Reporter 2015 Volume 3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

University of San Diego Women's Soccer Media Guide 1998
University of San Diego Digital USD Soccer (Women) University of San Diego Athletics Media Guides Fall 1998 University of San Diego Women's Soccer Media Guide 1998 University of San Diego Athletics Department Follow this and additional works at: https://digital.sandiego.edu/amg-soccer-women Digital USD Citation University of San Diego Athletics Department, "University of San Diego Women's Soccer Media Guide 1998" (1998). Soccer (Women). 6. https://digital.sandiego.edu/amg-soccer-women/6 This Catalog is brought to you for free and open access by the University of San Diego Athletics Media Guides at Digital USD. It has been accepted for inclusion in Soccer (Women) by an authorized administrator of Digital USD. For more information, please contact [email protected]. commitment UNIVERSITY OF SAN DIEGO TOREROS USDA thletic Administration President Alice B. Hayes NCAA Faculty Rep. Mitch Malachowski Athletic Director Tom Iannacone CIIAHPIO Associate Athletic Director Dan Yourg Assistant Athletic Director/SWA Wendy Guthrie Director of Athletic Development Brian Fogarty Director of Athletic Promotions/Mrktg. Renee Wiebe Director of Facilities John Martin Director of Intramurals/Recreation Gary Becker Head Athletic Trainer Carolyn Greer, M.A., A.T., C. Assistant Trainers Suzi Higgins, Steve Grec h Sports Information Director Ted Gosen Assistant SID/Women's Soccer Contact Ryan McCrary Womens Soccer Information Head Coach John Cossaboon, (Second year) Assistant Coach Ada Greenwood (First year) Assistant Coach Tommy Tate (Fourth year) Women's Soccer -

Science for the People Magazine Vol. 11, No. 4
CHAPTERS AND CONTACTS ~cit>nH' tor the People is an organization ,of people involved or interested in science and technology-related issues, whose activities Jrt' d1rected at· 1) exposing the< lass control of science and technology, 2) organizing campaigns which criticize, challenge and proP,ose altt•rnati' cs to the present uses of science and technology, and 3) developing a political strategy by which people in the technical strata can all\ with other progressive forces in socit>ty. SftP opposes the ideologies of sexism, racism, ·elitism and their practice, and holds an anti impt•rialist world-view. Membership in SftP is defined as subscribing to the magazine and/or actively participating in local SftP activities. ARIZONA: Sedley A1leen Josserand IOWA: Henry Howe. Dept of Zoology. VIRGINIA: Je_<m Loria. Route A. Box 3730 East Bellevue No 9 Tucson. AZ Un1vers1ty of Iowa. Iowa C1ty. Iowa 52242 496. Apt 7 A. Charlottesville. VA 85716 P"ul C Nelson 604 Hodge Ames. (804) 97 3-1206. ARKANSAS: Joe Neal P 0 Box 1772 lA 50010 (515) 232 2527 Fayetteville AR 727.01 Dotty Ol1ver. P WASHINGTON: Phil Bereano. 316 0 MARYLAND: Bahimore Chapter: c. r. Guggenheim. FS-15. Univ. of Washington. Box 2641 L1ttle Rock. AR 72201 Alternat1ve Press Center 2958 Greenmount Seattle. WA 98195. (206) 543-9037. CALIFORNIA: Berkeley Chapter: Ave Balt1mor<' MD 21218 Sc1ence for the People P 0 Box 4161 WISCONSIN: Cal Pierce. 525 W. Dayton Berkeley CA 94704 Kevm Cadogan. 1033 MASSACHUSETTS: Amherst No 2. Madison. WI 53703. (608) 255- Rose Ave Oakland. CA 94611 (415) 658 Chapter: Marvin Kalkstein. -

Autry Uniforms Optional by Meghan Miller a Light Blue Uniform Shirt Or a Shoe Beckwith Was Placed in Charge of THRESHER STAFF Tag
• aV- *• * e Rice Thresher Vol. LXXXVIII, Issue No. 28 SINCE 1916 Friday, April 20, 2001 Autry uniforms optional by Meghan Miller a light blue uniform shirt or a shoe Beckwith was placed in charge of THRESHER STAFF tag. Uniforms will still be available the recreation center earlier this se- for those who want them. mester. Mandatory Autry Court uniforms Right now, check-in will involve "I like to run and lift weights after are finally gone. signing a sheet of paper at the equip- [running]," said Tiffany Bludau, a After nearly six months of dis- ment room desk, but people will soon member of the Student Association cussion, uniforms in the recreation have to swipe a Rice ID card or a Uniform Policy Committee and a Sid center, which encompasses Autry recreation center membership card Richardson College sophomore. "It Court and other athletic facilities, to use the facilities. The sign-in sheet discouraged me when I'm already will no longer be required begin- will monitor the numbers of people working out and then I have to go ning Monday, the Office of Student coming through the center. change to work out [at the gym J. It'll Affairs announced this week. "Hopefully, students will appre- be nice, you can come in from a run A series of other administrative ciate the fact that they don't have to and then lift weights or whatever." changes in the recreation center will use the facility uniforms anymore so The UPC, headed by Beckwith, also be implemented. they won't mind taking a few sec- examined Autry Court's identifica- People using the weight room onds to write their names down," tion and safety policy when discuss- and gym facilities will be required to Student and Recreation Centers Di- ing uniform alternatives. -
Autobiography in Fiction
TEFTX13 S ER October 29, 1982 A Journal of Free Voices 75 .0 Autobiography in Fiction 'M GOING TO talk about myself— which, I suppose, is what is ex- I pected of me. But certainly not from the position of defending myself or even from that of a "writer of autobiographi- cal fiction." I'm afraid that definition of me would not be nearly enough. I'm way beyond that. Way beyond autobiog- raphy! I've passed on through and come out somewhere else — beyond myself— long ago. So I'm not taking a stand and I do not appear here as an exponent of, or even as a maker of, autobiographical — except in my own way! — anymore than one of what is called "experimental fic- tion." Yet for me iverything I have ever written, just about, I guess, has been in the nature of experiment — most of the time. My question has been, and keeps being, "How in the world will I do it? Well, let me try this, let me try that." I've really been experimenting to see if I could write — at all — what I had in mind, whatever vision I had, whatever it was that was obviously pushing me to get the design of, to get some meaning of — and some relief from, some peace, so it would let me alone. So it's all been an experiment — and, finally, invention, imagination, fabrication — way beyond where I started. Drawing by Ancel Nunn And I ask myself — have asked many many times in my writing life — : what would I ever have written had I not come An essay by William Goyen on a time, a place, from that place: what would I have ever written had I not heard those people and a people speaking -

Drawn in the Dirt Lines
TEXAS 1) ERVE A Journal of Free Voices November 9, 1984 $1.00 Pesticide Battle Lines Drawn In the Dirt By Geoffrey Rips Austin hen Agriculture Com- missioner Jim High- W tower, announced on Wednesday, October 19, that the Texas Department of Agriculture (TDA) was promulgating new regulations for the application of agricultural pesticides, a political range war that had been raging for months underground suddenly burst to the surface. While the regulations proposed for public comment were the result of ex- haustive negotiations and heated skirmishes between TDA and public and private interest groups, they are not the actual point of contention they are made out to be by groups opposing their im- plementation. Rather, the pesticide regulations are being used by large political and private interest groups to draw the line on Jim e u Hightower and on a process of Pog change that has shaken these in- lan terest groups loose from the A stranglehold on the state's by to agricultural and economic policies Pho they so long enjoyed. - -------- -1=z---N -----\--;74 1 = =---1--------- - 1---- . • PAGE TWO • ----A -- $ F OE . - — — - —7- -: 52: ---. - . - % „ HE PEOP ..-/-__- -&-.. .- Lines (Continued from Cover) _-:.. Ever since the election of Jim Hightower in 1982, ,_ __ LTh■ conservative political and farm interests have been itching for -- Sr — III PRIE144 mow an opportunity to take a shot at him. Among those interests -' , fiir4,11iitaq-.0•-... f , have been agribusiness concerns who had enjoyed a cozy cofi „_. •--,...--. relationship with Hightower's predecessor, Reagan Brown. ,, ,,, ••••••• 0 For the most part, these interests reap the most benefit from ..;.:__ ,-,46...:_ =En , _ 1 pi i A,7 ; .;.11. -

Analysis of the Complete Medical
Lone — Table of Contents — Executive Summary 8 Purpose and Scope 11 Background on the Florida Market 11 Organization of this Report 12 Analysis of the Complete Medical Malpractice Line of Business 12 Comparisons to Other Leading States 13 Top 10 States by Medical Malpractice Premium Volume 13 Loss and DCC Information for the Top 10 States 13 Expense Information for the Top 10 States 16 Profitability Measures for the Top 10 States 20 Analysis of Florida Malpractice Results for Leading Carriers in Overall Medical Malpractice Line in Florida 21 Leading Medical Malpractice Carriers in Florida and Their Loss and DCC Ratios 22 Expense Information for Leading Medical Malpractice Carriers in Florida 26 Profitability of Leading Medical Malpractice Carriers in Florida 30 Overall Financial Strength Measures for Leading Medical Malpractice Carriers in Florida 37 Composition of the Total Florida Medical Malpractice Market by Type of Insurer 41 Florida Marketplace Dynamics for the Total Medical Malpractice Line – Activity in the Admissions Unit 42 Recent Medical Malpractice Legislation 44 Analysis of the Physicians and Surgeons Subline 44 Comparisons to Other Leading States 45 Leading Physicians Carriers in Florida 47 Composition of Florida Physicians Malpractice Market by Type of Insurer 48 Florida Marketplace Dynamics for the Physicians Malpractice Subline 50 Comparison of Florida Physicians Rates to Those of Other States 53 Physicians Malpractice Rate Filings in 2016 56 Analysis of the Other Healthcare Professionals Subline 60 Diversity of the Insureds -
Borders and Unions in the Valley
TEXAS 13 SERVER March 9, 1984 A Journal of Free Voices 75C Borders and Unions in the Valley By Geoffrey Rips San Benito T IS A HOUSE like many others in this neighborhood of small frame I and cinder-block houses a few blocks from the expressway connecting Harlingen and Brownsville. A house like many others with a garden and white- washed cinder-block walls. But there are a large number of people entering and leaving the door at the back of this house. And on a door at the front "Casa Oscar Romero" is painted in black. On this late afternoon in San Benito, five or six men in their late teens, twenties, and thirties kick around a soccer ball on the empty, dusty lot next to the house. An older man and young girl sit on a wooden bench with their backs against a wall of the house. The man grips the edge of the plank on which he is seated and stares off into space. The girl watches the men kicking the ball around and laughs. Near the rear entrance to the house three women are lco ca engaged in discussion. is n A trailer with a little awning attached Ma is located some hundred feet behind the house. Jack and Diane Elder live here Nancy with their four young sons while they by oversee the operation of this haven for to Central American refugees. Pho (Continued on Page 10) Bitter harvest of the freeze. In This Issue: nwersity Nicaraguan Defense Contracts Contradictions = N—= --..-_—.... — = ..=. — F....... ---- JP- - ____ ____ _ - —_.„ .s FOE . -
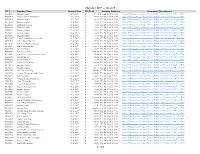
October 2017 -- Chart T PO # Supplier Name Creation Date PO Total Statutory Authority Competitive Procurement P0582507 Summus Staples 10/1/2017 $ 279.72 TX
October 2017 -- Chart T PO # Supplier Name Creation Date PO Total Statutory Authority Competitive Procurement P0582507 Summus Staples 10/1/2017 $ 279.72 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582508 Summus Praxair Distribution 10/1/2017 $ 225.42 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582509 Summus Staples 10/2/2017 $ 42.29 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582512 Summus Staples 10/2/2017 $ 619.19 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582514 Idexx Laboratories 10/2/2017 $ 36.00 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582515 Weber Scientific 10/2/2017 $ 53.40 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582516 Summus Staples 10/2/2017 $ 179.19 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582517 Summus Staples 10/2/2017 $ 12.60 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582518 Summus Staples 10/2/2017 $ 81.08 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0579057-1 Texas Petrographics Services Inc 10/2/2017 $ 98.00 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582519 OTool Plastic Pipe Inc 10/2/2017 $ 327.00 TX. Ed. Code 51.9335 https://bids.sciquest.com/apps/Router/PublicEvent?CustomerOrg=TexasTech P0582524 Valentines Building Services 10/2/2017 $ 1,838.10 TX. -

Corporate Structuresof of Independent Independent – Continued Insurance Adjusters, Adjusters Inc
NEW YORK PENNSYLVANIANEW YORK New York Association of Independent Adjusters, Inc. PennsylvaniaNew York Association AssociationCorporate of of Independent Independent Structures Insurance Adjusters, Adjusters Inc. 1111 Route 110, Suite 320, Farmingdale, NY 11735 1111 Route 110,110 Suite Homeland 320, Farmingdale, Avenue NY 11735 E-Mail: [email protected] section presents an alphabetical listing of insurance groups, displaying their organizational structure. Companies in italics are non-insurance entities. The effective date of this listing is as of July 2, 2018. E-Mail:Baltimore, [email protected] MD 21212 www.nyadjusters.org www.nyadjusters.orgTel.: 410-206-3155 AMB# COMPANY DOMICILEFax %: OWN 215-540-4408AMB# COMPANY DOMICILE % OWN 051956 ACCC HOLDING CORPORATION Email: [email protected] AES CORPORATION 012156 ACCC Insurance Company TX www.paiia.com100.00 075701 AES Global Insurance Company VT 100.00 PRESIDENT 058302 ACCEPTANCEPRESIDENT INSURANCE VICECOS INC PRESIDENT 058700 AETNA INC. VICE PRESIDENT Margaret A. Reilly 002681 Acceptance Insurance Company Kimberly LabellNE 100.00 051208 Aetna International Inc CT 100.00 Margaret A. Reilly PRESIDENT033722 Aetna Global Benefits (BM) Ltd Kimberly BermudaLabell 100.00 033652 ACCIDENT INS CO, INC. HC, INC. 033335 Spinnaker Topco Limited Bermuda 100.00 012674 Accident Insurance Company Inc NM Brian100.00 Miller WEST REGIONAL VP 033336 Spinnaker Bidco Limited United Kingdom 100.00 058304 ACMATVICE CORPORATION PRESIDENT 033337 Aetna Holdco (UK) LimitedEXECUTIVEWEST REGIONAL SECRETARYUnited Kingdom VP 100.00 050756 ACSTAR Holdings Inc William R. WestfieldDE 100.00 078652 Aetna Insurance Co Ltd United Kingdom 100.00 010607 ACSTARDavid Insurance Musante Company IL 100.00 091442 Aetna Health Ins Co Europe DAC WilliamNorman R. -

2016 Medical Malpractice Insurance Report
Massachusetts Division of Insurance Medical Malpractice Insurance Report For the 2016 Calendar Year Gary D. Anderson Commissioner of Insurance Acknowledgements This report was prepared by the State Rating Bureau staff of the Massachusetts Division of Insurance (“Division”). Matthew M. Mancini, State Rating Bureau Director, Gerald B. Condon, State Rating Bureau Researcher, Cara Blank, State Rating Bureau, Property Casualty Actuary, Cara Toomey, Counsel to the Commissioner, and Bashiru Abubakare, State Rating Bureau Actuary/Statistician, prepared the report and provided the analysis. The Division relies on insurance companies, the National Association of Insurance Commissioners, and other regulatory agencies for the accuracy of all reported financial information. Page ii TABLE OF CONTENTS Page Title ii Acknowledgments iii Table of Contents iv Included Figures 1 Executive Summary 2 Massachusetts Health Care Professionals 2 Number of Professionals 3 Liability Coverage Requirements 4 Market for Medical Malpractice Coverage 4 History 5 Licensed Insurance Companies 6 Surplus Lines Carriers 7 Risk Retention Groups 9 Shares of the Market 10 Financial Results for Insurance Carriers 10 Premiums 11 Costs 12 Loss Ratios 14 Profitability 15 Premiums for Medical Malpractice Coverage 16 Average Claim Costs 19 Premiums Compared to Those of Other States 21 Recent Medical Malpractice Reforms 22 Conclusion 23 Appendix A-1: Medical Malpractice Insurance Companies 24 Appendix A-2: Medical Malpractice Surplus Lines Carriers 26 Appendix A-3: Medical Malpractice -
2019 Annual Report
STATE OF ARKANSAS ASA HUTCHINSON, GOVERNOR ARKANSAS INSURANCE DEPARTMENT ALAN MCCLAIN ARKANSAS INSURANCE COMMISSIONER _____ ANNUAL REPORT SHOWING THE ARKANSAS BUSINESS FOR THE YEAR 2019 OF ALL INSURANCE COMPANIES, ASSOCIATIONS, AND FRATERNAL ORDERS TRANSACTING BUSINESS IN ARKANSAS. ____ MISSION STATEMENT The primary mission of the State Insurance Department shall be consumer protection through insurer solvency and market conduct regulation, and fraud prosecution and deterrence. OUR VISION Our vision is to serve and protect the public interest by the efficient and equitable enforcement of the state’s laws and regulations affecting the insurance industry. CORE VALUES The Insurance Department is comprised of several divisions with a wide variety of services to the public, public employees, and the industry. Our core values are: • Efficiency in our internal workings and in assisting consumers externally. • Results that benefit Arkansas consumers and lead to growth for the Industry. • Transparency in the rate-making process. • Leadership among state regulators in growing industry and protecting consumers. Michael Preston SECRETARY OF COMMERCE Alan McClain COMMISSIONER, ARKANSAS INSURANCE DEPARTMENT TABLE OF CONTENTS Commissioner’s Letter 1 Message from the Commissioner 2 Administration Division 3 Accounting Division 4 Compliance Division 12 Consumer Services Division 14 Criminal Investigation Division 15 Finance Division 16 Human Resources Division 21 Information Systems Division 21 Legal Division 22 License Division 25 Liquidation Division -

2019 DIFS Annual Report
www.michigan.gov/DIFS ANNUAL REPORT 2020 A YEAR IN REVIEW From the Director The Honorable Gretchen Whitmer, Governor of Michigan State Capitol Building Lansing, Michigan 48933 Subject: 2020 Department of Insurance and Financial Services Annual Report Dear Governor Whitmer: The Annual Report, prepared pursuant to Section 238 of the Michigan Insurance Code of 1956, 1956 PA 218, MCL 500.238 and Section 2108 of the Michigan Banking Code of 1999, 1999 PA 276, MCL 487.12108, is a valuable reference for information about regulated entities engaged in the business of insurance, banking, and consumer finance in Michigan. The Department of Insurance and Financial Services (DIFS) is responsible for regulating Michigan's insurance and financial industries. The entities that DIFS regulated in 2020 included: 25 HMOs, 77 banks, 123 domestic insurance companies, 136 credit unions, 1,500 foreign insurance companies, 318,223 individual insurance agents, 21,771 insurance agencies, 17,432 mortgage licensees and registrants, 444 deferred presentment licensees, and 2,494 other consumer finance-related entities. This annual report is also available on the DIFS website at www.michigan.gov/DIFS under “Publications.” Sincerely, Anita G. Fox Director Department of Insurance and Financial Services 2 Table of Contents 4 Office of Responsibilities 7 Budget and Revenue 9 Office of Consumer Services 11 Office of Communications 12 Office of General Counsel 13 Receivership Statistical Information 14 Office of Research, Rules and Appeals 15 Office of Insurance Licensing and Market Regulation 17 Office of Consumer Finance 19 Office of Banking 25 Office of Credit Unions 33 Office of Insurance Evaluation 39 Entity Type Definition 3 DIFS Office Responsibilities Office of Banking Responsible for all aspects of the supervision, regulation and examination of state-chartered banks, savings banks, trust-only banks, and trust departments, including processing related corporate applications and requests.