National Formulary Part I
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anaesthesia and Past Use Of
177 Correspondence were using LSD. It is more popular than other commonly Anaesthesia and past use of used hallucinogens whose quoted incidence of clients are: LSD ketamine 0.1% (super-K/vitamin K.I), psilocybin and psilocin 0.6% (the active alkaloids in the Mexican "magic To the Editor: mushroom"), and 3,4 methylenedioxymethamphetamine We report the case of a 43-yr-old lady who was admitted ~MDMA" 1% (ecstasy). The effects of the concurrent to the Day Surgery Unit for release of her carpal tunnel ingestion of LSD on anaesthesia are well described. 2-4 retinaculum. During the preoperative visit, she reported The long-term effects of the past use of LSD are largely no intercurrent illnesses, drug therapy or allergies. She unknown. We wonder if the hallucinations experienced did say, however, that she was frightened of general anaes- by our patient during anaesthesia were due to her LSD thesia, since she had experienced terrifying dreams during intake many years before. We would be interested to surgery under general anaesthesia on three occasions dur- know if others have had experience anaesthetising patients ing the previous ten years. On further questioning, she who are past users of phencyclidine-derived drugs. admitted that she had used lysergic acid diethylamide (LSD) during the late 1960's, the last occasion being 1968 Geoffrey N. Morris MRCGPFRCA when she had experienced characterstic hallucinations. Patrick T. Magee MSe FRCA She had not experienced hallucinations in the ensuing Anaesthetic Department years, except on the surgical occasions mentioned. Royal United Hospital One of the three previous operations had been per- Combe Park formed at our hospital and the anaesthetic record was Bath BA1 3NG checked. -

NH Healthy Families Preferred Drug List (PDL) Is the List of Covered Drugs
Pharmacy Program NH Healthy Families is committed to providing appropriate, high quality, and cost effective drug therapy to all NH Healthy Families members. NH Healthy Families works with providers and pharmacists to ensure that medications used to treat a variety of conditions and diseases are covered. NH Healthy Families covers prescription medications and certain over-the-counter (OTC) medications when ordered by a practitioner. The pharmacy program does not cover all medications. Some medications require prior authorization (PA) or have limitations on age, dosage, and maximum quantities. Preferred Drug List The NH Healthy Families Preferred Drug List (PDL) is the list of covered drugs. The PDL applies to drugs members can receive at retail pharmacies. The NH Healthy Families PDL is continually evaluated by the NH Healthy Families Pharmacy and Therapeutics (P&T) Committee to promote the appropriate and cost- effective use of medications. The Committee is composed of the NH Healthy Families Medical Director, NH Healthy Families Pharmacy Director, and several New Hampshire physicians, pharmacists, and other healthcare professionals. Pharmacy Benefit Manager NH Healthy Families works with Envolve Pharmacy Solutions to process pharmacy claims for prescribed drugs. Some drugs on the NH Healthy Families PDL may require PA, and Envolve Pharmacy Solutions is responsible for administering this process. Envolve Pharmacy Solutions is our Pharmacy Benefit Manager (PBM). Specialty Drugs NH Healthy Families contracts with a number of specialty pharmacies, such as AcariaHealth Specialty Pharmacy, to ensure members have adequate access to the specialty drugs they require. Specialty drugs, such as biopharmaceuticals and injectables, may require PA to be approved for payment by NH Healthy Families. -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

Conceptual Model for Using Imidazoline Derivative Solutions in Pulpal Management
Journal of Clinical Medicine Review Conceptual Model for Using Imidazoline Derivative Solutions in Pulpal Management Robert S. Jones Division of Pediatric Dentistry, Department of Developmental & Surgical Sciences, School of Dentistry, University of Minnesota, Minneapolis, MN 55455, USA; [email protected] Abstract: Alpha-adrenergic agonists, such as the Imidazoline derivatives (ImDs) of oxymetazoline and xylometazoline, are highly effective hemostatic agents. ImDs have not been widely used in dentistry but their use in medicine, specifically in ophthalmology and otolaryngology, warrants consideration for pulpal hemostasis. This review presents dental healthcare professionals with an overview of ImDs in medicine. ImD solutions have the potential to be more effective and biocompatible than existing topical hemostatic compounds in pulpal management. Through a comprehensive analysis of the pharmacology of ImDs and the microphysiology of hemostasis regulation in oral tissues, a conceptual model of pulpal management by ImD solutions is presented. Keywords: hemostasis; alpha-adrenergic agonists; imidazoline; oxymetazoline; nasal; dental pulp; mucosa; apexogenesis; pulpotomy; direct pulp cap; dentistry 1. Overview Citation: Jones, R.S. Conceptual The purpose of this review is to formulate a conceptual model on the potential man- Model for Using Imidazoline agement of pulpal tissue by imidazoline derivatives (ImDs) based on a review of the Derivative Solutions in Pulpal literature that examines the hemostatic properties and mechanistic actions of these com- Management. J. Clin. Med. 2021, 10, 1212. https://doi.org/10.3390/ pounds in other human tissues. Commercial ImDs are formulated in solution with an- jcm10061212 timicrobial preservatives in order to act as ‘parenteral topical agents’ and used to manage ophthalmic inflammation, nasal congestion, and to control bleeding during otolaryngology Academic Editor: Rosalia surgery [1,2]. -

ZANTAC® 150 (Ranitidine Hydrochloride) Tablets, USP
PRESCRIBING INFORMATION ZANTAC® 150 (ranitidine hydrochloride) Tablets, USP ZANTAC® 300 (ranitidine hydrochloride) Tablets, USP ZANTAC® 25 (ranitidine hydrochloride effervescent) ® EFFERdose Tablets ® ZANTAC (ranitidine hydrochloride) Syrup, USP DESCRIPTION The active ingredient in ZANTAC 150 Tablets, ZANTAC 300 Tablets, ZANTAC 25 EFFERdose Tablets, and ZANTAC Syrup is ranitidine hydrochloride (HCl), USP, a histamine H2-receptor antagonist. Chemically it is N[2-[[[5-[(dimethylamino)methyl]-2 furanyl]methyl]thio]ethyl]-N′-methyl-2-nitro-1,1-ethenediamine, HCl. It has the following structure: The empirical formula is C13H22N4O3S•HCl, representing a molecular weight of 350.87. Ranitidine HCl is a white to pale yellow, granular substance that is soluble in water. It has a slightly bitter taste and sulfurlike odor. Each ZANTAC 150 Tablet for oral administration contains 168 mg of ranitidine HCl equivalent to 150 mg of ranitidine. Each tablet also contains the inactive ingredients FD&C Yellow No. 6 Aluminum Lake, hypromellose, magnesium stearate, microcrystalline cellulose, titanium dioxide, triacetin, and yellow iron oxide. Each ZANTAC 300 Tablet for oral administration contains 336 mg of ranitidine HCl equivalent to 300 mg of ranitidine. Each tablet also contains the inactive ingredients croscarmellose sodium, D&C Yellow No. 10 Aluminum Lake, hypromellose, magnesium stearate, microcrystalline cellulose, titanium dioxide, and triacetin. 1 ZANTAC 25 EFFERdose Tablets for oral administration is an effervescent formulation of ranitidine that must be dissolved in water before use. Each individual tablet contains 28 mg of ranitidine HCl equivalent to 25 mg of ranitidine and the following inactive ingredients: aspartame, monosodium citrate anhydrous, povidone, and sodium bicarbonate. Each tablet also contains sodium benzoate. -
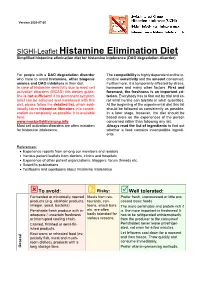
SIGHI-Leaflet Histamine Elimination Diet Simplified Histamine Elimination Diet for Histamine Intolerance (DAO Degradation Disorder)
Version 2020-07-20 SIGHI-Leaflet Histamine Elimination Diet Simplified histamine elimination diet for histamine intolerance (DAO degradation disorder) For people with a DAO degradation disorder The compatibility is highly dependent on the in- who have to avoid histamine, other biogenic dividual sensitivity and the amount consumed. amines and DAO inhibitors in their diet. Furthermore, it is temporarily affected by stress, In case of histamine sensitivity due to mast cell hormones and many other factors. First and activation disorders (MCAD) this dietary guide- foremost, the freshness is an important cri- line is not sufficient! If no permanent symptom terion. Everybody has to find out by trial and er- relief can be achieved and maintained with this ror what he/she can tolerate in what quantities. diet, please follow the detailed list, which addi- At the beginning of the experimental diet this list tionally takes histamine liberators into consid- should be followed as consistently as possible. eration as completely as possible. It is available In a later stage, however, the diet should be here: based more on the experiences of the person www.mastzellaktivierung.info concerned rather than following any list. Mast cell activation disorders are often mistaken Always read the list of ingredients to find out for histamine intolerance. whether a food contains incompatible ingredi- ents. References: • Experience reports from among our members and readers • Various patient leaflets from doctors, clinics and hospitals • Experience of other patient organizations, bloggers, forum threads etc. • Scientific publications • Textbooks and cookbooks about histamine intolerance To avoid: ? Risky: Well tolerated: Fermented or microbially ripened Meals from res- Prefer fresh, unprocessed or little pro- products (e.g. -

2D6 Substrates 2D6 Inhibitors 2D6 Inducers
Physician Guidelines: Drugs Metabolized by Cytochrome P450’s 1 2D6 Substrates Acetaminophen Captopril Dextroamphetamine Fluphenazine Methoxyphenamine Paroxetine Tacrine Ajmaline Carteolol Dextromethorphan Fluvoxamine Metoclopramide Perhexiline Tamoxifen Alprenolol Carvedilol Diazinon Galantamine Metoprolol Perphenazine Tamsulosin Amiflamine Cevimeline Dihydrocodeine Guanoxan Mexiletine Phenacetin Thioridazine Amitriptyline Chloropromazine Diltiazem Haloperidol Mianserin Phenformin Timolol Amphetamine Chlorpheniramine Diprafenone Hydrocodone Minaprine Procainamide Tolterodine Amprenavir Chlorpyrifos Dolasetron Ibogaine Mirtazapine Promethazine Tradodone Aprindine Cinnarizine Donepezil Iloperidone Nefazodone Propafenone Tramadol Aripiprazole Citalopram Doxepin Imipramine Nifedipine Propranolol Trimipramine Atomoxetine Clomipramine Encainide Indoramin Nisoldipine Quanoxan Tropisetron Benztropine Clozapine Ethylmorphine Lidocaine Norcodeine Quetiapine Venlafaxine Bisoprolol Codeine Ezlopitant Loratidine Nortriptyline Ranitidine Verapamil Brofaramine Debrisoquine Flecainide Maprotline olanzapine Remoxipride Zotepine Bufuralol Delavirdine Flunarizine Mequitazine Ondansetron Risperidone Zuclopenthixol Bunitrolol Desipramine Fluoxetine Methadone Oxycodone Sertraline Butylamphetamine Dexfenfluramine Fluperlapine Methamphetamine Parathion Sparteine 2D6 Inhibitors Ajmaline Chlorpromazine Diphenhydramine Indinavir Mibefradil Pimozide Terfenadine Amiodarone Cimetidine Doxorubicin Lasoprazole Moclobemide Quinidine Thioridazine Amitriptyline Cisapride -

Comparative Effects of Cimetidine and Famotidine on the Vagally Stimulated Acid Secretion in the Isolated Mouse Whole Stomach
Comparative Effects of Cimetidine and Famotidine on the Vagally Stimulated Acid Secretion in the Isolated Mouse Whole Stomach Kazuo Watanabe1, Shingo Yano1, Masayuki Yamamoto1 and Shoko Kanaoka2 1Laboratory of Chemical Pharmacology, Department of Drug Evaluation and Toxicological Sciences, Faculty of Pharmaceutical Sciences, Chiba University, 1-33, Yayoi-cho, Inage-ku, Chiba 263, Japan 2Research Institute for Wakan-Yaku, Toyama Medical and Pharmaceutical University, Toyama 930-01, Japan Received July 15, 1992 Accepted December 10, 1992 ABSTRACT-We investigated the effects of cimetidine and famotidine on the acid secretory response to elec trical vagal stimulation, bethanechol and histamine in the isolated mouse whole stomach preparation. The acid secretion elicited by electrical vagal stimulation at the position of the esophagus (10 Hz, 0.3 msec, 10 V for 5 min) was reproducible by repeated stimulation in each preparation, and it was abolished by tetrodo toxin, atropine and hexamethonium. This vagally stimulated acid secretion was abolished by cimetidine (3 mM), while it was only partly inhibited by famotidine (10-100 ƒÊM). Histamine (100 ƒÊM)-induced acid secre tion was inhibited by cimetidine and famotidine, and the doses of these drugs required for complete inhibi tion were 3 mM and 10 ƒÊM, respectively. In contrast, bethanechol (10 ƒÊM)-induced acid secretion was slight ly reduced by famotidine (1-100 ƒÊM), but markedly reduced by cimetidine (3 mM). In the guinea pig ileum, millimolar concentrations of cimetidine and famotidine shifted the dose-response curve of the contractile response to acetylcholine rightward. These findings suggest that the inhibitory effect of cimetidine on the vagally stimulated or bethanechol-induced acid secretion is elicited at least partly through mechanisms different from H2-antagonism. -

Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients Research Questions: 1. How many schizophrenia patients are prescribed recommended first-line second-generation treatments for schizophrenia? 2. How many schizophrenia patients switch to an injectable antipsychotic after stabilization on an oral antipsychotic? 3. How many schizophrenia patients are prescribed 2 or more concomitant antipsychotics? 4. Are claims for long-acting injectable antipsychotics primarily billed as pharmacy or physician administered claims? 5. Does adherence to antipsychotic therapy differ between patients with claims for different routes of administration (oral vs. long-acting injectable)? Conclusions: In total, 4663 schizophrenia patients met inclusion criteria, and approximately 14% of patients (n=685) were identified as treatment naïve without claims for antipsychotics in the year before their first antipsychotic prescription. Approximately 45% of patients identified as treatment naïve had a history of remote antipsychotic use, but it is unclear if antipsychotics were historically prescribed for schizophrenia. Oral second-generation antipsychotics which are recommended as first-line treatment in the MHCAG schizophrenia algorithm were prescribed as initial treatment in 37% of treatment naive patients and 28% of all schizophrenia patients. Recommended agents include risperidone, paliperidone, and aripiprazole. Utilization of parenteral antipsychotics was limited in patients with schizophrenia. Overall only 8% of patients switched from an oral to an injectable therapy within 6 months of their first claim. Approximately, 60% of all schizophrenia patients (n=2512) had claims for a single antipsychotic for at least 12 continuous weeks and may be eligible to transition to a long-acting injectable antipsychotic. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

Medicines That Affect Fluid Balance in the Body
the bulk of stools by getting them to retain liquid, which encourages the Medicines that affect fluid bowels to push them out. balance in the body Osmotic laxatives e.g. Lactulose, Macrogol - these soften stools by increasing the amount of water released into the bowels, making them easier to pass. Older people are at higher risk of dehydration due to body changes in the ageing process. The risk of dehydration can be increased further when Stimulant laxatives e.g. Senna, Bisacodyl - these stimulate the bowels elderly patients are prescribed medicines for chronic conditions due to old speeding up bowel movements and so less water is absorbed from the age. stool as it passes through the bowels. Some medicines can affect fluid balance in the body and this may result in more water being lost through the kidneys as urine. Stool softener laxatives e.g. Docusate - These can cause more water to The medicines that can increase risk of dehydration are be reabsorbed from the bowel, making the stools softer. listed below. ANTACIDS Antacids are also known to cause dehydration because of the moisture DIURETICS they require when being absorbed by your body. Drinking plenty of water Diuretics are sometimes called 'water tablets' because they can cause you can reduce the dry mouth, stomach cramps and dry skin that is sometimes to pass more urine than usual. They work on the kidneys by increasing the associated with antacids. amount of salt and water that comes out through the urine. Diuretics are often prescribed for heart failure patients and sometimes for patients with The major side effect of antacids containing magnesium is diarrhoea and high blood pressure. -

THE USE of MIRTAZAPINE AS a HYPNOTIC O Uso Da Mirtazapina Como Hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa
ARTIGO ESPECIAL THE USE OF MIRTAZAPINE AS A HYPNOTIC O uso da mirtazapina como hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa Prescription of approved hypnotics for insomnia decreased by more than 50%, whereas of antidepressive agents outstripped that of hypnotics. However, there is little data on their efficacy to treat insomnia, and many of these medications may be associated with known side effects. Antidepressants are associated with various effects on sleep patterns, depending on the intrinsic pharmacological properties of the active agent, such as degree of inhibition of serotonin or noradrenaline reuptake, effects on 5-HT1A and 5-HT2 receptors, action(s) at alpha-adrenoceptors, and/or histamine H1 sites. Mirtazapine is a noradrenergic and specific serotonergic antidepressive agent that acts by antagonizing alpha-2 adrenergic receptors and blocking 5-HT2 and 5-HT3 receptors. It has high affinity for histamine H1 receptors, low affinity for dopaminergic receptors, and lacks anticholinergic activity. In spite of these potential beneficial effects of mirtazapine on sleep, no placebo-controlled randomized clinical trials of ABSTRACT mirtazapine in primary insomniacs have been conducted. Mirtazapine was associated with improvements in sleep on normal sleepers and depressed patients. The most common side effects of mirtazapine, i.e. dry mouth, drowsiness, increased appetite and increased body weight, were mostly mild and transient. Considering its use in elderly people, this paper provides a revision about studies regarding mirtazapine for sleep disorders. KEYWORDS: sleep; antidepressive agents; sleep disorders; treatment� A prescrição de hipnóticos aprovados para insônia diminuiu em mais de 50%, enquanto de antidepressivos ultrapassou a dos primeiros.