Expert Panel to Review Helicopter Utilization and Protocols in Maryland
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Functions and Costs of Law Enforcement Aviation Units
The functions and costs of law enforcement aviation units Lynn Langton Statistician Bureau of Justice Statistics Why study law enforcement aviation units? • Advantages of airborne policing – Able to cover distances faster- often 1st on scene – Greater visual range from the sky – Can cover otherwise impassible areas – Officers removed from dangers on the ground – Potential deterrent effect from aircraft patrols – Able to perform routine homeland security critical facility checks • Major drawbacks – Helicopters/planes are expensive to obtain & operate – Helicopters generate substantial noise – Aerial patrol & surveillance viewed as obtrusive – Safety concerns Prior research on law enforcement aviation units • Schnelle et al. 1978 – Examination of the deterrent effect of helicopter patrols in Nashville, TN – Found reduction in burglaries during 6-day periods of helicopter patrol • Alpert et al. 1998 – NIJ helicopter pursuit study – Studied effectiveness of helicopters in police pursuits in Baltimore, MD and Miami-Dade, FL – Over 80% arrest success rate when helicopters involved in pursuits Prior research on law enforcement aviation units • London Police Service Helicopter Research Project 1999-2000 – Assessed deterrent effect of helicopter patrols & impact of helicopter use on police efficiency – No effect of patrols except on rates of commercial breaking & entering – Improved police response times & rate of suspect apprehension • Toronto Police Service Air Support Unit evaluation 2000-2001 – More effective to hire 25 new officers than to pay $2.1 million for air support unit 2007 BJS Census of Law Enforcement Aviation Units • Census of agencies w/100+ sworn that reported operating a fixed-wing plane or helicopter in the 2003 BJS LEMAS survey • 1st national study on airborne law enforcement • Data collected from 3/08 to 9/08. -

Curriculum Vitae
Curriculum Vitae Name: Kenneth Darren Katz, M.D., FAAEM, FACMT Business Address: Department of Emergency Medicine Lehigh Valley Health Network 1240 South Cedar Crest Suite 214 Allentown PA 18103 Education and Training Undergraduate: 08/1988 – 05/1992 Yale University BA - Biology New Haven, CT Graduate: 06/1992 – 06/1996 State University of New York MD Stony Brook School of Medicine Post-Graduate: 07/1996 – 06/2001 Christiana Care Health Systems Resident in Emergency and Newark, DE Internal Medicine 07/2001 – 06/2003 Good Samaritan Regional Medical Toxicology Fellowship Medical Center Phoenix, AZ 07/1997 – 08/1997 Dr. Phillip Heinegg Family practice externship Yonkers, NY Appointments and Positions Academic: 01/2015-present Philadelphia College Osteopathic Medicine Clinical Assistant Professor 07/2013- present Lehigh Valley Health Network Core Faculty Department of Emergency Medicine 07/2010- 6/2013 Department of Internal Medicine Adjunct Asst. Professor West Virginia University School of Medicine 06/2007- 6/2013 University of Pittsburgh Division Chief Department of Emergency Medicine Division of Medical Toxicology 06/2005- 12/2012 Pittsburgh Poison Center Medical Director 10/2012 – 6/2013 University of Pittsburgh Associate Professor Department of Emergency Medicine School of Medicine 07/2004 - 10/2012 University of Pittsburgh Assistant Professor Department of Emergency Medicine School of Medicine 07/2004 -01/2009 University of Pittsburgh Fellowship Director Department of Emergency Medicine Division of Medical Toxicology 7/2003 – 6/2004 University of Pittsburgh Clinical Instructor Department of Emergency Medicine School of Medicine Non-Academic: 06/2007 - present St. Margaret’s Hospital Staff Physician Emergency Department UPMC Health System Pittsburgh, PA 07/2004 – present University of Pittsburgh Staff Physician Department of Emergency Medicine 07/2003 – present University of Pittsburgh Medical Toxicologist 2 Curriculum Vitae Kenneth D. -
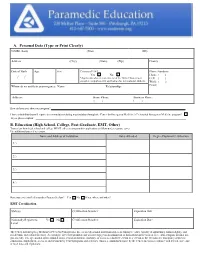
Application Packet
A. Personal Data (Type or Print Clearly) NAME (Last) (First) (MI) Address (City) (State) (Zip) County Date of Birth Age Sex Citizen of US* Phone Numbers: Yes No Home: ( ) / / *Applicants who are not citizens of the United States must Cell: ( ) complete a supplemental application for international students. Work: ( ) Whom do we notify in an emergency: Name: Relationship: Email: Address: Home Phone: Business Phone: ( ) ( ) How did you hear about our program? I have a disability that will require accommodations during matriculation through the Center for Emergency Medicine’s Prehospital Emergency Medicine program? If yes, please explain: B. Education (High School, College, Post-Graduate, EMT, Other) Transcripts from high school and college MUST either accompany this application or follow under separate cover. Use additional paper if necessary. Name and Address of Institution Dates Attended Degree/Diploma/Certification 1.) 2.) 3.) 4.) Have you ever enrolled in another Paramedic class? Yes No If yes, where and when? EMT Certification State(s): Certification Number: Expiration Date: Nationally Registered: Yes No Certification Number: Expiration Date: Level: The Center for Emergency Medicine of Western Pennsylvania, Inc., as an educational institution and as an employer, values equality of opportunity, human dignity, and racial/ethnic and cultural diversity. Accordingly, the Center prohibits and will not engage in discrimination or harassment on the basis of race, color, religion, national ori- gin, ancestry, sex, age, martial status, familial status, sexual orientation, disability, or status as a disabled veteran or a veteran of the Vietnam era. This policy applies to admissions, employment, access to and treatment by Center programs and activities. -

Global Military Helicopters 2015-16 Market Report Contents
GLOBAL MILITARY HELICOPTERS 2015-16 MARKET REPORT CONTENTS MARKET OVERVIEW 2 MILITARY HELICOPTER KEY REQUIREMENTS 4 EUROPE 5 NORTH AMERICA 10 LATIN AMERICA & THE CARIBBEAN 12 AFRICA 15 ASIA-PACIFIC 16 MIDDLE EAST 21 WORLD MILITARY HELICOPTER HOLDINGS 23 EUROPE 24 NORTH AMERICA 34 LATIN AMERICA & THE CARIBBEAN 36 AFRICA 43 ASIA-PACIFIC 49 MIDDLE EAST 59 EVENT INFORMATION 65 Please note that all information herein is subject to change. Defence IQ endeavours to ensure accuracy wherever possible, but errors are often unavoidable. We encourage readers to contact us if they note any need for amendments or updates. We accept no responsibility for the use or application of this information. We suggest that readers contact the specific government and military programme offices if seeking to confirm the reliability of any data. 1 MARKET OVERVIEW Broadly speaking, the global helicopter market is currently facing a two- pronged assault. The military helicopter segment has been impacted significantly by continued defense budgetary pressures across most traditional markets, and a recent slide in global crude oil prices has impacted the demand for new civil helicopters as well as the level of activity for existing fleets engaged in the offshore oil & gas exploration sector. This situation has impacted industry OEMs significantly, many of which had been working towards strengthening the civil helicopter segment to partially offset the impact of budgetary cuts on the military segment. However, the medium- to long-term view of the market is promising given the presence of strong fundamentals and persistent, sustainable growth drivers. The market for military helicopters in particular is set to cross a technological threshold in the form of next-generation compound helicopters and tilt rotorcraft. -

Aircraft Types Used in Law Enforcement
Aircraft Types used in Law Enforcement ACT Lancair Philippines, Airships [all types] R series [R33 etc.] United Kingdom, Skyship France, Japan, United Kingdom, United States, Virgin/ABC Lightships Belgium, France, United Kingdom, Aeritalia AMC-3/AL60 South Africa, Aero 24 Hungary, 45 [K-75] Czechoslovakia, Hungary, AP-32 Czechoslovakia, C-104 Czechoslovakia, Aeronca 7AC United States, Aero Baero 180RVR Argentina Aero Commander [see Rockwell] Commander/Shrike Commander Australia, Bahamas, Colombia, Costa Rica, Indonesia, Iran, Kenya, Panama, United States, Airspeed Ferry United Kingdom, Agusta A109 Australia, Austria, Belgium, Ghana, Italy, Japan, Slovenia, Spain, Switzerland, United Arab Emirates, United Kingdom, United States, Venezuela, AB139 Oman, Albatross CIII Germany, DIII Germany, Antonov An-2 Estonia, Latvia, Mongolia, Nicaragua, Poland, Russia An-24 Mongolia, An-26 Nicaragua, An-32 Mexico, Peru, Russia An-72 Russia Arado 68 Germany 96 [Avia C-2B] Czechoslovakia, Armstrong-Whitworth AW660 Argosy C1 United Kingdom, ATR ATR42 Italy, Auster Auster Falkland Islands, Hong Kong, Kenya, Malaysia [RAF], Netherlands, United Kingdom, Avia International Police Aviation Research - law enforcement aircraft types 2 B-534 Czechoslovakia, S-89 [Supermarine Spitfire] Czechoslovakia, S-97 [Lavockin La-7] Czechoslovakia, S-99/S-199 [Bf109] Czechoslovakia, C-2B [Arado 96B] Czechoslovakia, K-65 [Fiesler Fi-156C] Czechoslovakia, K-75 [Aero 45] Czechoslovakia, VR-1 [Fa-223] Czechoslovakia, Avro Anson Australia 748 Sri Lanka, United Kingdom, Ayres S-2 -

Helicopter EMS (HEMS) Programs in the United States Were Largely Not-For-Profit Hospital Or Public Safety Operations Until the Late 1990’S
National Association of State EMS Officials – Air Medical Services Committee Brief Outline of the Federal Pre-emption Issues in Regulating Air Medical Services October, 2011 Helicopter EMS (HEMS) programs in the United States were largely not-for-profit hospital or public safety operations until the late 1990’s. These programs were generally well integrated with state and local EMS system. An increase in Medicare reimbursement for air ambulance transports in the early 2000’s appears to have contributed to a significant increase in the number of HEMS programs, medical helicopters, and for-profit operators. The number of air medical transports doubled between 2000 and 2010. The number of helicopter crashes increased as well, drawing public and National Transportation Safety Board attention to the issue. Some for-profit operators use aggressive tactics and marketing to increase flights. Unlike passengers who choose an air carrier to use on a vacation or business trip, patients typically have little or no say in what service is utilized to transport them by air ambulance. As states have attempted to regulate HEMS programs and ensure their integration with state and local EMS systems, operators have responded with lawsuits asserting the exclusive authority of the Federal Aviation Administration under the Airline Deregulation Act (PL 95-504) of 1978 (ADA). The ADA pre-empts states from regulating the rates, routes, or services of an air carrier. When Congress passed the ADA, there were very few HEMS programs in the United States, and it is doubtful that there was any consideration of the impact of the ADA on the regulation of air ambulances by states. -

JOURNAL of Health & Life Sciences
Journal of Health & Life Sciences Law VOLUME 4, NUMBER 2 FEBRUARY 2011 TABLE OF Meet the Fraud Busters: Program Safeguard Contractors CO N TE N TS and Zone Program Integrity Contractors ................................. 1 by Sara Kay Wheeler, Stephanie L. Fuller, and J. Austin Broussard The Link Between Quality and Medical Management: Physician Tiering and Other Initiatives .................................. 36 by Rakel Meir and Paul W. Shaw Medical Control of Emergency Medical Services .................. 65 by Rick L. Hindmand and W. Ann Maggiore Quality in Action: Paradigm for a Hospital Board- Driven Quality Program .......................................................... 95 by Elisabeth Belmont, Claire Cowart Haltom, Douglas A. Hastings, Robert G. Homchick, Lewis Morris, Robin Locke Nagele, Kathryn C. Peisert, Brian M. Peters, Beth Schermer, and Julie Taitsman NOTES A N D The Employee Exceptions to the Anti-Kickback and COMME N TS Stark Laws After Tuomey: What’s a Physician’s Employer To Do? ..................................................................... 146 by Susan O. Scheutzow and Steven A. Eisenberg PRACTICE Data Privacy Concerns for U.S. Healthcare RESOURCE Enterprises’ Overseas Ventures ............................................. 173 by Vadim Schick Journal of Health & Life Sciences Law 65 Medical Control of Emergency Medical Services Rick L. Hindmand and W. Ann Maggiore ABSTRACT: Effective medical control by medical directors and other medical oversight professionals is an essential element in providing appropri- ate emergency medical services (EMS). Within an EMS system, EMS medical directors have a supervisory rather than agency relationship with the emer- gency medical technicians (EMTs). Contrary to some commentary on the legal framework of this relationship, EMTs do not practice “under the license” of the medical director, but instead practice pursuant to their own state or county licenses, which generally require physician supervision. -

Emergency Medical Services Statutes and Regulations
Emergency Medical Services Statutes and Regulations Printed: August 2016 Effective: September 11, 2016 1 9/16/2016 Statutes and Regulations Table of Contents Title 63 of the Oklahoma Statutes Pages 3 - 13 Sections 1-2501 to 1-2515 Constitution of Oklahoma Pages 14 - 16 Article 10, Section 9 C Title 19 of the Oklahoma Statutes Pages 17 - 24 Sections 371 and 372 Sections 1- 1201 to 1-1221 Section 1-1710.1 Oklahoma Administrative Code Pages 25 - 125 Chapter 641- Emergency Medical Services Subchapter 1- General EMS programs Subchapter 3- Ground ambulance service Subchapter 5- Personnel licenses and certification Subchapter 7- Training programs Subchapter 9- Trauma referral centers Subchapter 11- Specialty care ambulance service Subchapter 13- Air ambulance service Subchapter 15- Emergency medical response agency Subchapter 17- Stretcher aid van services Appendix 1 Summary of rule changes Approved changes to the June 11, 2009 effective date to the September 11, 2016 effective date 2 9/16/2016 §63-1-2501. Short title. Sections 1-2502 through 1-2521 of this title shall be known and may be cited as the "Oklahoma Emergency Response Systems Development Act". Added by Laws 1990, c. 320, § 5, emerg. eff. May 30, 1990. Amended by Laws 1999, c. 156, § 1, eff. Nov. 1, 1999. NOTE: Editorially renumbered from § 1-2401 of this title to avoid a duplication in numbering. §63-1-2502. Legislative findings and declaration. The Legislature hereby finds and declares that: 1. There is a critical shortage of providers of emergency care for: a. the delivery of fast, efficient emergency medical care for the sick and injured at the scene of a medical emergency and during transport to a health care facility, and b. -

Search and Rescue/Emergency Medical Services
SEARCH AND RESCUE/EMERGENCY MEDICAL SERVICES UA Log ist ics /Av iat ion Use this area for cover image (height 6.5cm, width 8cm) Patrick Bosman Aviation Manager GoM Copyright of Shell Upstream Americas/Logistics/Aviation 1 GOAL Introduce the Search and Rescue/Emergency Medical Services ppyrovide by Era Helico pters Copyright of Shell Upstream Americas/Logistics/Aviation 2 SAR/EMS CONTRACT Started in March 2011 5 Members (Shell membership is split; UA 90%, SPLC 10%) Monthly fee for members Pay fixed dispatch fee and actual flight hours Copyright of Shell Upstream Americas/Logistics/Aviation 3 RESOURCES 2x 24/7 Solely Dedicated SAR/Emergency Medical Services AW139 Helicopp(ters (Galveston and Fourchon ) VFR/IFR Day/Night Operations Night Vision Goggles 15 Minute Launch Time Day/Night 24 Hour Rescue Coordination Call Center Advanced Life Support Paramedics Rescue Swimmer OtHitCblOverwater Hoist Capable Capable of Long Range Flights Copyright of Shell Upstream Americas/Logistics/Aviation 4 COVERAGE Copyright of Shell Upstream Americas/Logistics/Aviation 5 A LOOK INSIDE Copyright of Shell Upstream Americas/Logistics/Aviation 6 SAR/EMS PROCEDURE Emergency Response Plan Air Ambulance (EMS) call -out Notify dispatcher that this is a ‘SHELL’ emergency Assessment byyp dispatcher Dispatch of ERA helicopter Coverage GoM meets 4 hour MER requirement Updates of mission through email Close-out report at end of mission Copyright of Shell Upstream Americas/Logistics/Aviation 7 CRITICAL CATEGORY DEFINITIONS Copyright of Shell Upstream -

Need for Helicopter Emergency Medical Services (Hems) in Rural British Columbia
NEED FOR HELICOPTER EMERGENCY MEDICAL SERVICES (HEMS) IN RURAL BRITISH COLUMBIA by Roberta Squire PROJECT SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF BUSINESS ADMINISTRATION UNIVERSITY OF NORTHERN BRITISH COLUMBIA March 2014 © Roberta Squire, 2014 ABSTRACT Currently, there is no dedicated helicopter emergency medical service (HEMS) in Northern British Columbia (BC). Injuries to workers in BC result in the loss of more economically productive years than heart disease and cancer combined and cost nearly $2.8 billion per year. Nearly three quarters of all people who die of trauma-related conditions in Northern BC do so before they can be brought to a hospital; 82% in Northwestern BC, compared to 12% in Metro Vancouver (Cameron 2007; McKenna 2013). Minimizing the time from injury to optimal trauma care through the utilization of HEMS has been adopted as an essential component of emergency care infrastructures Globally. The purpose of this paper is to examine the opportunities, challenges and needs of a dedicated helicopter emergency medical system to service the remote regions of Northern BC. lll TABLE OF CONTENTS Approval 11 Abstract Ill Table of contents IV List of Tables VI List of Figures Vll Abbreviations Vlll Acknowledgements X Chapter I Introduction 1 Chapter II Literature Review 7 Section 2.1 Need for HEMS Services in Northern British Columbia 7 Section 2.2 Brief History of HEMS in Canada and World-wide 8 Section 2.3 Review of Literature on Helicopter Emergency Medical Services in BC 11 Section -

Stephen Is a Consultant in Emergency Medicine Employed by NHS Greater Glasgow and Lead Consultant for Scotland’S Aeromedical Retrieval Service
Dr Stephen Hearns MB ChB FRCP FRCS FRCEM FRGS Dip.IMC DRTM Stephen is a Consultant in Emergency Medicine employed by NHS Greater Glasgow and lead consultant for Scotland’s aeromedical retrieval service. He has completed Bond Solon and Royal College of Physicians and Surgeons training courses relating to the role of expert witness. He regularly acts an expert witness for the NHS Scotland Central Legal Office and for pursuers’ solicitors. He is the Scottish Public Service Ombudsman’s expert advisor in emergency medicine and pre-hospital care. Stephen finished his training with the London Helicopter Emergency Medical Service. Over the past ten years he has led the establishment of the Emergency Medical Retrieval Service in Scotland. He leads a team of 40 doctors, nurses and paramedics who work for the service. He has published a number of papers and book chapters related to emergency medicine and pre-hospital care. He also led the team establishing the Diploma in retrieval and transfer medicine for the Royal College of Surgeons of Edinburgh and contributes to the organisation of the annual UK retrieval conference. He is attracted to the challenges of retrieval medicine in demanding remote environments with limited resources. He has been an active voluntary member of Arrochar mountain rescue team for 18 years and holds the Mountain Leader Award. Stephen acted as medical officer on seven international expeditions before establishing the first expedition medicine course in the UK. He has previously been an instructor on ATLS, ALS and PALS courses. Stephen is married to Kerry and has three sons. Stephen enjoys mountains, road cycling and mountain biking. -

PAR's Listing of Aircraft Used in Law Enforcement
Police Aviation Research AIRCRAFT USED FOR LAW ENFORCEMENT SINCE 1914 The listing below includes those aircraft types associated with airborne law enforcement since 1914. In some instances this refers to one use in isolation in others an alleged and recorded in a public document but a use not subsequently proven. See the entry for the Blackburn Botha. We can be certain it is spurios but it is in a public record and has therefore been included. This list should be taken as a guide and/or a basis for further research. Manufacturer ModelModel CountryCountry ofof use ACT Lancair Philippines, Airships [all types] R series [R33 etc.] United Kingdom, Skyship France, Japan, Trinidad & Tobago, United Kingdom, United States, Virgin/ABC Lightships Belgium, France, United Kingdom, Aeritalia AMC-3/AL60 South Africa, Aero 24 Hungary, 45 [K-75] Czechoslovakia, Hungary, AP-32 Czechoslovakia, C-104 Czechoslovakia, Aeronca 7AC United States, Aero Baero 180RVR Argentina Aero Commander see Rockwell CCommander/Shrike d /Sh ik Australia, t li BBahamas, h Colombia, C l bi Costa C t Rica, Ri Commander Indonesia, Iran, Kenya, Panama, United States, Airspeed AS4 Ferry United Kingdom, Agusta A109 Australia, Austria, Belgium, Bosnia-Herzegovenia, Bulgaria, Chile, China, Ghana, Italy, Japan, Oman, SlSlovenia, i SSpain, i SSwitzerland, it l d United U it d Arab A b Emirates, E i t United Kingdom, United States, Venezuela, AW119 Brazil, Finland, Uganda, United States AW139 Bulgaria, China, Cyprus, South Korea, Malaysia, Netherlands, Oman, Spain, Trinidad & Tobago,