Control Practices for Delivering Direct Student Support Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

COVID-19 Guidance on Cloth Face Masks This Document Provides Guidance on Best Practices for the Use of Nonmedical Face Masks, Considering COVID-19
COVID-19 Guidance on Cloth Face Masks This document provides guidance on best practices for the use of nonmedical face masks, considering COVID-19. Currently, institutions have varying guidelines and Water Mission has taken these under advisement to produce recommendations for the ministry. Each country program should make sure to comply with national and local guidance, if stricter guidelines are in enforced. Water Mission Recommendations Taking into consideration current guidelines provided by the World Health Organization (WHO), the Center for Disease Control (CDC) (see Appendix 1) and other research, Water Mission makes the following recommendations for the use of cloth face masks in relation to COVID-19. Category Minimum Requirements When to use a face • Water Mission recommends the use of cloth face masks according to the mask risk level in each country program (see table below). o As of 4/27/20, ALL STAFF ARE REQUIRED TO WEAR APPROVED FACE MASKS AT ALL TIMES Approved face • Two-layer cloth face masks (see specifications below) masks • Single-use nonmedical face masks Provision of face • All Water Mission staff should be provided with five (5) cloth face masks masks per person (plus laundry soap for washing) • If using single-use face masks, Water Mission staff should be provided with two (2) face masks per person, per day Face mask training • All staff members must be trained on proper face mask use and management (click link for training presentation) Proper face mask • Wash hands with water and soap, or use alcohol-based hand -

Universal PPE Guidelines and Faqs (As of August 2, 2021)
Universal PPE Guidelines and FAQs (as of August 2, 2021) Guidance was issued on July 27, 2021, by the Centers for Disease Control and Prevention (CDC) that raises concerns of increased COVID-19 transmission due to the Delta variant. As a result, in alignment with the CDC, Nebraska Medicine is making modifications to the Universal PPE Guidelines to support the increasing numbers of COVID-19 cases in the community. Vaccination remains the most effective way to prevent transmission of disease and is the only way to prevent severe illness with risk of hospitalization and death. Guidance will be updated and/or expanded based on the level of community spread of COVID- 19, the proportion of the population that is fully vaccinated, the rapidly evolving science on COVID-19 vaccines, the understanding of COVID-19 variants and employee health data related to COVID-19 exposure. For the purposes of this document, people are considered fully vaccinated after receiving the full series of the following COVID-19 vaccines: Pfizer/BioNTech, Astrazeneca-SK Bio, Serum Institute of India, Johnson and Johnson (J&J/Janseen), Moderna, Novavax, Sinovac, and Sinopharm Key Points Applicable for ALL Nebraska Medicine Sites: Regardless of vaccination status: o Masks will be required in all clinical settings. o Masks will be required whenever a colleague is indoors in the presence of a patient and/or visitor. o Masks must be doffed and discarded when leaving a droplet/contact precautions isolation room. A new mask must be donned by the colleague immediately after leaving this type of isolation. When masks are used for droplet precautions, the mask becomes contaminated during patient encounters via large droplet particle transmission. -
Bsl-2 Enhanced Work Practices for Specimen Processing and Cell Culture
BSL-2 ENHANCED WORK PRACTICES FOR SPECIMEN PROCESSING AND CELL CULTURE [email protected] 4/1/21 [CA] Sleeve covers should be used for coats with uncuffed sleeves • BSC should be certified annually and have a current certification sticker attached. Ensure that the samples are coded and labeled in a way that identifies their contents to the laboratory. The lab must implement an easy to understand tracking system to discriminate live from inactive material. This could be different colored tubes, colored labels (“cryodots”), colored sharpies etc. Maintain your inventory in a secure manner. 1 • Prepare fresh 10% bleach in water each day. Label with date • Add concentrated bleach to aspiration flasks before use (add 10% of final volume). • Media should turn pink to clear on contact Do not use this waste bag for items that can puncture a red bag (e.g. pipette tips, serological pipettes) •A plastic beaker can also be used instead and can also be used to collect pipette tips and serological pipettes. Rinse these once with bleach in beaker •Dispose by decanting 10% bleach down drain •Pipette tips and serological pipettes are transferred to a sharps container Content generously shared by Yale University EH&S The Association for Biosafety and Biosecurity Considerations for Handling Potential SARS-CoV-2 Samples BSL2 BSL2 with BSL3 practices BSL3 ● Whole blood, serum and urine ● Aliquoting and/or diluting specimens ● Virus isolation/propagation in cell culture and initial ● Synthetic messenger RNA-based or recombinant protein-based products ● Inoculating -

LEO Facemasks-050820.Pdf
1-877-897-6646 Lands’ End Business helps your brand succeed with quality business and uniform apparel, legendary service and real value. Cotton Cloth Face Mask Style 521006 Color White Price $14.85/3pack These are designed to be used when FDA masks (e.g., N95 surgical masks) are not available. Not intended as Personal Protective Equipment (PPE)* - 3-ply 100% cotton, 4 oz Jersey knit - Anti-microbial fabric finish - Machine wash separately in cold water. Use only non-chlorine bleach if needed. Tumble dry low. Do not use fabric softener. Do not iron. Wash dark colors separately. May be washed up to 20 times. - Imported This fabric is OEKO-TEX® certified. 7” Relaxed Approx 3.5” Extended Approx 4.5” .375” 3.5” 7” .375” Poly/Cotton Cloth Face Mask Style 521005 Colors White, Light Blue, Royal Blue, Navy Blue, Gray Price $7.50/3pack These are designed to be used when FDA masks (e.g., N95 surgical masks) are not available. Not intended as Personal Protective Equipment (PPE)* - Fabric: 2-ply 65% polyester/35% cotton, 4.3 oz poplin - Machine wash separately in warm water. Tumble dry low. Do not use fabric softener. Do not iron. Wash dark colors separately. May be washed up to 75 times. - Imported This mask is OEKO-TEX® Standard 100 certified. 4” Pleats .5” Open upwards 6.5” Relaxed Approx 3” 8” Extended Approx 4” .25” BioSmart® is a patented Milliken® technology that binds chlorine in the wash cycle. BioSmart® garments must be washed in a bleach cycle to charge the fabric with chlorine initially, and to recharge during each wash. -
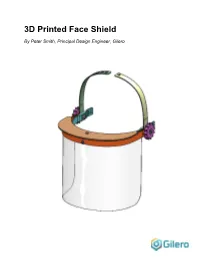
3D Printed Face Shield by Peter Smith, Principal Design Engineer, Gilero
3D Printed Face Shield By Peter Smith, Principal Design Engineer, Gilero This face shield design is based on an open source design by HanochH on Thingiverse. Changes were to make the design more robust. This design uses a number of 3D printed parts. The prototype was printed in PETG on a Fusion3. It also uses the following: • One (1) 12” x 7” sheet of PET clear film, 0.010 – 0.020” thick (or a cut up 2L soda bottle) • Two (2) ¼-20 x 5/8” long Hex Head Screws (with 7/16” across the flats of the hex head) • Two (2) ¼-20 Hex Nuts (with 7/16” across the flats) • Two (2) #6 x ½” long button head sheet metal screws • Ten inches of ¼” braided elastic or similar The above are commonly available in any hardware store or from online vendors such as McMaster-Carr: www.mcmaster.com Tools required for assembly: • Phillips screwdriver (#1 or #2) • Box cutter or sharp knife • Pair of household scissors Step 1. Print all parts using the supplied STL files. Note that 2 copies of the thumbnut will be needed. Press the nuts into the thumbnut printed parts. Press the Hex Head Screws into the recesses in the blue part shown and through the holes in the other parts as shown. Screw the assembled thumbnuts onto the Hex Head Screws to hold the assembly together. Step 2. Secure the cap with one of the #6 sheet metal screws. Step 3. Slip the visor into the gap in the orange part shown until it butts up to the cap. -

OHA's Mask, Face Covering, and Face Shield Requirements for Health Care
OFFICE OF THE DIRECTOR Kate Brown, Governor 500 Summer St NE E20 Salem OR 97301 Voice: 503-947-2340 Date: June 30,2021 Fax: 503-947-2341 Mask, Face Covering, and Face Shield Requirements for Health Care Offices While the Governor has rescinded many of the Executive Orders, the declaration of emergency remains in effect and masks are still required in health care settings. See Executive Order 21-15. In addition, health care offices must continue to follow all applicable state and federal regulatory requirements related to masking, including Oregon-OSHA rules addressing COVID-19 workplace risks. Authority: ORS 433.441, ORS 433.443, ORS 431A.010 and ORS 431A.015 Applicability: These requirements apply to: • All health care personnel in health care offices, as defined below. • All patients and visitors in health care offices, as defined below. Definitions: • “Face covering” means a cloth, polypropylene, paper or other face covering that covers the nose and the mouth and that rests snugly above the nose, below the mouth, and on the sides of the face. • “Face mask” means a medical grade mask. • “Face shield” means a clear plastic shield that covers the forehead, extends below the chin, and wraps around the sides of the face. • “Healthcare Personnel (HCP)” means all paid and unpaid persons serving in healthcare offices who have the potential for direct or indirect exposure to patients or infectious materials, including body substances (e.g., blood, tissue, and specific body fluids); contaminated medical supplies, devices, and equipment; contaminated -

The Challenge of Performing Mastoidectomy Using The
The challenge of performing mastoidectomy using the operating microscope with COVID-19 personal protective equipment (PPE) Philip Clamp1 and Stephen Broomfield1 1University Hospitals Bristol and Weston NHS Foundation Trust May 19, 2020 Abstract Objective: As an aerosol generating procedure (AGP), mastoidectomy in the COVID-19 era requires healthcare workers to wear personal protective equipment (PPE); UK guidelines recommend an FFP-3 mask and full-face visor. The aim of this study was to examine the effect of wearing PPE on the view achieved using the operating microscope. Methods: Using the operating microscope, ENT surgeons were asked to view a target so that it filled the entire operating field. The distance between the surgeon's eye and the microscope was recorded and subsequently measured with the surgeon wearing a range of PPE. In each PPE condition, surgeons scored the visibility of the target; scores were used to calculate the visible area of the surgical field. Results: Eleven surgeons took part, generating 51 eye-microscope and target-view scores. Distance from the eye to the microscope inversely correlated with diameter and area visible (Pearson correlation coefficient -0.983 and -0.894 respectively; p<0.001). Use of PPE increased the eye-microscope distance and reduced the surgical view. The median area visible wearing the FFP-3 mask and full-face visor was 4% (range 4 { 16%). Conclusion: PPE consisting of an FFP-3 mask and full-face visor is incompatible with use of the operating microscope, with less than 10% of the surgical field visible in most cases. Solutions that allow for concurrent use of the operating microscope and drill during mastoid surgery are urgently required so that surgeons are adequately protected from COVID-19 transmission. -

IFRC Guidance on the Generalised Use of Cloth Face Masks During the COVID-19 Pandemic
IFRC guidance on the generalised use of cloth face masks during the COVID-19 pandemic Background The use of medical masks1, respirators2 and other face coverings is a widely discussed intervention in the response to COVID-19. There is no strong evidence either in favour of or against the widescale use of masks by members of the general public. WHO’s recommendation is that medical personal protective equipment (PPE) such as medical masks and respirators should be reserved for two categories of people: 1) people involved in the care of suspected and confirmed COVID-19 cases, and 2) people who are suspected of or confirmed to have COVID-19. Current evidence supports droplet and contact transmission of COVID-19 in standard settings, whereas in health facilities, the virus can be aerosolised during certain procedures, e.g. intubation and ventilation, therefore presenting a higher risk of transmission. Respirators are needed for high-risk healthcare activities (i.e. aerosol-generating procedures), and medical masks are required as a general precaution in healthcare settings where COVID-19 cases may be present. Healthcare workers and other frontline workers are also at heightened risk for illness and death from COVID-19 due to their repeated exposure to infectious patients. From the health worker perspective, lack of PPE can lead to anxiety and fear of seeing sick patients, and may lead to attrition of staff, which has been seen in some countries. Additionally, without the availability of respirators, health workers may face a dilemma when faced with patients whose treatment would require aerosol generating procedures, potentially increasing fatalities. -

Facemasks in the Protection of Hospitals
FACEMASKS IN THE PROTECTION OF HOSPITALS HEALTHCARE WORKERS (HCW) IN RESOURCE POOR SETTINGS Dr. Abrar Ahmad Chughtai This thesis is in fulfilment of the requirements for the degree of Doctor of Philosophy School of Public Health and Community Medicine UNSW Medicine May 2015 1 THE UNIVERSITY OF NEW SOUTH WALES Thesis/Dissertation Sheet Surname or Fam1ly name Chughta1 F1rst name Abrar Other name/s Ahmad Abbreviation for degree as g1ven m the Umvers1ty calendar PhD School Public Health and Commun1ty Medicine Faculty Medicine T1tle Facemasks m the protection of hosp1tals healthcare workers (HCWs) in resource poor settings Abstract 350 words maximum: (PLEASE TYPE) Currently there is an ongoing debate and a dearth of evidence around the efficacy of facemasks and respirators. Most studies have been observational and there is a lack of trial data around use and re-use of facemasks in the healthcare setting. Due to the lack of high quality studies, I hypothesised that there would be huge variations in the policies and practices around the use of facemasks and respirators in the healthcare setting. This thesis therefore aims to examine the policies and practices around the use of these products in low resource countries. Five studies were conducted at varying administrative levels. In the first study, publicly available policies and guidelines around the use of facemasks/respirators were examined to describe areas of consistency, as well as gaps in the recommendations. In the second study, infection control stakeholders were interviewed from China, Pakistan and Vietnam to further explore the issues, which arose during the guideline review. Next, hospitals from the three countries were surveyed to examine practices around the use of facemasks/ respirators and to examine the translation of policies into practice. -
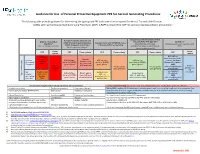
Guidance for Use of PPE for Aerosol Generating Procedures (PDF)
Guidance for Use of Personal Protective Equipment PPE for Aerosol Generating Procedures The following table provides guidance for determining the appropriate PPE and room criteria required for Aerosol Transmissible Diseases 1 (ATDs) when performing Aerosol Generating Procedures (AGP). A PAPR is required for AGP for patients requiring airborne precautions. Droplet transmitted infections2 that Has signs/symptoms consistent with Airborne transmitted are part of the ATD Standard All Others5 COVID-19 and undergoing evaluation, Asymptomatic with COVID-19 status infections2 (e.g. influenza, adenovirus) (Including patients with negative COVID COVID-19 exposed, or confirmed unknown and/or test pending (e.g. TB, measles, varicella) excludes RSV, rhinovirus, parainfluenza, tests) (Novel respiratory isolation)3 human metapneumovirus Room 3 Room PPE PPE Room criteria PPE Room criteria PPE Room criteria PPE criteria criteria N95 with eye PAPR and 6 protection (or PAPR) refer to Airborne Aerosol N95 with face N95 with face N95 with eye recommended plus isolation Isolation room Generating shield (or PAPR), shield (or PAPR), protection (or PAPR), Standard Precautions table for continuous 4 4 Procedure gown, gloves gown, gloves gown, gloves AND Airborne AGP preferred Private Private patient Private patient refer to isolation table Isolation patient room room preferred room preferred as applicable room not Use Standard 7 Not PAPR or N95 Surgical mask necessary N95 with face Private patient Surgical mask Precautions aerosol and refer to with eye Type of -

Face Shields; Health Care Personnel; Hospital Purchasing Departments and Distributors; And, Any Other Stakeholders
April 13, 2020 To: Manufacturers of Face Shields; Health Care Personnel; Hospital Purchasing Departments and Distributors; and, Any Other Stakeholders On April 9, 2020, the U.S. Food and Drug Administration (FDA) issued an Emergency Use Authorization (EUA) in response to concerns relating to insufficient supply and availability of face shields1 for use by health care personnel (HCP) as personal protective equipment (PPE) in healthcare settings in accordance with CDC recommendations to cover the front and sides of the face and provide barrier protection during the Coronavirus Disease 2019 (COVID-19) pandemic. On April 13, 2020, in response to questions from stakeholders regarding the authorization process, and having concluded that revising the April 9, 2020, EUA is appropriate to protect the public health or safety under section 564(g)(2)(c) of the Act (21 U.S.C. 360bbb-3(g)(2)(c)), FDA is reissuing the April 9, 2020, letter in its entirety with an amendment incorporated to clarify that this letter of authorization, as posted and publicly announced on FDA’s website at https://www.fda.gov/medical-devices/emergency-situations-medical-devices/emergency-use- authorizations#covid19ppe, serves as face shield manufacturers’ notification of authorization. As stated in the April 9, 2020 letter, manufacturers of authorized face shields do not need to take any action, other than complying with the Conditions of Authorization (Section IV) in this letter of authorization, to be an authorized face shield under this EUA if the face shield is within -

Face Shield and Headgear (FSU1610HB3) SOLUTIONS for MEDICAL PROVIDERS and FIRST RESPONDERS
Face Shield and Headgear (FSU1610HB3) SOLUTIONS FOR MEDICAL PROVIDERS AND FIRST RESPONDERS FEATURES • Shields eyes and face from fluid, sprays and splashes • Easy to put on and take off when time is critical • Transparent shield with headgear, strap and optional foam strip • For use with goggles or glasses • Flexible headgear contours to forehead • With anti-fog • Option for replacement shields for head gear • Disposable or reusable* • Shipped in individual poly bags • Lightweight • Non-sterile SPECS • FSU1610HB3 (unassembled kit) • Shield thickness: 15 mil/0.015 in • Shield dimensions: 16 in W x 9.45 in H • Shield material: PET • Headgear material: Injection-molded polypropylene • Foam material: Polyurethane Foam • Strap material: Synthetic (Non Latex) Polyisoprene • Manufactured in North America For more information contact [email protected] PLEASE NOTE • This product has NOT been FDA cleared or approved. • This product has been authorized by FDA under an Emergency Use Authorization for use by healthcare providers as personal protective equipment. • This product is only authorized for the duration of the declaration that circumstances justifying the authorization of emergency use under Section 564(b)(1) of the Act, 21 USC 360bbb-3(b)(1) unless the authorization is terminated or revoked sooner. CAUTION • This product is NOT intended for use in presence of high intensity light source or flammable gas. • This product is NOT sterilized. • Use of this face shield alone will NOT prevent infection from microbes or viruses. Shown with foam added *Cleaning/disinfecting instructions listed on reverse side of document Face Shield and Headgear CLEANING AND DISINFECTING INSTRUCTIONS • To clean and disinfect, use a Health Canada authorized hard-surface disinfectant.