EXTREME HEAT TOOLKIT a Planning Guide for Public Health and Emergency Response Professionals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hazard Criteria
NWS San Diego All-Hazard Reference Guide Warnings and Advisories are issued 12 to 48 hours in advance. Watches are issued when warning level conditions are forecast within the next 36 to 48 hours, or up to 72 hours with high confidence. High Winds/Blowing Dust Blowing High Wind Dust Storm Region Wind Advisory Dust Warning Warning Advisory Coastal and Sustained ≥ 30 mph Sustained ≥ 40 mph Visibility Visibility Valley areas or gust ≥ 35 mph gust ≥ 58 mph ¼ to 1 mile <¼ mile Mountains and Sustained ≥ 35 mph Sustained ≥ 45 mph Visibility Visibility Deserts or gust ≥ 40 mph or gust ≥ 58 mph ¼ to 1 mile <¼ mile < 7000 feet Mountains Sustained ≥ 40 mph Sustained ≥ 40 mph Visibility Visibility > 7000 feet or gust ≥ 55 mph or gust ≥ 75 mph ¼ to 1 mile <¼ mile Winter Weather Winter Winter Blizzard Wind Chill Wind Chill Region Weather Storm Warning Advisory Warning Advisory Warning 4-8” in Sustained winds Wind Chill 12” in 12 hours, Wind Chill Mountains 12 hours, > 35 mph and Temperatures 18” in 24 hours, Temperatures > 7000 feet or 8-12” in visibility <¼ mile from High Impact < -20 ◦F 24 hours in blowing snow -10 to -20 ◦F 3-6” in Sustained winds Wind Chill Mountains 8” in 12 hours, Wind Chill 12 hours, > 35 mph and Temperatures 3000 to 12” in 24 hours, Temperatures 4-8” in visibility <¼ mile from 7000 feet High Impact < -20 ◦F 24 hours in blowing snow -10 to -20 ◦F Other areas 1-4” in Sustained winds Wind Chill including 4” in 12 hours, Wind Chill 12 hours, > 35 mph and Temperatures High 6” in 24 hours, Temperatures 3-6” in visibility <¼ mile -

Inclement Weather Guidelines for Outdoor Events
INCLEMENT WEATHER GUIDELINES FOR OUTDOOR EVENTS “Inclement weather” is a generic term often used to describe weather conditions that are either unsafe or undesirable for outdoor events. Inclement weather can come in many different forms, as outlined below. This guideline is intended to be used as a tool to help you identify when forecasted or actual weather conditions require cancelling or postponing an event. NOTE: This checklist addresses only the most unsafe weather conditions. Your own event guidelines may dictate actions for other weather conditions that may be undesirable (e.g. rainy, too warm, too cold). Should any of the following triggers occur or become forecasted for the time of the event, the event should be cancelled or, when appropriate, temporarily postponed for safety reasons. Temporarily postponing an event means just waiting a few minutes until the immediate hazard passes, if your schedule allows. When in doubt about what to do, consult with FSU Emergency Management for decision support. ADVANCED NOTICE TRIGGER TO CANCEL EVENT: TRIGGER TO TEMPORARILY POSTPONE TIMEFRAME EVENT: 0 ‐ 48 Hours [ ] Hurricane or Tropical Storm Watch [ ] Winter Storm Watch 0 ‐ 24 Hours [ ] Heat Advisory or Excessive Heat Watch [ ] High Wind Watch [ ] Winter Weather Advisory [ ] Wind Chill Advisory 0 ‐ 12 Hours [ ] Tornado Watch [ ] Severe Thunderstorm Watch [ ] Flash Flood Watch [ ] Excessive Heat Warning [ ] Wind Advisory During Event [ ] Observed Heat Index in excess of 108’F. [ ] FSU ALERT issued for Tornado Warning, Severe Thunderstorm Warning, Flash Flood Warning or [ ] Observed Wind Chill less than 0’F. Lightning Warning. [ ] Observed winds in excess of 35 miles per hour. [ ] Significant Weather Advisory (no FSU ALERT). -

Heat Advisory Guidelines
HACIENDA LA PUENTE UNIFIED SCHOOL DISTRICT OFFICE OF STUDENT AND FAMILY SERVICES 15959 E. GALE AVENUE • CITY OF INDUSTRY, CA 91716 Heat Advisory Precautions for Schools I. GUIDELINES FOR DAILY ACTIVITIES Extreme heat events are characterized by stagnant, warm air masses and consecutive nights with high temperatures. An extreme heat event, or heat wave, is a prolonged period of excessively hot weather, which may be accompanied by high humidity. In times of extreme heat, a heat advisory will be sent from the district office in coordination with the Los Angeles County Office of Education. Otherwise the principal should monitor the heat index on days when heat will be an issue. The heat index is determined by temperature and relative humidity. A. Heat index of 95+ degrees - No outside activities B. Heat index of 90-94 degrees – Limited outside activities 1. Maintain clear focus on supervising students and looking for signs of over-heating 2. Mandatory water breaks every 30 minutes. 3. Mandatory breaks from activities after the water break for 5 to10 minutes in duration. 4. Monitor heat index every 30 minutes C. Heat index of 89 degrees or below – standard protocol REMEMBER: IN TIMES OF EXTREME HEAT, STUDENTS WITH OUTDOOR ACTIVITIES SHOULD BE HYDRATED OFTEN THROUGHOUT THE DAY. II. RATIONALE Our Heat Advisory Precautions are designed to protect students from incurring heat related illnesses or problems. This is a guide for school personnel to use and refer to when making decisions about modifying and/or suspending outdoor activities. The best defense against heat-related conditions is prevention. Staff shall be reminded yearly and in times of extreme heat regarding precautions to take to ensure student safety. -

REFERENCE SHEET for NWS TAUNTON WARNING/ADVISORY THRESHOLDS (Last Updated: March 7, 2017)
REFERENCE SHEET FOR NWS TAUNTON WARNING/ADVISORY THRESHOLDS (Last Updated: March 7, 2017) The following are National Weather Service criteria for issuing Watches/Warnings/Advisories: Watches: 50% confidence of meeting Warning criteria (generally within 36-48+ hours). Advisories and Warnings: 80% confidence in the event occurrence (generally within 24-36 hours). TYPE OF ISSUANCE WHEN ISSUED FOR SOUTHERN NEW ENGLAND WINTER WEATHER ADVISORY More than one predominant hazard Winter weather event having more than one predominant hazard (ie., snow and ice, snow and sleet, or snow, ice & sleet) meeting or exceeding advisory criteria for at least one of the precipitation elements, but remaining below warning criteria. Snow, Ocean Effect Snow, and/or Sleet 3 inches averaged over a forecast zone in 12 hours Snow and Blowing Snow Sustained or frequent gusts of 25 to 34 mph accompanied by falling and blowing snow occasionally reducing visibility to ≤ 1/4 mile for ≥ 3 hours Blowing Snow Widespread or localized blowing snow reducing visibility to ≤ ¼ mile with winds < 35 mph Black Ice A Special Weather Statement will usually be issued when sufficient moisture is expected to cause a thin layer of ice on road surfaces, typically on cloudless nights (“black ice”). At forecaster discretion a formal Winter Weather Advisory may be issued instead. FREEZING RAIN ADVISORY Any accretion of freezing rain or freezing drizzle on road surfaces WIND CHILL ADVISORY Wind chill index between -15°F and -24°F for at least 3 hours using only the sustained wind WINTER STORM WARNING More than one predominant hazard Winter weather event having more than one predominant hazard {ie. -

Assessment of NOAA National Weather Service Methods to Warn for Extreme Heat Events
JANUARY 2017 H A W K I N S E T A L . 5 Assessment of NOAA National Weather Service Methods to Warn for Extreme Heat Events MICHELLE D. HAWKINS,VANKITA BROWN, AND JANNIE FERRELL NOAA/National Weather Service, Silver Spring, Maryland (Manuscript received 27 May 2015, in final form 8 August 2016) ABSTRACT Recent climate studies have predicted a future with longer, more intense, and more frequent heat events. Evolving challenges presented by this paradigm necessitate an assessment of current efforts to warn for extreme heat events. NOAA’s National Weather Service (NWS) Weather Forecast Offices (WFOs) issue Excessive Heat Watch, Excessive Heat Warning, and Heat Advisory products as conditions warrant. In the fall of 2013 the NWS conducted an internal assessment with its WFOs to 1) document variations in the usage of heat-based watch, warning, and advisory hazard messages (products) across the country; 2) learn about the degree to which locally developed criteria are applied to forecaster decision-making processes in issuing these products; and 3) gather ideas for enhancing communication of expected excessive heat events in general. Survey responses indicate that WFOs selectively use one or a combination of products, and that various methodologies are used to develop criteria for issuing heat products. Given that forecasters use meteoro- logical and nonmeteorological factors when deciding to issue heat products, forecaster judgment is a crucial element of the warning process. Results also revealed partner confusion due to inconsistent heat product issuance criteria. Suggestions were made for eliminating or revising existing products and policies, or creating new products, policies, or issuance criteria. -

Spearfish Fire Department Policies and Procedures
SPEARFISH FIRE DEPARTMENT POLICIES AND PROCEDURES Page 1 of 5 Volume: Operation Section: 20.00 Number: 20.09 Subject: Weather Watches, Warnings, Advisory’s and Spotter Activation Date Issued: 8 August 2019 Originator: Assistant Chief R. Mathis Rescinds: 28 March 2017 Approval: Assistant Chief R. Mathis I. Purpose This procedure provides guidance for safety and general procedures when responding to Weather Spotter activations. II. SCOPE This policy applies to all personnel. III. DEFINITIONS Winter Storm Watch A Winter Storm Watch is issued when there is the potential for significant and hazardous winter weather within 48 hours. It does not mean that significant and hazardous winter weather will occur...it only means it is possible. Significant and hazardous winter weather is defined as a combination of: 1) 5 inches or more of snow/sleet within a 12-hour period or 7 inches or more of snow/sleet within a 24-hour period AND/OR 2) Enough ice accumulation to cause damage to trees or powerlines AND/OR 3) a life threatening or damaging combination of snow and/or ice accumulation with wind. Blizzard Warning A Blizzard Warning means that the following conditions are occurring or expected within the next 12 to 18 hours. 1) Snow and/or blowing snow reducing visibility to 1/4 mile or less for 3 hours or longer AND 2) Sustained winds of 35 mph or greater or frequent gusts to 35 mph or greater. There is no temperature requirement that must be met to achieve blizzard conditions. Winter Storm Warning A Winter Storm Warning is issued when a significant combination of hazardous winter weather is occurring or imminent. -

Minnesota Extreme Heat Toolkit
MINNESOTA EXTREME HEAT TOOLKIT Minnesota Climate and Health Program Minnesota Department of Health Environmental Impacts Analysis Unit Acknowledgments The Minnesota Extreme Heat Toolkit was made possible through funding from cooperative agreement 5UE1EH000738 from the Centers for Disease Control and Prevention (CDC) and the commitment of many individuals who contributed their time and expertise to its development. The information and resources contained within the toolkit benefited substantially from the input of various local and national experts. Two specific groups spent considerable time reviewing content and providing expert feedback into the development of the Extreme Heat Toolkit: the Extreme Heat Training Module Technical Team and the Extreme Heat Toolkit Steering Committee. We would like to acknowledge and thank the participants who provided advice, resources and review of the toolkit: Pam Blixt, Emergency Preparedness Manager, Minneapolis Department of Health and Family Support Aaron DeVries, Medical Director, Infectious Disease Epidemiology, Prevention, and Control Division, Minnesota Department of Health (MDH) Sara Dunlap, Research Analysis Specialist, Site Assessment and Consultation Unit, MDH Amy Evans, Public Health Emergency Preparedness Coordinator, Olmsted County Public Health Services Susan Galatowitsch, Professor, Department of Horticultural Science, University of Minnesota Todd Krause, Warning Coordination Meteorologist, National Weather Service, Chanhassen, MN Wendy Kvale, Public Health Nurse Consultant, Office of -

Weather Products
Forecast Products The Zone Forecast Product highlights the expected sky condition, type and probability of precipitation, visibility restrictions, and temperature Zone affecting individual counties for each 12-hour period out through 7 days. Forecast ZFP Wind direction and speed are also included in the forecast out to 60 hours. WFO Paducah issues the zone forecast by 4 a.m. and 3:30 p.m. under the Product header ZFPPAH. This forecast is updated as needed to meet changing weather conditions. Refer to Appendix A for a guide to ZFP terminology. WFO Paducah provides detailed digital forecast data via the Area/Point Forecast Matrices. These products display forecast weather parameters in 3, 6, and 12-hour intervals through 7 days. Incorporated into a matrix format, this product creates a highly detailed forecast, allowing for an at-a- Area/Point AFM glance view of a large number of forecast elements. The AFM contains Forecast forecasts for each county within the WFO Paducah forecast area, while PFM the PFM shows forecasts for specific cities. WFO Paducah issues the Matrices Area/Point Forecast Matrices by 4 a.m. and 3:30 p.m. under the respective headers of AFMPAH and PFMPAH. These products are updated every 3 hours and as needed to meet changing weather conditions. Refer to Appendix B for a detailed guide to interpreting the AFM and PFM. WFO Paducah issues the Area Forecast Discussion twice daily by 4 a.m. and 3:30 p.m. under the header AFDPAH. This product provides scientific Area insight into the thought process of the forecast team at Paducah. -

July 24, 2018 It’S Hot
A rough week ahead: heat rising, air quality falling and plenty of mosquitoes By Patty Guerra Modesto Bee, Tuesday, July 24, 2018 It’s hot. And it’s going to stay hot. After a short weekend break, temperatures in the Modesto area are heading up to the triple digits again this week, prompting the National Weather Service to issue a heat advisory. The heat, combined with the Ferguson fire burning near Yosemite National Park, is also dragging down air quality. And mosquitoes are on the rise, authorities say. The advisory means that “a prolonged period of hot temperatures is expected and will create a situation in which heat illnesses are possible,” the service said in its forecast for Modesto. The advisory is in effect Tuesday through Thursday, when the temperature is expected to reach 100 or 101 degrees. Lows are expected to drop only to about 70. Officials warn residents to drink plenty of fluids, stay out of the sun and check on at-risk relatives and neighbors. “Anyone overcome by heat should be moved to a cool and shaded location,” the service said. And in a heat stroke emergency, call 911. The heat also is affecting air quality. The San Joaquin Valley Air Pollution Control District issued an Air Quality Alert on July 17 due to smoke impacts from the Ferguson fire. The alert encompasses the foothills and eastern part of Stanislaus, Merced, Madera, Fresno, and Tulare counties. Increased pollution from the fire can cause health issues including respiratory infections and asthma attacks, the district said. The alert will remain in place until the fire is extinguished. -
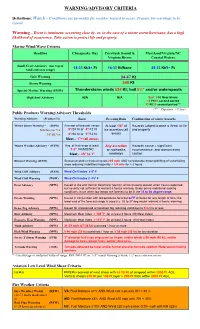
Warning/Advisory Criteria
WARNING/ADVISORY CRITERIA Definitions: Watch – Conditions are favorable for weather hazard to occur. Prepare for warnings to be issued. Warning – Event is imminent, occurring close by, or, in the case of a winter storm/hurricane, has a high likelihood of occurrence. Take action to protect life and property. Marine Wind/Wave Criteria Headline Chesapeake Bay Currituck Sound & Maryland/Virginia/NC Virginia Rivers Coastal Waters Small Craft Advisory (use top of wind and seas range) 18-33 Kt/4+ Ft 18-33 Kt/None 25-33 Kt/5+ Ft Gale Warning 34-47 Kt Storm Warning ≥48 Kt Special Marine Warning (SMW) Thunderstorm winds ≥34 Kt; hail ≥¾” and/or waterspouts High Surf Advisory N/A N/A Surf 8 Ft Near Shore 10 Ft/10 second period 12 Ft/10 second period ** (** = Duration >12 hrs) Public Products Warning/Advisory Thresholds Warning/Advisory (Product ID) Snow Freezing Rain Combination of winter hazards Winter Storm Warning * (WSW) Average of forecast. range: At least 1/4" of Hazards judged to pose a threat to life MD/Interior VA 5"/24 hr or 4"/12 hr ice accretion (all and property NC/SE VA 4"/24 hr or 3"/12 hr areas) Sleet – 1”+ (all areas) Winter Weather Advisory * (WSW) Avg. of fcst range at least: Any accretion Hazards cause A significant 1-2" VA/MD/NC on sidewalks inconvenience, and warrant extra Sleet - .25” to 1” roadways caution Blizzard Warning (WSW) Sustained wind or frequent gusts ≥35 mph AND considerable blowing/drifting of snow/falling snow reducing visibilities frequently < 1/4 mile for > 3 hours Wind Chill Advisory (WSW) Wind Chill Index ≤ 0o F Wind Chill Warning (WSW) Wind Chill Index ≤ -15o F Frost Advisory (NPW) Issued at the end (fall) or beginning (spring) of the growing season when frost is expected, but severity not sufficient to warrant a freeze warning. -

National Weather Service Warning Thresholds
NWS WARNINGS AND ADVISORIES FOR SOUTHERN NEW ENGLAND (Last Updated: December 4, 2015) The following are National Weather Service criteria for issuing Watches/Warnings/Advisories: Watches: 50% confidence of meeting Warning criteria (generally within 36-48+ hours). Advisories and Warnings: 80% confidence in the event occurrence (generally within 24-36 hours). TYPE OF ISSUANCE WHEN ISSUED FOR SOUTHERN NEW ENGLAND WINTER WEATHER ADVISORY More than one predominant hazard • Winter weather event having more than one predominant hazard (ie., snow and ice, snow and sleet, or snow, ice & sleet) meeting or exceeding advisory criteria for at least one of the precipitation elements, but remaining below warning criteria. Snow, Ocean Effect Snow, and/or Sleet • 3 inches averaged over a forecast zone in 12 hours (except 4 inches in Berkshire/Litchfield Counties) Snow and Blowing Snow • Sustained or frequent gusts of 25 to 34 mph accompanied by falling and blowing snow occasionally reducing visibility to ≤ 1/4 mile for ≥ 3 hours ` Blowing Snow • Widespread or localized blowing snow reducing visibility to ≤ ¼ mile with winds < 35 mph Black Ice • A Special Weather Statement will usually be issued when sufficient moisture is expected to cause a thin layer of ice on road surfaces, typically on cloudless nights (“black ice”). At forecaster discretion a formal Winter Weather Advisory may be issued instead. FREEZING RAIN ADVISORY Any accretion of freezing rain or freezing drizzle on road surfaces WIND CHILL ADVISORY Wind chill index between -15°F and -24°F for at least 3 hours using only the sustained wind WINTER STORM WARNING More than one predominant hazard • Winter weather event having more than one predominant hazard {ie. -

4.7 Analysis of Heat Impacts As Related to National Weather Service Extreme Heat Advisory and Warning Criteria in Eastern Iowa and Northwest Illinois
4.7 ANALYSIS OF HEAT IMPACTS AS RELATED TO NATIONAL WEATHER SERVICE EXTREME HEAT ADVISORY AND WARNING CRITERIA IN EASTERN IOWA AND NORTHWEST ILLINOIS Ray A. Wolf and David Sheets NOAA/National Weather Service, Davenport, Iowa 1. INTRODUCTION relationship of hot weather as measured by maximum daily temperature to hospital admissions found an Extreme heat is a significant cause of weather‐ increase in hospital visits due to heat for the young and related illnesses and deaths in the United States. elderly in a London, United Kingdom study, though According to the Center for Disease Control and overall there was no change in admissions. A more Prevention (CDC), extreme heat causes more deaths in recent study from North Carolina (Lippman et al. 2013) the United States each year than hurricanes, lightning, compared hospital emergency department admissions tornadoes, floods, and earthquakes combined. In with daily mean temperatures and reported the rate of addition, the annual number of heat‐related deaths admissions rose rapidly with increasing temperature, nationally is rising (CDC 2013). From 1999 to 2010, a peaking in the summer. total of 7,415 people died of heat‐related issues, an Another way to evaluate the impacts of extreme average of about 618 deaths per year. A recent study heat events is through Emergency Medical Service of ten Midwestern cities by Perera et al. (2012) found (EMS) calls. Bassil et al. (2007 and 2011) studied the that not only are dangerously hot, summer days relationship between ambulance calls related to heat becoming more common in recent decades, but these illnesses and the daily maximum temperature in events are becoming more hot and humid at night and Toronto, Canada, and found a likely relationship are lasting longer.