Developmental Structural Tooth Defects in Dogs – Experience from Veterinary Dental Referral Practice and Review of the Literature
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

ADEA Compendium of Curriculum Guidelines Allied Dental Education
ADEA Compendium of Curriculum Guidelines (Revised Edition) Allied Dental Education Programs May 2015–2016 ADEA Compendium of Curriculum Guidelines for Allied Dental Education Programs May 2015–2016 CONTENTS INTRODUCTION .................................................................................................. 2 ACKNOWLEDGEMENTS ...................................................................................... 5 DENTAL HYGIENE CURRICULUM GUIDELINES ................................................... 8 Clinical and Preclinical Dental Hygiene ........................................................... 8 Community Dental Health ............................................................................. 21 Dental Materials ............................................................................................ 31 Medical Emergencies .................................................................................... 53 Nutrition ........................................................................................................ 60 Oral Anatomy and Histo-embryology ............................................................ 70 Oral Pathology............................................................................................... 97 Periodontology ............................................................................................ 109 Pharmacology .............................................................................................. 125 Research for Dental Hygiene Education ..................................................... -

Free PDF Download
Eur opean Rev iew for Med ical and Pharmacol ogical Sci ences 2014; 18: 440-444 Radiographic evaluation of the prevalence of enamel pearls in a sample adult dental population H. ÇOLAK, M.M. HAMIDI, R. UZGUR 1, E. ERCAN, M. TURKAL 1 Department of Restorative Dentistry, Kirikkale University School of Dentistry, Kirikkale, Turkey 1Department of Prosthodontics, Kirikkale University School of Dentistry, Kirikkale, Turkey Abstract. – AIM: Enamel pearls are a tooth One theory of the enamel pearl etiology is that anomaly that can act as contributing factors in the enamel pearls develop as a result of a localized development of periodontal disease. Studies that developmental activity of a remnant of Hertwig’s have addressed the prevalence of enamel pearls in epithelial root sheath which has remained adher - populations were scarce. The purpose of this study 5 was to evaluate the prevalence of enamel pearls in ent to the root surface during root development . the permanent dentition of Turkish dental patients It is believed that cells differentiate into function - by means of panoramic radiographs. ing ameloblasts and produce enamel deposits on PATIENTS AND METHODS: Panoramic radi - the root. The conditions needed for local differ - ographs of 6912 patients were examined for the entiation and functioning of ameloblasts in this presence of enamel pearls. All data (age, sex and ectopic position are not fully understood 6,7 . systemic disease or syndrome) were obtained from the patient files and analyzed for enamel The most common site for enamel pearls is at pearls. Descriptive characteristics of sexes, the cementoenamel junction of multirooted jaws, and dental localization were recorded. -

COMPENDIUM of CURRICULUM GUIDELINES (Revised Edition)
COMPENDIUM OF CURRICULUM GUIDELINES (Revised Edition) ALLIED DENTAL EDUCATION PROGRAMS February 2005 TABLE OF CONTENTS Introduction…………………………………………………………………………….3 Acknowledgments…………………………………………………………………….6 DENTAL HYGIENE CURRICULUM GUIDELINES Clinical Dental Hygiene……………………………………………………………...10 Community Dental Health…………………………………………………………...21 Dental Materials……………………………………………………………………….28 Medical Emergencies……………………………………………………………….. 49 Nutrition……………………………………………………………………………….. 55 Oral and Facial Anatomy…………………………………………………………….65 Oral Pathology…………………………………………………………………………88 Periodontology……………………………………………………………..................98 Pharmacology…………………………………………………………………………110 Research………………………………………………………………………………..123 Special Needs Patients………………………………………………………………129 DENTAL ASSISTING CURRICULUM GUIDELINES Pathology……………………………………………………………………………….137 Preclinical Dental Assisting…………………………………………………………145 DENTAL HYGIENE AND DENTAL ASSISTING CURRICULUM GUIDELINES Dental Radiography……………………………………………………………………152 Radiation Use Guidelines……………………………………………………………..173 Clinical Radiology………………………………………………………………………178 Ethics and Professionalism…………………………………………………………..184 2 INTRODUCTION This document is a revision of curriculum guidelines that were developed for allied dental education programs between 1984 and 1994. It does not include all content areas that could be found in an allied dental education program. Most of the guidelines are for dental hygiene with some for dental assisting. Unfortunately, no guidelines were developed during this time -

Poster Communications
1113-5181/19/27.1/94-120 ODONTOLOGÍA PEDIÁTRICA ODONTOL PEDIÁTR (Madrid) COPYRIGHT © 2019 SEOP Y ARÁN EDICIONES, S. L. Vol. 27, N.º 1, pp. 94-120, 2019 Poster communications RESEARCH STUDIES 10. CHANGES IN ORAL HEALTH-RELATED QUALITY OF LIFE WHEN ASSOCIATED WITH THE TYPE OF CLEFT LIP AND/OR PALATE IN SURGICALLY TREATED CHILDREN 8. EFFECT OF INHALED MEDICATION ON THE López Ramos, R.P.1; Abanto, J.2; Blanco, D.3; Torres, ORAL HEALTH OF ASTHMATIC PATIENTS G.4; Pajuelo, M.3 1 1 2 3 4 Faculty of Public Health and Administration. Peruvian Pinto, V. ; Menor, A. ; Gallegos, L. ; Martínez, E. 2 1Clínica Pinto. Burgos. 2Centro de Salud de Coria. Cáceres. University of Cayetano Heredia. Lima, Peru. Department 3 4 of Pediatric Dentistry. University of São Paulo. São Alfonso X El Sabio University. Madrid. Complutense 3 University of Madrid. Madrid Paulo, Brasil. Faculy of Sciences and Philosophy. Peruvian University Cayetano Heredia. Lima, Peru. 4 Introduction and objectives: Currently, and with increasing Postgraduate course on Pediatric Dentistry. Faculty of frequency, respiratory disorders are affecting a large percen- Pediatric Dentistry. National University of San Marcos. tage of the child population. The literature reviewed in this Lima, Peru research project shows that the use of inhaled medication for respiratory conditions is related to adverse reactions such as Introduction and objectives: The most common cranio- erosion, dental caries, gingivitis, halitosis or xerostomia. The facial malformation in children is the cleft lip and/or palate objective of the present study was to evaluate the relations- and the treatment is multidisciplinary. -
Developmental Disturbances Affecting Teeth
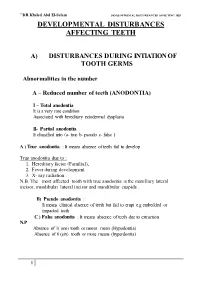
``DR.Khaled Abd El-Salam DEVELO PMENTAL DISTURBANCES AFFECTING TEET DEVELOPMENTAL DISTURBANCES AFFECTING TEETH A) DISTURBANCES DURING INTIATION OF TOOTH GERMS Abnormalities in the number A – Reduced number of teeth (ANODONTIA) I – Total anodontia It is a very rare condition Associated with hereditary ectodermal dysplasia II- Partial anodontia It classified into (a- true b- pseudo c- false ) A ) True anodontia : It means absence of teeth fail to develop True anodontia due to : 1. Hereditary factor (Familial), 2. Fever during development. 3. X- ray radiation . N.B. The most affected tooth with true anodontia is the maxillary lateral incisor, mandibular lateral incisor and mandibular cuspids . B) Pseudo anodontia : It means clinical absence of teeth but fail to erupt e.g embedded or impacted teeth C ) False anodontia : It means absence of teeth due to extraction N.P Absence of 1( one) tooth or mores mean (Hypodontia) Absence of 6 (six) tooth or more means (hyperdontia) 1 ``DR.Khaled Abd El-Salam DEVELO PMENTAL DISTURBANCES AFFECTING TEET ECTODERMAL DYSPLASIA • It is a hereditary disease which involves all structures which are derived from the ectoderm . • It is characterized by (general manifestation) : 1- Skin ( thin, smooth, Dry skin) 2- Hair (Absence or reduction (hypotrichosis). 3- Sweat-gland (Absence anhydrosis). 4- sebaceous gland ( absent lead to dry skin) 5-Temperature elevation (because of anhydrosis) 6- Depressed bridge of the nose 7- Defective mental development 8- Defective of finger nail Oral manifestation include teeth and -

TV's COMPLIED NDBE QUESTIONS 2013‐2015
TV’s COMPLIED NDBE QUESTIONS 2013‐2015 https://quizlet.com/87020251/stuff‐to‐remember‐flash‐cards/ Compiled + 2015 + notes = purple + Highlighted FUNGI *A chlamydospore is the thick‐walled big resting spore of several kinds of fungi, including Ascomycota such as Candida and Basidiomycota such as Panus. It is the life‐stage which survives in unfavourable conditions, such as dry or hot seasons. 1. Organisms that exhibit dimorphism and grow on Sabouraud's medium (low pH): Fungi 2. Type of agar used for most fungi? Sabouraud agar 3. Organism that causes athletes foot (tinea pedis) Trichophyton 4. Which fungal infection leads to superficial skin disease? Trichophyton ‐ Epidermophyton & Microsporum cause dermatophytosis. Tx w/ Griseofulvin 5. Which fungus causes cerebral/brain infarct? a. Cryptococcus may spread into the meninges and cause Cryptococcal Meningitis b. Aspergillus causes aspergilloma “fungus ball” in the lungs causing pulmonary infection in ppl with AIDS or have undergone organ transplant c. Mucormycosis Pt’s w/ diabetic ketoacidosis, burns, or leukemia are particularly susceptible. It results in black, dead tissue in the nasal cavity and blocks the blood supply to the brain. ‐ Mucormycosis is found in blood vessels (endothelium) & is often related to diabetic pts 6. Aflatoxin is what produced by what fungus? Aspergillus 7. Cell immunity is most important for? Intracellular parasiteow 8. Which one can be seen as an intracellular organism? Histoplasmosis ‐ In infected tissues, yeast cells of Histoplasmosis are found within macrophages. 9. Disseminated fungi? Histoplasmosis (infection by a fungus found in the droppings of birds and bats in humid areas. It is not serious if confined to the lungs but can be fatal if spread throughout the body) 10. -

A Global Compendium of Oral Health
A Global Compendium of Oral Health A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan This book first published 2019 Cambridge Scholars Publishing Lady Stephenson Library, Newcastle upon Tyne, NE6 2PA, UK British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Copyright © 2019 by Morenike Oluwatoyin Folayan and contributors All rights for this book reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner. ISBN (10): 1-5275-3691-2 ISBN (13): 978-1-5275-3691-3 TABLE OF CONTENTS Foreword .................................................................................................. viii Introduction ................................................................................................. 1 Dental Development: Anthropological Perspectives ................................. 31 Temitope A. Esan and Lynne A. Schepartz Belarus ....................................................................................................... 48 Natallia Shakavets, Alexander Yatzuk, Klavdia Gorbacheva and Nadezhda Chernyavskaya Bangladesh ............................................................................................... -

Journal of Science / Vol 8 / Issue 1 / 2018 / 19-25
Monika Rohilla. / Journal of Science / Vol 8 / Issue 1 / 2018 / 19-25. e ISSN 2277 - 3290 Print ISSN 2277 - 3282 Journal of Science Microbiology www.journalofscience.net Research article DISTURBANCES DURING APPOSITION OF DENTAL HARD TISSUES Monika Rohilla* PG Demonstrator in the Department of Pedodontics, PGIDS, Rohtak, Haryana 124514, India. ABSTRACT A series of factors influence the normal development of the occlusion, interfering in correct alignment of the teeth and harmonic relationship with the adjacent and antagonistic elements. Developmental disturbances of the teeth may manifest by variations in number, position, size, shape, eruption, structure. Such disturbances may occur in association with some more generalised disorder or may occur independently. The present study is undertaken to review the etiopathogenesis of various developmental disturbances during apposition of dental hard tissues. Keywords: Development, Hypoplasia, Apposition. Access this article online mutations in the AMEL-X gene which codes for Home page: Quick Response ameloblastin, enamelin, or tuftelin. In the case of http://journalofscience.net// code autosomal dominant type, the locus of defective gene is on chromosome 4q21 to which enamelin maps. The most DOI: common X-linked types are caused by a variety of defects http://dx.doi.org/10.21276/jos.2018.8.1.5 in the amelogenin genes and confusingly, it seems the same mutation can sometimes cause hypoplastic, Received:16.11.17 Revised:28.11.17 Accepted:06.12.17 hypomineralisation, or hypomaturation forms in different patients [2]. If there is disturbance of the first phase in which the Corresponding Author matrix is being formed the result is enamel hypoplasia Monika Rohilla and if it occurs during the second phase then the quality is PG demonstrator in the department of pedodontics, PGIDS, Rohtak, affected resulting in enamel hypomineralisation. -

Description Concept ID Synonyms Definition
Description Concept ID Synonyms Definition Category ABNORMALITIES OF TEETH 426390 Subcategory Cementum Defect 399115 Cementum aplasia 346218 Absence or paucity of cellular cementum (seen in hypophosphatasia) Cementum hypoplasia 180000 Hypocementosis Disturbance in structure of cementum, often seen in Juvenile periodontitis Florid cemento-osseous dysplasia 958771 Familial multiple cementoma; Florid osseous dysplasia Diffuse, multifocal cementosseous dysplasia Hypercementosis (Cementation 901056 Cementation hyperplasia; Cementosis; Cementum An idiopathic, non-neoplastic condition characterized by the excessive hyperplasia) hyperplasia buildup of normal cementum (calcified tissue) on the roots of one or more teeth Hypophosphatasia 976620 Hypophosphatasia mild; Phosphoethanol-aminuria Cementum defect; Autosomal recessive hereditary disease characterized by deficiency of alkaline phosphatase Odontohypophosphatasia 976622 Hypophosphatasia in which dental findings are the predominant manifestations of the disease Pulp sclerosis 179199 Dentin sclerosis Dentinal reaction to aging OR mild irritation Subcategory Dentin Defect 515523 Dentinogenesis imperfecta (Shell Teeth) 856459 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield I 977473 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; Autosomal dominant genetic disorder of tooth development Dentinogenesis Imperfecta - Shield II 976722 Dentin, Hereditary Opalescent; Shell Teeth Dentin Defect; -

DAPA 741 Oral Pathology Examination 4 December 6, 2000 1
Name: _____________________ DAPA 741 Oral Pathology Examination 4 December 6, 2000 1. Irregularity of the temporomandibular joint surfaces is a radiographic feature of A. Subluxation B. Osteoarthritis C. Trigeminal neuralgia D. Anterior disk displacement 2. Which of the following is an autoimmune disease? A. Bell’s palsy B. Osteoarthritis C. Rheumatoid arthritis D. Trigeminal neuralgia 3. Which joints are commonly affected in osteoarthritis but usually spared in rheumatoid arthritis? A. Hips B. Joints of the hands C. Knees D. Temporomandibular joint 4. Bell’s palsy may be induced by trauma to which nerve? A. Trigeminal nerve B. Glossopharyngeal nerve C. Facial nerve D. Inferior alveolar nerve 5. A patient presents to your office concerned about a painless click when she open her mouth. Your examination of her temporomandibular joint reveals a click at approximately 15 mm of opening. You instruct her to touch the incisal edges of her maxillary and mandibular anterior teeth together and then open from this position. The click disappears when she opens from this position. You diagnosis is A. Subluxation B. Anterior disk displacement C. Crepitus D. Inflammatory arthralgia 6. An ankylosed joint will cause the mandible to deviate to which side on opening? A. The affected side B. The unaffected side C. There would be no deviation on opening 7. Pain from which of the following commonly awakens the patient at night? A. Masticatory myofascial pain B. Tension headaches C. Trigeminal neuralgia D. Osteoarthritis 8. Which of the following disorders may result in blindness and is thus considered an acute ocular emergency? A. Trigeminal neuralgia B. -

Prevalence and Distribution of Dental Anomalies in a Paediatric
Prevalence and distribution of dental V.P. Wagner1, T. Arrué2, E. Hilgert2, N. A. Arús3, H. L. D. da Silveira3, anomalies in a paediatric M. D. Martins4, J. A. Rodrigues2 1Academic Unit of Oral and Maxillofacial Pathology, School of Clinical Dentistry - population based on University of Sheffield, UK 2Paediatric Dentistry Division, School of Dentistry, Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil panoramic radiographs 3Oral Radiology Division, School of Dentistry, Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil 4Oral Pathology Division, School of Dentistry, analysis Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil DOI 10.23804/ejpd.2020.21.04.7 e-mail: [email protected] Abstract considered to be the main aetiological factors. Variations in the dental morphology and structure, for example, typically result from disturbances during embryological development. Aim To evaluate the frequency and distribution of dental Nevertheless, environmental factors that occur during the anomalies (DA) in a paediatric population. prenatal and postnatal development period can also trigger the Material and methods Panoramic digital radiographs of children between 6 and 12 years old performed at a reference centre development of DA, particularly positional abnormalities or for radiographic exams were accessed. Two calibrated examiners disorders in the eruption chronology [Vani et al., 2016; Laganà evaluated the radiographs. The association between variables and et al., 2017]. The identification of DA is important once they outcomes was assessed using non-parametric tests. The significance can cause disturbances such as malocclusion, increased level was set at 5%. susceptibility to caries and aesthetic issues [Mukhopadhyay and Results Five hundred and twelve individuals were included Mitra, 2014].