to How to create a tissue Topic Transcriptomes: See the Big build, lead, and manage a microarray (TMA) Picture With Pacbio SMRT team that does great science Sequencing UW Translational Research Biotechnology Center DNA Team Science - ICTR and Service Initiatives in Pathology Lab Sequencing Facility UWCCC Vendor n/a Pacific Biosciences n/a 15’ Break/Networking 3:00 – 3:30pm Workshop Session II Rm 1220 HSLC Rm 1222 HSLC Rm 1244 HSLC LabArchives: The Electronic Hyperfinder: Computational Creating Novel Disease Models Topic Lab Notebook Service for Sorting for High-Dimensional with CRISPR Campus Flow Cytometry Data UW Genome Editing and Animal Electronic Lab Notebook Flow Cytometry Lab Service Models Core Service Integrated DNA Technologies, Vendor LabArchives -

Overview of Pathology and Its Related Disciplines - Soheir Mahmoud Mahfouz
MEDICAL SCIENCES – Vol.I -Overview of Pathology and its Related Disciplines - Soheir Mahmoud Mahfouz OVERVIEW OF PATHOLOGY AND ITS RELATED DISCIPLINES Soheir Mahmoud Mahfouz Cairo University, Kasr El Ainy Hospital, Egypt Keywords: Pathology, Pathology disciplines, Pathology techniques, Ancillary diagnostic methods, General Pathology, Special Pathology Contents 1. Introduction 1.1 Pathology coverage 1.1.1 Etiology and Pathogenesis of a Disease 1.1.2 Manifestations of Disease (Lesions) 1.1.3 Phases Of A Disease Process (Course) 1.2 Physician’s approach to patient 1.3 Types of pathologists and affiliated specialties 1.4 Role of pathologist 2. Pathology and its related disciplines 2.1 Cytology 2.1.1 Cytology Samples 2.1.2 Technical Aspects 2.1.3 Examination of Sample and Diagnosis 3. Pathology techniques and ancillary diagnostic methods 3.1 Macroscopic pathology 3.2 Light Microscopy 3.3 Polarizing light microscopy 3.4 Electron microscopy (EM) 3.5 Confocal Microscopy 3.6 Frozen section 3.7 Cyto/histochemistry 3.8 Immunocyto/histochemical methods 3.9 Molecular and genetic methods of diagnosis 3.10 Quantitative methods 4. Types of tests used in pathology 4.1 DiagnosticUNESCO tests – EOLSS 4.2 Quantitative tests 4.3 Prognostic tests 5. The scope of SAMPLEpathology & its main divisions CHAPTERS 6. Conclusions Glossary Bibliography Biographical sketch Summary Pathology is the science of disease. It deals with deviations from normal body function and ©Encyclopedia of Life Support Systems (EOLSS) MEDICAL SCIENCES – Vol.I -Overview of Pathology and its Related Disciplines - Soheir Mahmoud Mahfouz structure. Many disciplines are involved in the study of disease, as it is necessary to understand the complex causes and effects of various disorders that affect the organs and body as a whole. -

MEDICAL UNIVERSITY of SOUTH CAROLINA Charleston, SC
MEDICAL UNIVERSITY OF SOUTH CAROLINA Charleston, SC PROGRAMS OFFERED The Department of Pathology and Laboratory Medicine of the Medical University of South Carolina offers a fully accredited training program in anatomic and clinical pathology (AP/CP). The AP/CP program consists of a 39 month core curriculum with 9 months of elective. Anatomic Pathology core rotations include autopsy pathology/forensic pathology, surgical pathology, cytopathology, dermatopathology and VA pathology. Clinical Pathology core rotations include hematopathology, immunopathology, clinical chemistry, microbiology, tranfusion medicine, apheresis, histocompatibility laboratory, molecular pathology, cytogenetics, VA pathology, laboratory management and informatics. Nine months elective time is available for more in-depth studies in areas of special interest and/or research. A graduate (PhD) program in experimental pathology is available and may be coordinated with the residency training program. Fellowships are offered at the discretion of the Chair in forensic pathology, dermatopathology, cytopathology, surgical pathology, gastrointestinal pathology, hematopathology and clinical chemistry. TYPES AND NUMBERS OF APPOINTMENTS The institution is accredited for twenty-two residency positions in anatomic pathology and clinical pathology, with an even distribution of residents at all levels. Persons seeking the PhD degree in experimental pathology must meet the requirements of the College of Graduate Studies, Medical University of South Carolina. The department participates -
Pathology: a Career in Medicine the Study of the Nature of Disease, Its Causes, Processes, Development, and Consequences
PATHOLOGY A Career in Medicine The Intersociety Council for Pathology Information (ICPI) www.pathologytraining.org 2015 Pathology: A Career in Medicine The study of the nature of disease, its causes, processes, development, and consequences. Pathology is the medical specialty that provides a scientific foundation for medical practice The pathologist is a physician who specializes in the diagnosis and management of human disease by laboratory methods. Pathologists function in three broad areas: as diagnosticians, as teachers, and as investigators. Fundamental to the discipline of pathology is the need to integrate clinical information with physiological, biochemical and molecular laboratory studies, together with observations of tissue alterations. Pathologists in hospital and clinical laboratories practice as consultant physicians, developing and applying knowledge of tissue and laboratory analyses to assist in the diagnosis and treatment of individual patients. As teachers, they impart this knowledge of disease to their medical colleagues, to medical students, and to trainees at all levels. As scientists, they use the tools of laboratory science in clinical studies, disease models, and other experimental systems, to advance the understanding and treatment of disease. Pathology has a special appeal to those who enjoy solving disease-related problems, using technologies based upon fundamental sciences ranging from biophysics to molecular genetics, as well as tools from the more traditional disciplines of anatomy, biochemistry, pharmacology, physiology and microbiology. The Pathologist in Patient Care The pathologist uses diagnostic and screening tests to identify and interpret the changes that characterize different diseases in the cells, tissues, and fluids of the body. Anatomic pathology involves the analysis of the A biosample robot prepares specimens for gross and microscopic structural changes caused by testing disease in tissues and cells removed during biopsy procedures, in surgery, or at autopsy. -

Editorial Note on Medical Microbiology & Diagnosis – Clinical
Manuscript no.- JMMD-2021-5 Article type- Editorial Received date- 20-01-2021 Accepted- 20-01-2021 Publish date-23-01-2021 Editorial Note on Medical Microbiology & Diagnosis – Clinical Microbial Pathology Tirpude RJ Defence Institute of Physiology and Allied Sciences Address for Correspondence: Tirpude RJ, Defence Institute of Physiology and Allied Sciences, Delhi - 110054, India. Tel-9869217101, E-mail: [email protected] Editorial Clinical pathology is concerned with the diagnosis of disease based on laboratory analysis of body fluids like urine and blood. It deals with the tools of microbiology like macroscopic, microscopic, analyzers and cultures. It covers microbiology, host-pathogen interaction and immunology related to infectious agents, including bacteria, fungi, viruses and protozoa. It also accepts papers in the field of clinical microbiology, with the exception of case reports. The pathogenesis of a disease is the biological mechanism that leads to the diseased state. It also describes the origin and development of the disease, and whether it is acute, chronic, or recurrent. Medical microbiology involves the identification of microorganisms for the diagnosis of infectious diseases and the assessment of likely response to specific therapeutic interventions. Major categories of organisms include bacteria, mycobacteria, fungi, viruses, and parasites. Microbiological methods combined with clinical symptoms, additional laboratory tests, and imaging techniques are used in combination to distinguish a true disease- associated infection from colonization with normal flora or other conditions, such as malignancies, inflammatory disorders, or autoimmune disorders, all of which have unique therapies and prognoses for the patient. Laboratories combine the use of traditional microscopy and culture methods, with a rapidly evolving set of molecular and proteomic techniques. -

1 – Pathogenesis of Pulp and Periapical Diseases
1 Pathogenesis of Pulp and Periapical Diseases CHRISTINE SEDGLEY, RENATO SILVA, AND ASHRAF F. FOUAD CHAPTER OUTLINE Histology and Physiology of Normal Dental Pulp, 1 Normal Pulp, 11 Etiology of Pulpal and Periapical Diseases, 2 Reversible Pulpitis, 11 Microbiology of Root Canal Infections, 5 Irreversible Pulpitis, 11 Endodontic Infections Are Biofilm Infections, 5 Pulp Necrosis, 12 The Microbiome of Endodontic Infections, 6 Clinical Classification of Periapical (Apical) Conditions, 13 Pulpal Diseases, 8 Nonendodontic Pathosis, 15 LEARNING OBJECTIVES After reading this chapter, the student should be able to: 6. Describe the histopathological diagnoses of periapical lesions of 1. Describe the histology and physiology of the normal dental pulpal origin. pulp. 7. Identify clinical signs and symptoms of acute apical periodon- 2. Identify etiologic factors causing pulp inflammation. titis, chronic apical periodontitis, acute and chronic apical 3. Describe the routes of entry of microorganisms to the pulp and abscesses, and condensing osteitis. periapical tissues. 8. Discuss the role of residual microorganisms and host response 4. Classify pulpal diseases and their clinical features. in the outcome of endodontic treatment. 5. Describe the clinical consequences of the spread of pulpal 9. Describe the steps involved in repair of periapical pathosis after inflammation into periapical tissues. successful root canal treatment. palisading layer that lines the walls of the pulp space, and their Histology and Physiology of Normal Dental tubules extend about two thirds of the length of the dentinal Pulp tubules. The tubules are larger at a young age and eventually become more sclerotic as the peritubular dentin becomes thicker. The dental pulp is a unique connective tissue with vascular, lym- The odontoblasts are primarily involved in production of mineral- phatic, and nervous elements that originates from neural crest ized dentin. -

Pulp Therapy for Primary and Young Permanent Teeth: Foundational Articles and Consensus Recommendations, 2021
Pulp Therapy for Primary and Young Permanent Teeth: Foundational Articles and Consensus Recommendations, 2021 Alqaderi H, Lee CT, Borzangy S, Pagonis TC. Coronal pulpotomy for cariously exposed permanent posterior teeth with closed apices: A systematic review and meta-analysis. J Dent. 2016;44:1-7. American Academy of Pediatric Dentistry. Pulp therapy for primary and immature permanent teeth. Reference Manual, 2014. Available at: https://www.aapd.org/globalassets/media/policies_guidelines/bp_pulptherapy. pdf. Accessed, March 1, 2020. Barros MMAF, De Queiroz Rodrigues M, Muniz FWMG, Rodrigues LKA. Selective, stepwise, or nonselective removal of carious tissue: which technique offers lower risk for the treatment of dental caries in permanent teeth? A systematic review and meta-analysis. Clin Oral Investig. 2020;24:521-32. Coll JA, Seale NS, Vargas K, Marghalani AA, Al Shamali S, Graham L. Primary Tooth Vital Pulp Therapy: A Systematic Review and Meta-analysis. Pediatr Dent. 2017;39:16-123. Coll JA, Vargas K, Marghalani AA, Chen CY, Alshamali S, Dhar V, Crystal Y. A Systematic Review and Meta-Analysis of Non-vital Pulp Therapy for Primary Teeth. Pediatr Dent 2020;42(4):256-272. Cushley S, Duncan HF, Lappin MJ, Tomson PL, Lundy FT, Cooper P, Clarke M, El Karim IA. Pulpotomy for mature carious teeth with symptoms of irreversible pulpitis: A systematic review. J Dent. 2019;88:103158. El Meligy OA, Allazzam S, Alamoudi NM. Comparison between biodentine and formocresol for pulpotomy of primary teeth: a randomized clinical trial. Quintessence Int. 2016;47:571‐80. Farsi DJ, El-Khodary HM, Farsi NM, El Ashiry EA, et al. -

Insight Into the Role of Dental Pulp Stem Cells in Regenerative Therapy
biology Review Insight into the Role of Dental Pulp Stem Cells in Regenerative Therapy Shinichiro Yoshida 1,* , Atsushi Tomokiyo 1 , Daigaku Hasegawa 1, Sayuri Hamano 2,3, Hideki Sugii 1 and Hidefumi Maeda 1,3 1 Department of Endodontology, Kyushu University Hospital, 3-1-1 Maidashi, Higashi-ku, Fukuoka 812-8582, Japan; [email protected] (A.T.); [email protected] (D.H.); [email protected] (H.S.); [email protected] (H.M.) 2 OBT Research Center, Faculty of Dental Science, Kyushu University, 3-1-1 Maidashi, Higashi-ku, Fukuoka 812-8582, Japan; [email protected] 3 Department of Endodontology and Operative Dentistry, Faculty of Dental Science, Kyushu University, 3-1-1 Maidashi, Higashi-ku, Fukuoka 812-8582, Japan * Correspondence: [email protected]; Tel.: +81-92-642-6432 Received: 20 May 2020; Accepted: 5 July 2020; Published: 9 July 2020 Abstract: Mesenchymal stem cells (MSCs) have the capacity for self-renewal and multilineage differentiation potential, and are considered a promising cell population for cell-based therapy and tissue regeneration. MSCs are isolated from various organs including dental pulp, which originates from cranial neural crest-derived ectomesenchyme. Recently, dental pulp stem cells (DPSCs) and stem cells from human exfoliated deciduous teeth (SHEDs) have been isolated from dental pulp tissue of adult permanent teeth and deciduous teeth, respectively. Because of their MSC-like characteristics such as high growth capacity, multipotency, expression of MSC-related markers, and immunomodulatory effects, they are suggested to be an important cell source for tissue regeneration.