Gaston Controlled Substances Coalition 2017-2020 Strategic Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
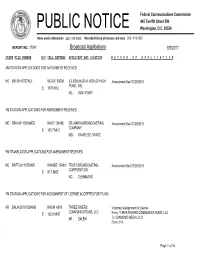
Broadcast Applications 8/3/2011
Federal Communications Commission 445 Twelfth Street SW PUBLIC NOTICE Washington, D.C. 20554 News media information 202 / 418-0500 Recorded listing of releases and texts 202 / 418-2222 REPORT NO. 27542 Broadcast Applications 8/3/2011 STATE FILE NUMBER E/P CALL LETTERS APPLICANT AND LOCATION N A T U R E O F A P P L I C A T I O N AM STATION APPLICATIONS FOR AMENDMENT RECEIVED NC BR-20110727ACL WGOS 56508 IGLESIA NUEVA VIDA OF HIGH Amendment filed 07/29/2011 POINT, INC. E 1070 KHZ NC , HIGH POINT FM STATION APPLICATIONS FOR AMENDMENT RECEIVED MD BRH-20110518AED WXCY 53488 DELMARVA BROADCASTING Amendment filed 07/29/2011 COMPANY E 103.7 MHZ MD , HAVRE DE GRACE FM TRANSLATOR APPLICATIONS FOR AMENDMENT RECEIVED NC BRFT-20110725AEI W249BZ 154301 TRUTH BROADCASTING Amendment filed 07/29/2011 CORPORATION E 97.7 MHZ NC , CLEMMONS FM STATION APPLICATIONS FOR ASSIGNMENT OF LICENSE ACCEPTED FOR FILING AR BALH-20110729AHB KHOM 6619 THREE RIVERS Voluntary Assignment of License COMMUNICATIONS, LLC E 100.9 MHZ From: THREE RIVERS COMMUNICATIONS, LLC AR , SALEM To: DIAMOND MEDIA, LLC Form 314 Page 1 of 44 Federal Communications Commission 445 Twelfth Street SW PUBLIC NOTICE Washington, D.C. 20554 News media information 202 / 418-0500 Recorded listing of releases and texts 202 / 418-2222 REPORT NO. 27542 Broadcast Applications 8/3/2011 STATE FILE NUMBER E/P CALL LETTERS APPLICANT AND LOCATION N A T U R E O F A P P L I C A T I O N FM STATION APPLICATIONS FOR ASSIGNMENT OF LICENSE ACCEPTED FOR FILING MO BALH-20110729AHC KBMV-FM 29623 THREE RIVERS Voluntary Assignment of License COMMUNICATIONS, LLC E 107.1 MHZ From: THREE RIVERS COMMUNICATIONS, LLC MO , BIRCH TREE To: DIAMOND MEDIA, LLC Form 314 FM STATION APPLICATIONS FOR ASSIGNMENT OF PERMIT ACCEPTED FOR FILING MA BAPED-20110729AGI WJCI 177345 MORGAN BROOK CHRISTIAN Voluntary Assignment of Construction Permit RADIO, INC. -

Charlotte, North Carolina Photograph Courtesy of the Convention and Visitors Bureau Charlotte
Charlotte, North Carolina Photograph courtesy of the Convention and Visitors Bureau Charlotte. harlotte is a city of the New South. This ’90s provided a chance to test the “Charlotte C means the city’s energy, government model” of arts support. Though most arts and public policies tend to focus more groups saw a dip in ticket sales and donations on the future than the past. Drive, or better yet after the September 11 terrorist attacks, no walk, through the center of town today and major arts organization has gone under or “Being you’ll find few buildings from the city’s history failed to regroup. Most were riding a wave of as a 19th-century trading crossroads and textile budget and ticket-sales growth right up to early pro-culture is center. Although the early 20th century 2002, when county and city funding to the cen- the business brought considerable industry and growth to tralized Charlotte-Mecklenburg Arts & Science the town, urban renewal in the 1970s leveled Council (ASC) all at once dropped about $2 environment nearly half the central wards’ houses and million—or 13 percent of the council’s $15.2 churches to make room for plazas, malls, sky- million budget. State funding to the council here.” scrapers, performance venues, a sports stadium likewise has been cut from a high of $170,000 Tom Gabbard and condominiums. The now-vibrant city core in 2000 to $94,000 in 2003. president is referred to only as Uptown. There is no An October 2003 analysis released by Blumenthal Center for “down” in Charlotte’s civic image of itself. -

PROOF Aug 2013
Next Issue Available in September My City Magazine . August 2013 . Vol. 1 Issue 1 Cover Art by John Hairston, Jr. “Queen Charlotte” Mena Mae Chan by Ellen Gurley | Page 4 Learnby Bill “The to Thrill” Take Cleveland a Joke | Page America 14 Andrewby Ellen Gurley Taylor | Page 5 Monicaby Shane Elks Jeffries | Page 15 Funkyby Ellen Gurley Geezer | Page 6 Alexanderby Shane Elks | Page “Lexi” 16 Walker LoBiondo EventsPage 8 in Your Area Cheapby Ellen Gurley Momma’s | Page 18 Guide Spinnerby Seth Peagle Rack | Page 11 Truckby Ellen Gurley Stalking | Page 19 Letter From the Editor Hello, Charlotte. This is My City Magazine. We are delighted to be celebrating the first issue of print. Thank you for picking up a copy. We are committed to keeping you abreast of the happenings in your city in an artsy not fartsy fashion via news, reviews, interviews and viewpoints. - We have columnists who act as mouthpieces for every aspect of Charlotte culture; art, food, beer, music, fash ion, comics, neighbourhoods, theatre, alternative lifestyle, raising families and home improvement. We hope you enjoy My City as much as we delight in bringing it to you. Thank you for your warm reception. Sincerely, Ellen Gurley [email protected] | 704.575.6611 | P.O. Box 5606, Charlotte, NC 28299 THE MY CITY MAGAZINE TEAM John Hairston, Jr. Seth Peagler Marc “El Guapo” Jacksina Greggory Bradford Ellen “LNMental” Gurley Ray “About Your House” Terry Alex Barnette Austin Caine Shane “Mr. Red” Elks Jennifer Davis Clairsean “Babe” Alexander-Floyd Liz Eagle Bill “The Thrill” Cleveland and the one and only Erin Tracy-Blackwood My City Staff My City Staff SETH PEAGLER | Columnist - In 2003, Seth Peagler received a B.A. -
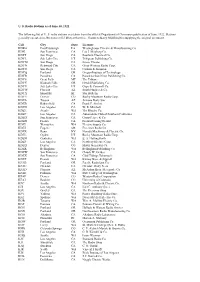
U. S. Radio Stations As of June 30, 1922 the Following List of U. S. Radio
U. S. Radio Stations as of June 30, 1922 The following list of U. S. radio stations was taken from the official Department of Commerce publication of June, 1922. Stations generally operated on 360 meters (833 kHz) at this time. Thanks to Barry Mishkind for supplying the original document. Call City State Licensee KDKA East Pittsburgh PA Westinghouse Electric & Manufacturing Co. KDN San Francisco CA Leo J. Meyberg Co. KDPT San Diego CA Southern Electrical Co. KDYL Salt Lake City UT Telegram Publishing Co. KDYM San Diego CA Savoy Theater KDYN Redwood City CA Great Western Radio Corp. KDYO San Diego CA Carlson & Simpson KDYQ Portland OR Oregon Institute of Technology KDYR Pasadena CA Pasadena Star-News Publishing Co. KDYS Great Falls MT The Tribune KDYU Klamath Falls OR Herald Publishing Co. KDYV Salt Lake City UT Cope & Cornwell Co. KDYW Phoenix AZ Smith Hughes & Co. KDYX Honolulu HI Star Bulletin KDYY Denver CO Rocky Mountain Radio Corp. KDZA Tucson AZ Arizona Daily Star KDZB Bakersfield CA Frank E. Siefert KDZD Los Angeles CA W. R. Mitchell KDZE Seattle WA The Rhodes Co. KDZF Los Angeles CA Automobile Club of Southern California KDZG San Francisco CA Cyrus Peirce & Co. KDZH Fresno CA Fresno Evening Herald KDZI Wenatchee WA Electric Supply Co. KDZJ Eugene OR Excelsior Radio Co. KDZK Reno NV Nevada Machinery & Electric Co. KDZL Ogden UT Rocky Mountain Radio Corp. KDZM Centralia WA E. A. Hollingworth KDZP Los Angeles CA Newbery Electric Corp. KDZQ Denver CO Motor Generator Co. KDZR Bellingham WA Bellingham Publishing Co. KDZW San Francisco CA Claude W. -

Broadcast Loc Alism Hearinq 101 So You Local Artists Will Have to Forgive
I Broadcast Loc alism Hearinq 101 I I So you local artists will have to forgive me if we haven't had the time to take on the responsibility of launching your music career. (Applause.1 Ms. Merritt, you seem to contradict youreelf a little bit when you say that you don't want the government to be involved with radio, yet you're asking an ever- growing, ever-expanding federal government to mandate the play of your records on radio stations. MS. MERRITT: I certainly am ngt indicating that. T.J.: And you say that the radio stations shouldn't be worried about their bottom line when you openly admit that that's what you're trying to reach is your bottom MS. MERRITT: I'm not -- if you want music, you're to have to find a way, we're going to have to find'a way to cooperate because we both need to atay in business. But, you know, I certainly don't live by a pool. I struggle to make ends meet and I have a lot of respect for that. So I'm not here to promote my career. I'm here to give North Carolina musicians a voice so that they can keep ibuting just as you have. (Applause. T.J.: Do her comments count in my two minutes? say this, I know this will be indecent language to a lot of people in here, but ours is a society built on capitalism. And in order to make a profit, you have to abide by the rules of capitalism. -

WDAV's News Box Editor - for the First Time in Its 141 Mi -»* >K Ibflfltf9 Hbhhl "^^^^^^^^^^^^^^Rb^B Bydennismclawhorn Year History, Davidson College Newseditor "*
B^BBBB^HBBVHiflBBHflVHfeBWBkflBB^fllflVJBiBBBk LXVII, Volume Number TWO Davidson College,Davidson. N.C. 28036 September 15, 1978 Code *" College Httfej? '- -rma HK 4j closes - H^HHMHMRW readied J^BaH^BBnflKTsHffnK ByDONALDCALDWELL Asst. « I B^KfllflH bVMEHM^B^BB^BBB^b1 WDAV's News box Editor - For the first time in its 141 mi -»* >k IBflfltf9 HBHHl "^^^^^^^^^^^^^^rb^b ByDENNISMCLAWHORN year history, Davidson College NewsEditor "* . - may soonhave acomprehensive— ■mHbVbmHbTJbT^ When WDAV Publications Director Rob Payne went to the Codeof Faculty Evaluation. post office to pick up the station's mail Saturday morning, he In last Friday's scheduled PMBHMNHH ' found the box not only empty,but closed. meeting, S m&^^mMf - Upon officials, the Professional Af- fHHI m^BmXzfr-bhbbkmbV tA B^BwWiB questioningpostal WDAV staff members fairs Committee (PAC) consi- ■ t *■■*_"* discovered thatMarthaRoberts, Assistant Director of Communi- s 1 afl Rr ' - dered and recommended further BBk 4t ■ HLu. im^bL v cations had closed the post office box Fridav afternoon. W yBBTJ^B^Bi^BM Bite, in the proposedCode. fltfttt. According to General Mana- about how it looked from the This draft,the document's ' ger Carrington Thompson, the pbst office point of view and icond, is being revised by / v^^^B^B^B^BI ©Hii WDAV staff was not notified tianges '■# >a$iAXSviiH^9v3^BEBfiCEBiEM Br '^iNHHHMOTII^B decided to have all the mail cademic Vice-President and delivered to the College's Com- Dean of Faculty Price Zimmer- see munications Department. mann and was to be focus released * * "Students getting t B * ■'■ this morning. ' a* ■■■- **,,■ - mbbbMHbVi- pp. -

Wsge 91.7 Fm
Your Independent Music Source WSGE 91.7 FM WSGE 91.7 FM is the best-kept marketing secret in the region. Our listeners are your clients, customers, patrons and employees. About the Station WSGE’s mission is to provide distinctive WSGE’s eclectic music programming music and information programming appeals to a growing audience of more designed to stimulate, educate and than 31,000 listeners per week. Many tune entertain. WSGE will serve in the public’s in for our award-winning Carolina Beach/ interest, advancing the educational goals Shag music, while others enjoy our Rock, of Gaston College by providing a unique Rhythm & Blues, Highway 321 Blues, Jazz alternative to commercial broadcasting or Gospel. in Gaston, Mecklenburg and surrounding counties. WSGE is a noncommercial public radio station that gives back to the community WSGE has stayed consistent with its roots by supporting organizations such as the dating back to 1980. It’s an independent United Way of Gaston County, The House voice that doesn’t shy away from taking of Mercy, The Community Foundation of creative risks. Whether digging deep into Gaston County, Gastonia Downtown a music genre, breaking the latest songs, Development Association and others. Also, or making local and regional music the station annually coordinates Socks for accessible with friendly commentary, it’s Seniors, which collects socks, gloves and definitely the station for curious minds. toiletries for people in need during the Central to this dynamic mix is music and holiday season. news programming from National Public Radio. More information is available at 704.922.2251 Benefits of Corporate Support Strategic Marketing Partnership Underwriting FAQ Focused on Your Goals Q. -

FCC Delays WDAV License Renewal
FCC delays WDAV license renewal By PHILIP DUNCAN FCC said that an expectation isn't "Indicators are very good that Lawrimore discussed the pro- $18,000 will go for salaries and News Editor enough, that we must have actual we will go on the air in the fall." jected costs: "The transmitter $10,000 for general operating pledges." Lawrimore has been working on and antenna system will cost expenses. The total is, according The Federal Communications "Getting pledges at this early plans for the actual operation of about $50,000—this is essential to to Lawrimore, "extremely low, in Commission is holding up David- stage would take too much time," the station after the expected FCC get on the air with high power. comparison to other educational son College's application to renew Lawrimore explained, so an alter- approval is granted. "$21,000 will go for improve- stations' budgets." the license of radio station nate route will be proposed in "I drew up a five-page proposal ments in the studio, considerable WDAV. order to meet FCC regulations. summarizing what we proposed to improvement in classical records See rotated editorial, "The application is being held "We will show that the college and tapes, miscellaneous elec- page 4 up for four reasons," said Director' has liquid assets sufficient to tronic parts, and maintenance The proposal describes five of News and Photography Earl finance the radio station. equipment. potential sources of revenue for W. Lawrimore. "We haven't changed plans— "The 'automation option' is still the radio station. The first is a "First, they (the FCC) say we will still raise money for the listed at $36,000, but no decision direct fund-raising drive. -

Gaston County ECA Standing Rules
Gaston County Extension and Community Association (ECA) STANDING RULES Article I. Name ......................................................................................................................................... 2 Article II. Mission ..................................................................................................................................... 2 Article III. Code of Conduct ..................................................................................................................... 2 Article IV. Membership Requirements ..................................................................................................... 3 Article V. Organizational Structure .......................................................................................................... 4 Section 1. Executive Board ................................................................................................................... 5 Section 2. President ............................................................................................................................... 6 Section 3. Vice President ..................................................................................................................... 6 Section 4. Secretary ............................................................................................................................. 7 Section 5. Treasurer ............................................................................................................................. 8 Section -

CRRA/Carolinamls Membership Roster April 2015 1 Copyright
CRRA/CarolinaMLS Membership Roster April 2015 # 2539 #1 Properties of Lake Norman 218001 1st Choice Properties 268 Farmstead Ln. 13663 Providence Rd., Ste. 233 Mooresville, NC 28117 704-662-9698 Weddington, NC 28104 951-965-6460 Fax: 866-396-9163 Fax: 704-749-2008 38811 Cherry, Linda L 704-662-9698 * 27121 Wickham, Cheri Ann 951-965-6460 52918 Jonnes, Norman 704-662-9698 * 15428 Lynch, Cathy E 704-662-9698 98615 Lynch, David Eugene 704-200-6393 2180 1st Choice Properties, Inc. 44902 Ogburn II, John Fred 704-662-9698 7427 Matthews Mint Hill Road Charlotte, NC 28227 704-650-5707 1 Fax: 704-749-2364 5167 10th Avenue Realty 82189 Alvarez, Jesus Salvador 704-650-5707 3048 Streamhaven Dr * 28737 Granger, Anna A 704-650-5707 IndianLand, SC 29707 704-770-6825 24180 Granger, John C 704-650-5707 Fax: 888-216-0292 80667 Rodgers III, Master Willard 704-770-6825 2 * 51667 Rodgers, Dawn Hall 704-770-6825 6012 24/7 Realty Corporation 11527 Watermoss Ln Charlotte, NC 28262 704-587-3998 3546 121 Realty LLC Fax: 704-587-0077 3901 Etheredge Street Indian Trail, NC 28079 704-641-4663 * 26601 Morris Sr, Daniel Clarence 704-587-3998 67575 Morris, Denise Sandra 704-587-3998 * 93546 Hefner, Annette Helms 704-641-4663 3 4331 3 D Realty, Inc. 248 Grandview Drive 6322 123 My New Home Statesville, NC 28677 704-528-6455 401 East Blvd Ste. 210 Fax: 704-528-6411 Charlotte, NC 28203-5151 980-721-1832 Fax: 704-973-0660 * 43310 DiDomenico, Kim Darlene 704-528-6455 34746 Casad, Katherine Leigh 980-721-1832 40026 Escontrias, Amber L 980-721-1832 8973 365 Realty Inc 32779 -

Pursuant to N.C.G.S
Annual Report of the Charitable Solicitation Licensing Section May 1, 2000 – June 30, 2001 North Carolina Department of the Secretary of State Elaine F. Marshall, Secretary Charitable Solicitation Licensing Section Post Office Box 29622 Raleigh, North Carolina 27626-0622 E-Mail Address: csl @sosnc.gov 919-814-5400 North Carolina Department of the Secretary of State 2000-2001 Charitable Solicitation Licensing Annual Report -- Page 1 of 204 The North Carolina Department of the Secretary of State does not discriminate on the basis of race, color, national origin, sex, religion, age or disability in the employment or the provision of services. North Carolina Department of the Secretary of State 2000-2001 Charitable Solicitation Licensing Annual Report -- Page 2 of 204 Pursuant to N.C.G.S. 131F-30, this report contains the following: 1. A summary of complaints, investigations and enforcement actions related to solicitation activities; 2. A list of charitable or sponsor organizations on file; 3. A list of charitable or sponsor organizations who chose to submit an audited financial statement; 4. A list of professional fundraisers who are or have been licensed in the past five years; and 5. A Detailed Summary of 2000-2001 Solicitor Activities in North Carolina. North Carolina Department of the Secretary of State 2000-2001 Charitable Solicitation Licensing Annual Report -- Page 3 of 204 A Summary of complaints, investigations and enforcement actions related to solicitation activities: During the period between July 1, 2000 and June 30, 2001, the Department conducted 18 investigations of alleged violations of the Statute. Two of those investigations found violations and a civil penalty was assessed in each case. -
State of the Media: Audio Today a Focus on Public Radio December 2014
STATE OF THE MEDIA: AUDIO TODAY A FOCUS ON PUBLIC RADIO DECEMBER 2014 STATE OF THE MEDIA: AUDIO TODAY Q4 Copyright © 2014 The Nielsen Company 1 THE ECLECTIC AUDIO LANDSCAPE In today’s fragmented media world, where consumers have more choices and more access to content than ever before, audio remains strong. 91.3% of all Americans (age 12+) are using radio during the week. Since the beginning of 2010, the national weekly radio audience has grown from 239.7 million to 243 million listeners tuning in across more than 250 local markets in every corner of the country. 243 MILLION AMERICANS LISTEN TO RADIO EACH WEEK In a time of changing habits and new digital platforms, radio’s consistent audience numbers are quite remarkable. With the holidays just around the corner, consumers will be turning to the radio to catch their favorite sounds of the season or stay in touch with what’s happening in their local community each day. PUBLIC RADIO OFFERS AN UNCOMMON MIX OF PROGRAMMING FOR 32 MILLION LISTENERS This year we have profiled the overall radio landscape, multicultural audiences and network radio listeners, and for our final report we turn our attention to Public Radio; the more than 900 rated stations which offer an eclectic mix of news, entertainment, music and cultural programming in markets large and small. Public Radio is a unique and relevant part of the lives of 32 million Americans and exists in large part due to the financial support of the listeners we examine in the following pages. Source: RADAR 123, December 2014; M-SU MID-MID, Total