Cell Injury David S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Genotoxicity and Cytotoxicity Amongst in Dental
Dental, Oral and Craniofacial Research Research Article ISSN: 2058-5314 Evaluation of genotoxicity and cytotoxicity amongst in dental surgeons and technicians by micronucleus assay Molina Noyola Leonardo Daniel1,2, Coronado Romo María Eugenia3, Vázquez Alcaraz Silverio Jafet4, Izaguirre Pérez Marian Eliza1,2, Arellano-García Evarista5, Flores-García Aurelio6 and Torres Bugarín Olivia1* 1Laboratorio de Evaluación de Genotóxicos, Programa Internacional de Medicina, Universidad Autónoma de Guadalajara, Mexico 2Facultad de Medicina, Universidad Autónoma de Guadalajara, Mexico 3Departamento de Ortodoncia, Facultad de Odontología, Universidad Autónoma de Guadalajara, Mexico 4Departamento de Endodoncia, Facultad de Odontología, Universidad Autónoma de Guadalajara, Mexico 5Facultad de Ciencias, Universidad Autónoma de Baja California, Mexico 6Unidad Académica de Medicina, Universidad Autónoma de Nayarit, Tepic, Nayarit, Mexico Abstract Introduction: Dental surgeons and technicians are continuously exposed to agents could be affect the genetic material and induce mutations. The aim of this study was to evaluate the genotoxic and cytotoxic occupational risk of dental surgeons and technicians through the micronucleated cells (MNC) and nuclear abnormalities (NA) assay in oral mucosa. Methods: Case-control study. We have collected a buccal mucosa from dental surgeons, dental technicians and healthy individuals (matched by BMI, age and gender). The smears were fixed (ethanol 80%/48 h), stained (orange acridine) and analyzed (microscope, 100×). The frequency of MNC and NA (binucleated cells [BNC], lobulated nucleus [LN], condensed chromatins [CC], karyorrhexis [KR], pyknosis (PN) and karyolysis [KL] were counted in 2,000 cells per participant. Results: 90 samples were collected (26 surgeons, 19 technicians and 45 controls). Compared with controls, exception of PN, in surgeons was higher frequency and positive association of MNC and all NA (p<0.05). -

In Partial Fulfilment of Requirements for the Degree Of
THE EFFECTS OF FEED-BORNE FUSARIUM MYCOTOXINS ON THE PERFORMANCE AND HEALTH OF RAINBOW TROUT (ONCORHYNCHUS MYKISS) A Thesis Presented to The Faculty of Graduate Studies of The University of Guelph by JAMIE MARIE HOOFT In partial fulfilment of requirements for the degree of Master of Science May, 2010 © Jamie M. Hooft, 2010 Library and Archives Bibliothèque et 1*1 Canada Archives Canada Published Heritage Direction du Branch Patrimoine de l'édition 395 Wellington Street 395, rue Wellington Ottawa ON K1A 0N4 Ottawa ON K1A 0N4 Canada Canada Your file Votre référence ISBN: 978-0-494-67487-1 Our file Notre référence ISBN: 978-0-494-67487-1 NOTICE: AVIS: The author has granted a non- L'auteur a accordé une licence non exclusive exclusive license allowing Library and permettant à la Bibliothèque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par télécommunication ou par l'Internet, prêter, telecommunication or on the Internet, distribuer et vendre des thèses partout dans le loan, distribute and sell theses monde, à des fins commerciales ou autres, sur worldwide, for commercial or non- support microforme, papier, électronique et/ou commercial purposes, in microform, autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriété du droit d'auteur ownership and moral rights in this et des droits moraux qui protège cette thèse. Ni thesis. Neither the thesis nor la thèse ni des extraits substantiels de celle-ci substantial extracts from it may be ne doivent être imprimés ou autrement printed or otherwise reproduced reproduits sans son autorisation. -

71182407Ad80c7abf430b599eb
Journal name: International Journal of Nanomedicine Article Designation: Original Research Year: 2017 Volume: 12 International Journal of Nanomedicine Dovepress Running head verso: Yang et al Running head recto: HA-SPIONs for effective cancer diagnosis and treatment open access to scientific and medical research DOI: http://dx.doi.org/10.2147/IJN.S121249 Open Access Full Text Article ORIGINAL RESEARCH Hyaluronan-modified superparamagnetic iron oxide nanoparticles for bimodal breast cancer imaging and photothermal therapy Rui-Meng Yang1,* Abstract: Theranostic nanoparticles with both imaging and therapeutic abilities are highly Chao-Ping Fu2,* promising in successful diagnosis and treatment of the most devastating cancers. In this study, Jin-Zhi Fang1 the dual-modal imaging and photothermal effect of hyaluronan (HA)-modified superparamag- Xiang-Dong Xu1 netic iron oxide nanoparticles (HA-SPIONs), which was developed in a previous study, were Xin-Hua Wei1 investigated for CD44 HA receptor-overexpressing breast cancer in both in vitro and in vivo Wen-Jie Tang1 experiments. Heat is found to be rapidly generated by near-infrared laser range irradiation of HA- SPIONs. When incubated with CD44 HA receptor-overexpressing MDA-MB-231 cells in vitro, Xin-Qing Jiang1 HA-SPIONs exhibited significant specific cellular uptake and specific accumulation confirmed Li-Ming Zhang2 by Prussian blue staining. The in vitro and in vivo results of magnetic resonance imaging and 1Department of Radiology, Guangzhou photothermal ablation demonstrated that HA-SPIONs exhibited significant negative contrast First People’s Hospital, Guangzhou enhancement on T -weighted magnetic resonance imaging and photothermal effect targeted Medical University, 2School of 2 Materials Science and Engineering, CD44 HA receptor-overexpressing breast cancer. -

DUKE UNIVERSITY School of Medicine Pathologists' Assistant
DUKE UNIVERSITY School of Medicine Pathologists’ Assistant Program Department of Pathology Academic Programs The Department of Pathology at Duke University offers a wide array of training programs to fit individual requirements and goals. The Residency Training program is an ACGME approved program and is available as an Anatomic Pathology/Clinical Pathology combined program, a shorter Anatomic Pathology only program, or an Anatomic Pathology/Neuropathology program. Subspecialty fellowships in Cytopathology, Dermatopathology, Hematopathology, Medical Microbiology, and Neuropathology are also ACGME approved. These programs provide the highest quality of graduate medical education by drawing on the depth and breadth of faculty expertise in the Department in all aspects of anatomic and clinical pathology and the availability of a wide variety of often complex clinical cases seen at Duke University Health System. For medical students interested in a career in Pathology pre-doctoral fellowships, internships and externships are available. Research Training in Experimental pathology can be obtained through Pre- and postdoctoral fellowships of one to five years. All pre-doctoral fellows are candidates for the Ph.D. degree in pathology. The Ph.D. is optional in postdoctoral programs, which provide didactic and research training in various aspects of modern experimental pathology. A two year NAACLS accredited Pathologists’ Assistant Program leads to a Master of Health Science degree, certifies graduates to sit for the ASCP Board of Certification examination, and leads to exciting career opportunities in a variety of anatomic pathology laboratory settings. Pathologists’ assistants are analogous to physician assistants, but with highly specialized training in autopsy and surgical pathology. This profession was pioneered in the Duke Department of Pathology 50 years ago, and is one of only twelve such programs in existence today. -

1 Pathology Week 1 – Cellular Adaptation, Injury and Death
Pathology week 1 – Cellular adaptation, injury and death Cellular responses to injury Cellular Responses to Injury Nature and Severity of Injurious Stimulus Cellular Response Altered physiologic stimuli: Cellular adaptations: • ↑demand, ↑ trophic stimulation (e.g. growth factors, hormones) • Hyperplasia, hypertrophy • ↓ nutrients, stimulation • Atrophy • Chronic irritation (chemical or physical) • Metaplasia Reduced oxygen supply; chemical injury; microbial infection Cell injury: • Acute and self-limited • Acute reversible injury • Progessive and severe (including DNA damage) • Irreversible injury → cell death Necrosis Apoptosis • Mild chronic injury • Subcellular alterations in organelles Metabolic alterations, genetic or acquired Intracell accumulations; calcifications Prolonged life span with cumulative sublethal injury Cellular aging Hyperplasia - response to increased demand and external stimulation - ↑ number cells - ↑ volume of organ - often occurs with hypertrophy - occurs if cells able to synthesize DNA – mitotic division - physiologic or pathologic Physiological hyperplasia A) hormonal – ↑ functional capacity tissue when needed (breast in puberty, uterus in pregnancy) B) compensatory - ↑ tissue mass after damage/resection (post-nephrectomy) Mechanisms: - ↑ local production growth factors or activation intracellular signaling pathways o both → production transcription factors that turn on cellular genes incl those encoding growth factors, receptors for GFs, cell cycle regulators →→ cellular proli feration - in hormonal hyperplasia -

Cytology of Inflammation
Association of Avian Veterinarians Australasian Committee Ltd. Annual Conference Proceedings Auckland New Zealand 2017 25: 20-30 Cytology of Inflammation Terry W. Campbell MS, DVM, PhD, Emeritus Department of Clinical Sciences College of Veterinary Medicine and Biomedical Sciences Colorado State University 300 West Drake Road Fort Collins, Colorado, USA The inflammatory response of birds can be classified as a mixed cell inflammation, the most common cellular in- either heterophilic, eosinophilic (rarely reported as they flammatory response seen in birds. They can develop into may be difficult to detect with routine staining), mixed epithelioid and multinucleated giant cells. As the inflam- cell, or macrophagic (histiocytic) depending upon the pre- matory process continues and becomes chronic, granu- dominant cell type. Inflammatory cells arrive at the lesion lomas may develop as the macrophages form into layers by active migration in response to various chemotactic that resemble epithelium and this is the reason for the factors, and the type of inflammatory response present term “epithelioid cells.” As the lesion matures, fibroblasts may suggest a possible aetiology and pathogenesis. proliferate and begin to lay down collagen. These prolif- erating fibroblasts appear large compared to the small Heterophilic Inflammation of Birds densely staining fibroblasts of normal fibrous tissue. Lym- phocytes appear within the stroma and participate in the Inflammation occurs whenever chemotactic factors for cell-mediated immune response. Fusion of macrophages inflammatory cells are released. The most common caus- into giant cells occurs in association with material that is es are microbes and their toxins, physical and chemical not readily digested by macrophages. The results of acute trauma, death of cells from circulatory insufficiency, and inflammation may be complete resolution, development immune reactions. -

Anal Cytology in Women with Cervical Intraepithelial Or Invasive Cancer
ORIGINAL ARTICLE J Bras Patol Med Lab, v. 51, n. 5, p. 315-322, October 2015 Anal cytology in women with cervical intraepithelial or invasive cancer: interobserver agreement Citologia anal em mulheres com neoplasia intraepitelial ou invasiva cervical: concordância interobservadores 10.5935/1676-2444.20150051 Sandra A. Heráclio1; Fátima Regina G. Pinto2; Kristiane Cahen2; Letícia Katz2; Alex Sandro R. Souza1, 3 1. Instituto de Medicina Integral Professor Fernando Figueira (Imip). 2. Laboratório Central de Saúde Pública de Pernambuco (Lacen-PE). 3. Universidade Federal de Pernambuco (UFPE). ABSTRACT Introduction: Incidence rates of anal cancer have been rising worldwide in the last 20 years. Due to embryological, histological and immunohistochemical similarities between the anal canal and the cervix, routine screening with anal cytology for precursor lesions in high-risk groups has been adopted. Objective: To determine interobserver agreement for the diagnosis of anal neoplasia by anal cytology. Material and methods: A cross-sectional observational study was conducted in 324 women with cervical intraepithelial or invasive cancers, for screening of anal cancer, from December 2008 to June 2009. Three hundred twenty-four cytological samples were analyzed by three cytopathologists. Cytological evaluation was based on the revised Bethesda terminology; samples were also classified into negative and positive for atypical cells. We calculated the kappa statistic with 95% confidence interval (95% CI) to assess agreement among the three cytopathologists. Results: Interobserver agreement in the five categories of the Bethesda terminology was moderate (kappa for multiple raters: 0.6). Agreement among cytopathologists 1, 2 and 3 with a consensus diagnosis was strong (kappa: 0.71, 0.85 and 0.82, respectively). -

Department of Experimental Pathology, Immunology and Microbiology 531
Department of Experimental Pathology, Immunology and Microbiology 531 Department of Experimental Pathology, Immunology and Microbiology Interim Chairperson: Zaatari, Ghazi Vice Chairperson: Matar, Ghassan Professors: Abdelnoor, Alexander; Khouri, Samia; Matar, Ghassan; Sayegh, Mohamed; Zaatari, Ghazi Associate Professor: Rahal, Elias Assistant Professors: Al-Awar, Ghassan; El Hajj, Hiba; Shirinian, Margret; Zaraket, Hassan The Department of Experimental Pathology, Immunology and Microbiology offers courses to medical laboratory sciences (MLSP) students as well as nursing, medical, and graduate students. It offers a graduate program (discipline of Microbiology and Immunology) leading to a master’s degree (MS) or doctoral degree (PhD) in Biomedical sciences. The requirements for admission to the graduate program are stated on page 33 of this catalogue. IDTH 203 The immune System in Health and Disease 37.28; 3 cr. See Interdepartmental Courses. IDTH 205 Microbiology and Infectious Diseases 37.28; 5 cr. See Interdepartmental Courses. MBIM 223 Parasitology for MLSP Students 39.39; 4 cr. Second semester. MBIM 237 Microbiology and Immunology for Nursing Degree Students 32.64; 3 cr. A course on the fundamental aspects of medical microbiology and immunology for nursing students. Second semester. MBIM 260 Elective in Infectious Diseases for Medicine III and IV 0.180 A course on basic evaluation, diagnosis, and management of infectious diseases. One month. MBIM 261 Elective in Immunology for Medicine III and IV 0.180 A course that is an introduction to immunological research and its application to clinical practice. One month. MBIM 310 Basic Immunology 32.32; 3 cr. A course on innate and adaptive immune mechanisms, infection and immunity, vaccination, immune mechanisms in tissue injury and therapeutic immunology. -
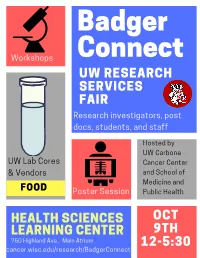
Badgerconnect 2019 Program
Badger Connect Workshops UW RESEARCH SERVICES FAIR Research investigators, post docs, students, and staff Hosted by UW Carbone UW Lab Cores Cancer Center & Vendors and School of Medicine and FOOD Poster Session Public Health HEALTH SCIENCES OCT LEARNING CENTER 9TH 750 Highland Ave., Main Atrium 12-5:30 cancer.wisc.edu/research/BadgerConnect BadgerConnect Research Services Fair October 9th, 2019 12:00 – 5:30 PM, HSLC Atrium AGENDA 12:00 – 12:30pm Registration / Networking Registration table and networking at booths open at 12pm 12:30 – 2:00pm Flash Talks Lunch (Rm 1306 HSLC) ~4 minute flash talks by research services throughout lunch 15’ Break/Networking 2:15 – 2:45pm Workshop Session I Rm 1220 HSLC Rm 1222 HSLC Rm 1244 HSLC Reference Grade De Novo Assemblies and Whole Team Science 101: How to How to create a tissue Topic Transcriptomes: See the Big build, lead, and manage a microarray (TMA) Picture With Pacbio SMRT team that does great science Sequencing UW Translational Research Biotechnology Center DNA Team Science - ICTR and Service Initiatives in Pathology Lab Sequencing Facility UWCCC Vendor n/a Pacific Biosciences n/a 15’ Break/Networking 3:00 – 3:30pm Workshop Session II Rm 1220 HSLC Rm 1222 HSLC Rm 1244 HSLC LabArchives: The Electronic Hyperfinder: Computational Creating Novel Disease Models Topic Lab Notebook Service for Sorting for High-Dimensional with CRISPR Campus Flow Cytometry Data UW Genome Editing and Animal Electronic Lab Notebook Flow Cytometry Lab Service Models Core Service Integrated DNA Technologies, Vendor LabArchives -

Overview of Pathology and Its Related Disciplines - Soheir Mahmoud Mahfouz
MEDICAL SCIENCES – Vol.I -Overview of Pathology and its Related Disciplines - Soheir Mahmoud Mahfouz OVERVIEW OF PATHOLOGY AND ITS RELATED DISCIPLINES Soheir Mahmoud Mahfouz Cairo University, Kasr El Ainy Hospital, Egypt Keywords: Pathology, Pathology disciplines, Pathology techniques, Ancillary diagnostic methods, General Pathology, Special Pathology Contents 1. Introduction 1.1 Pathology coverage 1.1.1 Etiology and Pathogenesis of a Disease 1.1.2 Manifestations of Disease (Lesions) 1.1.3 Phases Of A Disease Process (Course) 1.2 Physician’s approach to patient 1.3 Types of pathologists and affiliated specialties 1.4 Role of pathologist 2. Pathology and its related disciplines 2.1 Cytology 2.1.1 Cytology Samples 2.1.2 Technical Aspects 2.1.3 Examination of Sample and Diagnosis 3. Pathology techniques and ancillary diagnostic methods 3.1 Macroscopic pathology 3.2 Light Microscopy 3.3 Polarizing light microscopy 3.4 Electron microscopy (EM) 3.5 Confocal Microscopy 3.6 Frozen section 3.7 Cyto/histochemistry 3.8 Immunocyto/histochemical methods 3.9 Molecular and genetic methods of diagnosis 3.10 Quantitative methods 4. Types of tests used in pathology 4.1 DiagnosticUNESCO tests – EOLSS 4.2 Quantitative tests 4.3 Prognostic tests 5. The scope of SAMPLEpathology & its main divisions CHAPTERS 6. Conclusions Glossary Bibliography Biographical sketch Summary Pathology is the science of disease. It deals with deviations from normal body function and ©Encyclopedia of Life Support Systems (EOLSS) MEDICAL SCIENCES – Vol.I -Overview of Pathology and its Related Disciplines - Soheir Mahmoud Mahfouz structure. Many disciplines are involved in the study of disease, as it is necessary to understand the complex causes and effects of various disorders that affect the organs and body as a whole. -

MEDICAL UNIVERSITY of SOUTH CAROLINA Charleston, SC
MEDICAL UNIVERSITY OF SOUTH CAROLINA Charleston, SC PROGRAMS OFFERED The Department of Pathology and Laboratory Medicine of the Medical University of South Carolina offers a fully accredited training program in anatomic and clinical pathology (AP/CP). The AP/CP program consists of a 39 month core curriculum with 9 months of elective. Anatomic Pathology core rotations include autopsy pathology/forensic pathology, surgical pathology, cytopathology, dermatopathology and VA pathology. Clinical Pathology core rotations include hematopathology, immunopathology, clinical chemistry, microbiology, tranfusion medicine, apheresis, histocompatibility laboratory, molecular pathology, cytogenetics, VA pathology, laboratory management and informatics. Nine months elective time is available for more in-depth studies in areas of special interest and/or research. A graduate (PhD) program in experimental pathology is available and may be coordinated with the residency training program. Fellowships are offered at the discretion of the Chair in forensic pathology, dermatopathology, cytopathology, surgical pathology, gastrointestinal pathology, hematopathology and clinical chemistry. TYPES AND NUMBERS OF APPOINTMENTS The institution is accredited for twenty-two residency positions in anatomic pathology and clinical pathology, with an even distribution of residents at all levels. Persons seeking the PhD degree in experimental pathology must meet the requirements of the College of Graduate Studies, Medical University of South Carolina. The department participates -

MCQ-PG Entrance -AGADTANTRA Maitm Ca Maaohyaot \...Mama-B
BV(DU) COLLEGE OF AYURVED, PUNE-411043 (MH- INDIA) MCQ-PG Entrance -AGADTANTRA 1 maitM ca maaohyaot\...mama-banQaana\ iCnnait ca ÈÈ A) raOxyaat \ B) saaOxmyaat\ tOxNyaat\ AaOYNyaat C) D) 2 ivaYaM ca vaRQdyao …… A) GaRtM B) tOlaM vasaaM xaaOd`M C) D) 3. ……garsaM&M tu ik`yato ivaivaQaaOYaQaOÁ ÈÈ A) kRi~maM B) sqaavarM jaMgamaM dUiYatM C) D) 4. garo…… È A) GaRtM B) tama`M xaaOd`M homaÁ C) D) 5. ….vas~oYau Sayyaasau kvacaaBarNaoYau ca È A) pRYzoYau B) s~xau AnyaoYau padpIzoYau C) D) 6. vaIyaa-lpBaavaanna inapatyaot\ tt\ ……. vaYa-gaNaanaubainQa È A) iptavaR%tM B) vaatavaR%tM kfavaR%tM maodaovaR%tM C) D) 7. According to Sushruta, Sthavar visha adhisthana are …. in number. A) 16 B) 10 C) 8 D) 13 8. According to Sushruta, Jangam visha adhisthana are …. in number. A) 10 B) 12 C) 16 D) 14 Bharati Vidyapeeth (Deemed to be University) College of Ayurved, Pune. Tel.: 20-24373954; Email- [email protected]; Website:-www.coayurved.bharatividyapeeth.edu 9. …… is one of the ingredients of dooshivishari Agad. A) Mamsi B) Amruta C) Shunthi D) Triphala 10. Which of the following yog is used for the treatment of garopahat pawak? A) Dooshivishari B) Moorvadi C) Eladi D) Panchashirisha 11. Tobacco is……poison. A) Corrosive B) somniferous C) cardiac D) spinal 12. Which of the following is a spinal stimulant poison? A) Ahifen B) Kuchala C) Vatsanabh D) Arka 13. ivaYasaMk`maNaaqa-M mastko BaoYajadanama\ [it……… È A) ]paQaanama \ B) AirYTma\ inaYpIDnama\ pirYaokma\ C) D) 14. Which of the following dravya is not used for hrudayavaran? A) Gomay ras B) Kshaudra C) Supakwa Ekshu D) Mudgayusha 15.