The Pennsylvania State University the Graduate School STUDYING DIVERTICULAR DISEASE USING FAMILIAL BASED NEXT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of Nlrs in the Regulation of Type I Interferon Signaling, Host Defense and Tolerance to Inflammation
International Journal of Molecular Sciences Review Role of NLRs in the Regulation of Type I Interferon Signaling, Host Defense and Tolerance to Inflammation Ioannis Kienes 1, Tanja Weidl 1, Nora Mirza 1, Mathias Chamaillard 2 and Thomas A. Kufer 1,* 1 Department of Immunology, Institute for Nutritional Medicine, University of Hohenheim, 70599 Stuttgart, Germany; [email protected] (I.K.); [email protected] (T.W.); [email protected] (N.M.) 2 University of Lille, Inserm, U1003, F-59000 Lille, France; [email protected] * Correspondence: [email protected] Abstract: Type I interferon signaling contributes to the development of innate and adaptive immune responses to either viruses, fungi, or bacteria. However, amplitude and timing of the interferon response is of utmost importance for preventing an underwhelming outcome, or tissue damage. While several pathogens evolved strategies for disturbing the quality of interferon signaling, there is growing evidence that this pathway can be regulated by several members of the Nod-like receptor (NLR) family, although the precise mechanism for most of these remains elusive. NLRs consist of a family of about 20 proteins in mammals, which are capable of sensing microbial products as well as endogenous signals related to tissue injury. Here we provide an overview of our current understanding of the function of those NLRs in type I interferon responses with a focus on viral infections. We discuss how NLR-mediated type I interferon regulation can influence the development of auto-immunity and the immune response to infection. Citation: Kienes, I.; Weidl, T.; Mirza, Keywords: NOD-like receptors; Interferons; innate immunity; immune regulation; type I interferon; N.; Chamaillard, M.; Kufer, T.A. -

Interoperability in Toxicology: Connecting Chemical, Biological, and Complex Disease Data
INTEROPERABILITY IN TOXICOLOGY: CONNECTING CHEMICAL, BIOLOGICAL, AND COMPLEX DISEASE DATA Sean Mackey Watford A dissertation submitted to the faculty at the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Gillings School of Global Public Health (Environmental Sciences and Engineering). Chapel Hill 2019 Approved by: Rebecca Fry Matt Martin Avram Gold David Reif Ivan Rusyn © 2019 Sean Mackey Watford ALL RIGHTS RESERVED ii ABSTRACT Sean Mackey Watford: Interoperability in Toxicology: Connecting Chemical, Biological, and Complex Disease Data (Under the direction of Rebecca Fry) The current regulatory framework in toXicology is expanding beyond traditional animal toXicity testing to include new approach methodologies (NAMs) like computational models built using rapidly generated dose-response information like US Environmental Protection Agency’s ToXicity Forecaster (ToXCast) and the interagency collaborative ToX21 initiative. These programs have provided new opportunities for research but also introduced challenges in application of this information to current regulatory needs. One such challenge is linking in vitro chemical bioactivity to adverse outcomes like cancer or other complex diseases. To utilize NAMs in prediction of compleX disease, information from traditional and new sources must be interoperable for easy integration. The work presented here describes the development of a bioinformatic tool, a database of traditional toXicity information with improved interoperability, and efforts to use these new tools together to inform prediction of cancer and complex disease. First, a bioinformatic tool was developed to provide a ranked list of Medical Subject Heading (MeSH) to gene associations based on literature support, enabling connection of compleX diseases to genes potentially involved. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

NOD-Like Receptors in the Eye: Uncovering Its Role in Diabetic Retinopathy
International Journal of Molecular Sciences Review NOD-like Receptors in the Eye: Uncovering Its Role in Diabetic Retinopathy Rayne R. Lim 1,2,3, Margaret E. Wieser 1, Rama R. Ganga 4, Veluchamy A. Barathi 5, Rajamani Lakshminarayanan 5 , Rajiv R. Mohan 1,2,3,6, Dean P. Hainsworth 6 and Shyam S. Chaurasia 1,2,3,* 1 Ocular Immunology and Angiogenesis Lab, University of Missouri, Columbia, MO 652011, USA; [email protected] (R.R.L.); [email protected] (M.E.W.); [email protected] (R.R.M.) 2 Department of Biomedical Sciences, University of Missouri, Columbia, MO 652011, USA 3 Ophthalmology, Harry S. Truman Memorial Veterans’ Hospital, Columbia, MO 652011, USA 4 Surgery, University of Missouri, Columbia, MO 652011, USA; [email protected] 5 Singapore Eye Research Institute, Singapore 169856, Singapore; [email protected] (V.A.B.); [email protected] (R.L.) 6 Mason Eye Institute, School of Medicine, University of Missouri, Columbia, MO 652011, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-573-882-3207 Received: 9 December 2019; Accepted: 27 January 2020; Published: 30 January 2020 Abstract: Diabetic retinopathy (DR) is an ocular complication of diabetes mellitus (DM). International Diabetic Federations (IDF) estimates up to 629 million people with DM by the year 2045 worldwide. Nearly 50% of DM patients will show evidence of diabetic-related eye problems. Therapeutic interventions for DR are limited and mostly involve surgical intervention at the late-stages of the disease. The lack of early-stage diagnostic tools and therapies, especially in DR, demands a better understanding of the biological processes involved in the etiology of disease progression. -

Cellular and Molecular Signatures in the Disease Tissue of Early
Cellular and Molecular Signatures in the Disease Tissue of Early Rheumatoid Arthritis Stratify Clinical Response to csDMARD-Therapy and Predict Radiographic Progression Frances Humby1,* Myles Lewis1,* Nandhini Ramamoorthi2, Jason Hackney3, Michael Barnes1, Michele Bombardieri1, Francesca Setiadi2, Stephen Kelly1, Fabiola Bene1, Maria di Cicco1, Sudeh Riahi1, Vidalba Rocher-Ros1, Nora Ng1, Ilias Lazorou1, Rebecca E. Hands1, Desiree van der Heijde4, Robert Landewé5, Annette van der Helm-van Mil4, Alberto Cauli6, Iain B. McInnes7, Christopher D. Buckley8, Ernest Choy9, Peter Taylor10, Michael J. Townsend2 & Costantino Pitzalis1 1Centre for Experimental Medicine and Rheumatology, William Harvey Research Institute, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, Charterhouse Square, London EC1M 6BQ, UK. Departments of 2Biomarker Discovery OMNI, 3Bioinformatics and Computational Biology, Genentech Research and Early Development, South San Francisco, California 94080 USA 4Department of Rheumatology, Leiden University Medical Center, The Netherlands 5Department of Clinical Immunology & Rheumatology, Amsterdam Rheumatology & Immunology Center, Amsterdam, The Netherlands 6Rheumatology Unit, Department of Medical Sciences, Policlinico of the University of Cagliari, Cagliari, Italy 7Institute of Infection, Immunity and Inflammation, University of Glasgow, Glasgow G12 8TA, UK 8Rheumatology Research Group, Institute of Inflammation and Ageing (IIA), University of Birmingham, Birmingham B15 2WB, UK 9Institute of -

ATP-Binding and Hydrolysis in Inflammasome Activation
molecules Review ATP-Binding and Hydrolysis in Inflammasome Activation Christina F. Sandall, Bjoern K. Ziehr and Justin A. MacDonald * Department of Biochemistry & Molecular Biology, Cumming School of Medicine, University of Calgary, 3280 Hospital Drive NW, Calgary, AB T2N 4Z6, Canada; [email protected] (C.F.S.); [email protected] (B.K.Z.) * Correspondence: [email protected]; Tel.: +1-403-210-8433 Academic Editor: Massimo Bertinaria Received: 15 September 2020; Accepted: 3 October 2020; Published: 7 October 2020 Abstract: The prototypical model for NOD-like receptor (NLR) inflammasome assembly includes nucleotide-dependent activation of the NLR downstream of pathogen- or danger-associated molecular pattern (PAMP or DAMP) recognition, followed by nucleation of hetero-oligomeric platforms that lie upstream of inflammatory responses associated with innate immunity. As members of the STAND ATPases, the NLRs are generally thought to share a similar model of ATP-dependent activation and effect. However, recent observations have challenged this paradigm to reveal novel and complex biochemical processes to discern NLRs from other STAND proteins. In this review, we highlight past findings that identify the regulatory importance of conserved ATP-binding and hydrolysis motifs within the nucleotide-binding NACHT domain of NLRs and explore recent breakthroughs that generate connections between NLR protein structure and function. Indeed, newly deposited NLR structures for NLRC4 and NLRP3 have provided unique perspectives on the ATP-dependency of inflammasome activation. Novel molecular dynamic simulations of NLRP3 examined the active site of ADP- and ATP-bound models. The findings support distinctions in nucleotide-binding domain topology with occupancy of ATP or ADP that are in turn disseminated on to the global protein structure. -

TITLE PAGE Oxidative Stress and Response to Thymidylate Synthase
Downloaded from molpharm.aspetjournals.org at ASPET Journals on October 2, 2021 -Targeted -Targeted 1 , University of of , University SC K.W.B., South Columbia, (U.O., Carolina, This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. The final version may differ from this version. This article has not been copyedited and formatted. -
Supplementary File 2A Revised
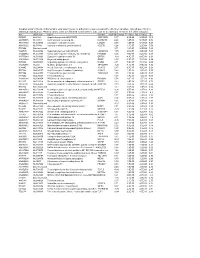
Supplementary file 2A. Differentially expressed genes in aldosteronomas compared to all other samples, ranked according to statistical significance. Missing values were not allowed in aldosteronomas, but to a maximum of five in the other samples. Acc UGCluster Name Symbol log Fold Change P - Value Adj. P-Value B R99527 Hs.8162 Hypothetical protein MGC39372 MGC39372 2,17 6,3E-09 5,1E-05 10,2 AA398335 Hs.10414 Kelch domain containing 8A KLHDC8A 2,26 1,2E-08 5,1E-05 9,56 AA441933 Hs.519075 Leiomodin 1 (smooth muscle) LMOD1 2,33 1,3E-08 5,1E-05 9,54 AA630120 Hs.78781 Vascular endothelial growth factor B VEGFB 1,24 1,1E-07 2,9E-04 7,59 R07846 Data not found 3,71 1,2E-07 2,9E-04 7,49 W92795 Hs.434386 Hypothetical protein LOC201229 LOC201229 1,55 2,0E-07 4,0E-04 7,03 AA454564 Hs.323396 Family with sequence similarity 54, member B FAM54B 1,25 3,0E-07 5,2E-04 6,65 AA775249 Hs.513633 G protein-coupled receptor 56 GPR56 -1,63 4,3E-07 6,4E-04 6,33 AA012822 Hs.713814 Oxysterol bining protein OSBP 1,35 5,3E-07 7,1E-04 6,14 R45592 Hs.655271 Regulating synaptic membrane exocytosis 2 RIMS2 2,51 5,9E-07 7,1E-04 6,04 AA282936 Hs.240 M-phase phosphoprotein 1 MPHOSPH -1,40 8,1E-07 8,9E-04 5,74 N34945 Hs.234898 Acetyl-Coenzyme A carboxylase beta ACACB 0,87 9,7E-07 9,8E-04 5,58 R07322 Hs.464137 Acyl-Coenzyme A oxidase 1, palmitoyl ACOX1 0,82 1,3E-06 1,2E-03 5,35 R77144 Hs.488835 Transmembrane protein 120A TMEM120A 1,55 1,7E-06 1,4E-03 5,07 H68542 Hs.420009 Transcribed locus 1,07 1,7E-06 1,4E-03 5,06 AA410184 Hs.696454 PBX/knotted 1 homeobox 2 PKNOX2 1,78 2,0E-06 -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Depicting Gene Co-Expression Networks Underlying Eqtls Nathalie Vialaneix, Laurence Liaubet, Magali San Cristobal
Depicting gene co-expression networks underlying eQTLs Nathalie Vialaneix, Laurence Liaubet, Magali San Cristobal To cite this version: Nathalie Vialaneix, Laurence Liaubet, Magali San Cristobal. Depicting gene co-expression networks underlying eQTLs. Haja N. Kadarmideen. Systems Biology in Animal Production and Health vol 2, 2, Springer International Publishing, pp.1-31, 2016, 978-3-319-43330-1. 10.1007/978-3-319-43332-5_1. hal-01390589 HAL Id: hal-01390589 https://hal.archives-ouvertes.fr/hal-01390589 Submitted on 2 Nov 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Depicting gene co-expression networks underlying eQTLs Nathalie Villa-Vialaneix, Laurence Liaubet and Magali SanCristobal Abstract Deciphering the biological mechanisms underlying a list of genes whose expression is under partial genetic control (i.e., having at least one eQTL) may not be as easy as for a list of differential genes. Indeed, no specific phenotype (e.g., health or production phenotype) is linked to the list of transcripts under study. There is a need to find a coherent biological interpretation of a list of genes under (partial) genetic control. We propose a pipeline using appropriate statistical tools to build a co-expression network from the list of genes, then to finely depict the network structure. -

Whole Genome Sequencing of Familial Non-Medullary Thyroid Cancer Identifies Germline Alterations in MAPK/ERK and PI3K/AKT Signaling Pathways
biomolecules Article Whole Genome Sequencing of Familial Non-Medullary Thyroid Cancer Identifies Germline Alterations in MAPK/ERK and PI3K/AKT Signaling Pathways Aayushi Srivastava 1,2,3,4 , Abhishek Kumar 1,5,6 , Sara Giangiobbe 1, Elena Bonora 7, Kari Hemminki 1, Asta Försti 1,2,3 and Obul Reddy Bandapalli 1,2,3,* 1 Division of Molecular Genetic Epidemiology, German Cancer Research Center (DKFZ), D-69120 Heidelberg, Germany; [email protected] (A.S.); [email protected] (A.K.); [email protected] (S.G.); [email protected] (K.H.); [email protected] (A.F.) 2 Hopp Children’s Cancer Center (KiTZ), D-69120 Heidelberg, Germany 3 Division of Pediatric Neurooncology, German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), D-69120 Heidelberg, Germany 4 Medical Faculty, Heidelberg University, D-69120 Heidelberg, Germany 5 Institute of Bioinformatics, International Technology Park, Bangalore 560066, India 6 Manipal Academy of Higher Education (MAHE), Manipal, Karnataka 576104, India 7 S.Orsola-Malphigi Hospital, Unit of Medical Genetics, 40138 Bologna, Italy; [email protected] * Correspondence: [email protected]; Tel.: +49-6221-42-1709 Received: 29 August 2019; Accepted: 10 October 2019; Published: 13 October 2019 Abstract: Evidence of familial inheritance in non-medullary thyroid cancer (NMTC) has accumulated over the last few decades. However, known variants account for a very small percentage of the genetic burden. Here, we focused on the identification of common pathways and networks enriched in NMTC families to better understand its pathogenesis with the final aim of identifying one novel high/moderate-penetrance germline predisposition variant segregating with the disease in each studied family. -

Open Data for Differential Network Analysis in Glioma
International Journal of Molecular Sciences Article Open Data for Differential Network Analysis in Glioma , Claire Jean-Quartier * y , Fleur Jeanquartier y and Andreas Holzinger Holzinger Group HCI-KDD, Institute for Medical Informatics, Statistics and Documentation, Medical University Graz, Auenbruggerplatz 2/V, 8036 Graz, Austria; [email protected] (F.J.); [email protected] (A.H.) * Correspondence: [email protected] These authors contributed equally to this work. y Received: 27 October 2019; Accepted: 3 January 2020; Published: 15 January 2020 Abstract: The complexity of cancer diseases demands bioinformatic techniques and translational research based on big data and personalized medicine. Open data enables researchers to accelerate cancer studies, save resources and foster collaboration. Several tools and programming approaches are available for analyzing data, including annotation, clustering, comparison and extrapolation, merging, enrichment, functional association and statistics. We exploit openly available data via cancer gene expression analysis, we apply refinement as well as enrichment analysis via gene ontology and conclude with graph-based visualization of involved protein interaction networks as a basis for signaling. The different databases allowed for the construction of huge networks or specified ones consisting of high-confidence interactions only. Several genes associated to glioma were isolated via a network analysis from top hub nodes as well as from an outlier analysis. The latter approach highlights a mitogen-activated protein kinase next to a member of histondeacetylases and a protein phosphatase as genes uncommonly associated with glioma. Cluster analysis from top hub nodes lists several identified glioma-associated gene products to function within protein complexes, including epidermal growth factors as well as cell cycle proteins or RAS proto-oncogenes.