Identification of Antimalarial and Larvicidal Compounds
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Leaves Compound Winged Or Rarely Not Winged
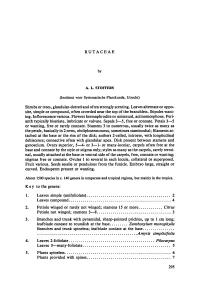
Rutaceae by A.L. Stoffers (Instituut voor Systematische Plantkunde, Utrecht) Shrubs or trees, glandular-dottedand often strongly scenting. Leaves alternate or oppo- site, simple or compound, often crowded near the top of the branchlets. Stipules want- ing. Inflorescence various. Flowers hermaphrodite or unisexual, actinomorphous. Peri- anth typically biseriate, imbricate or valvate. Sepals 3—5, free or connate. Petals 3 —5 twice or wanting, free or rarely connate. Stamens 3 to numerous, usually as many as the in 2 petals, basically rows, obdiplostemonous,sometimes staminodial; filaments at- tached at the base or the rim of the disk; anthers 2-celled, introrse, with longitudinal dehiscence; connective often with glandular apex. Disk present between stamens and gynoecium. Ovary superior, 5 —4- or 3 —1- or many-locular, carpels often free at the base and connate by the style or stigma only; styles as many as the carpels, rarely termi- nal, usually attached at the base or ventral side of the carpels, free, connate or wanting; in stigmas free or connate. Ovules 1 to several each locule, collateral or superposed. Fruit various. Seeds sessile or pendulous from the funicle. Embryo large, straight or curved. Endosperm present or wanting. About 1500 species in c. 140 genera in temperate and tropicalregions, but mainly in the tropics. Key to the genera: 1. Leaves simple (unifoliolate) 2 Leaves compound 4 Citrus 2. Petiole winged or rarely not winged; stamens 15 or more Petiole not winged; stamens 3—8 3 3. 1 Branches and trunk with pyramidal, sharp-pointed prickles, up to cm long; leafblade cuneate to roundish at the base Zanthoxylum monophylla Branches and trunk spineless; leafblade cordate at the base Amyris simplicifolia 4. -

The Taxonomy, Chorology and Reproductive Biology of Southern Afri Can Meliaceae and Ptaeroxylaceae
Bothalia 16.2: 143-168 (1986) The taxonomy, chorology and reproductive biology of southern Afri can Meliaceae and Ptaeroxylaceae F. WHITE* Keywords: chorology. Meliaceae. Ptaeroxylaceae. reproductive biology, southern Africa, taxonomy ABSTRACT Information is provided on the taxonomy, chorology and reproductive biology of 14 indigenous and two intro duced species of Meliaceae in southern Africa, and on Ptaeroxylon (Ptaeroxylaceae). Two new taxa are described: Nymanieae F. White, tribus nov. and Turraea strevi F. White & B. T. Styles, sp. nov. Nurmonia (Harms) F. White, comb, et stat. nov.. a new section of Turraea L. is created. The account complements the treatments of these families in the Flora o f southern Africa. UITTREKSEL Inligting word verskaf oor die taksonomie. chorologie en voortplantingsbiologie van 14 inheemse en twee inge- voerde spesies van Meliaceae in suidelike Afrika en oor Ptaeroxylon (Ptaeroxylaceae). Twee nuwe taksons word beskryf: Nymanieae F. White, tribus nov. en Turraea strevi F. White & B. T. Styles, sp. nov. Nurmonia (Harms) F. White, comb, et stat. nov., 'n nuwe seksie van Turraea L. word geskep. Hierdie verslag is aanvullend tot die behandelings van hierdie families in die Flora o f southern Africa. CONTENTS The position of Ptaeroxylon and Nyma nia............................................................ 163 Introduction.................................................................143 South African Trichilia: chemistry and Generic and family delimitation..................... .......144 the taxonomist's e y e .......................... 163 The position of Ptaeroxylon.................................144 Conclusions................................................... 163 The position of N ym ania.....................................144 Taxonomy as a visual a rt.............................. 163 The circumscription of Turraea..........................145 The Meliaceae and the chorology of south Notes on individual genera and species ern Africa.................................................. 164 1. -

<I>Trichilia Emetica
https://doi.org/10.30799/jnpr.062.18040201 J. Nat. Prod. Resour. - Volume 4 Issue 2 (2018) 179–181 ISSN: 2455-0299 Share Your Innovations through JACS Directory Journal of Natural Products and Resources Visit Journal at http://www.jacsdirectory.com/jnpr Isolation and Identification of Flavonoids Components from Trichilia emetica Whole Seeds Abdullahi Usman1,2,*, Vera Thoss1, Mohammad Nur-e-Alam3 1School of Chemistry, Bangor University, Bangor LL 57 2UW, United Kingdom. 2Department of Chemistry, Faculty of Natural and Applied Sciences, Nasarawa State University, P.M.B. 1022 Keffi, Nigeria. 3Department of Pharmacognosy, College of Pharmacy, King Saud University, P.O.Box 2457, Riyadh 11451, Saudi Arabia. A R T I C L E D E T A I L S A B S T R A C T Article history: Five known flavonoids were isolated from the ethyl acetate soluble fraction of aqueous extract of T. Received 24 May 2018 emetica whole seeds. On the basis of 1D and 2D-NMR experiments and MS data analyses, these Accepted 09 June 2018 compounds were identified as naringenin (B), taxifolin 4’-O-β-D-glucopyranoside (C), elephantorrhizol Available online 13 June 2018 (D), catechin 3-O-β-D-glucopyranoside (E) and eriodictyol 3-O-β-D-glucopyranoside (F). DPPH radical scavenging activity was used to estimate the antioxidant capacity of each of these compounds. The result shows that elephantorrhizol has stronger DPPH scavenging activity than other isolated flavonoids. Keywords: Trichilia emetica Naringenin Elephantorrhizol 1. Introduction plates 20 × 20 cm, E. Merck, Germany). Visualization of the compound was done using UV lamp UVL-14 EL hand held 220 V 50 Hz 4 W 254 nm white The genus Trichilia belongs to the Meliaceae (Mahogany family), it light by UVP. -
2279 Knapp-Checklisttag.Indd
A peer-reviewed open-access journal PhytoKeys 9: 15–179Checklist (2012) of vascular plants of the Department of Ñeembucú, Paraguay 15 doi: 10.3897/phytokeys.9.2279 CHECKLIST www.phytokeys.com Launched to accelerate biodiversity research Checklist of vascular plants of the Department of Ñeembucú, Paraguay Juana De Egea1,2, Maria Peña-Chocarro1, Cristina Espada1, Sandra Knapp1 1 Department of Botany, Th e Natural History Museum, Cromwell Road, London SW7 5BD, United Kingdom 2 Wildlife Conservation Society Paraguay, Capitán Benitez Vera 610, Asunción, Paraguay Corresponding author: S. Knapp ([email protected]) Academic editor: Susanne Renner | Received 25 October 2011 | Accepted 6 January 2012 | Published 30 January 2012 Citation: De Egea J, Peña-Chocarro M, Espada C, Knapp S (2012) Checklist of vascular plants of the Department of Ñeembucú, Paraguay. PhytoKeys 9: 15–179. doi: 10.3897/phytokeys.9.2279 Abstract Th e Department of Ñeembucú is one of the least well-documented areas of eastern Paraguay, and the fl ora is composed of a mixture of forest and Chaco elements. Regions like Ñeembucú are often considered of lower diversity and interest that more forested regions; this results from both actual species richness fi gures and from under-collecting due to perception as uninteresting. We present here a checklist of the vascular plants of Ñeembucú, which includes 676 taxa (including infraspecifi c taxa and collections identifi ed only to genus) in 100 families and 374 genera. Four hundred and thirty nine (439) of these are new records for Ñeembucú and of these, 4 are new published records for Paraguay. -
Addressing Target Two of the Global Strategy for Plant Conservation by Rapidly Identifying Plants at Risk
Addressing target two of the Global Strategy for Plant Conservation by rapidly identifying plants at risk James S. Miller, Holly A. Porter-Morgan, Hannah Stevens, Brian Boom, Gary A. Krupnick, Pedro Acevedo-Rodríguez, James Fleming & Micah Gensler Biodiversity and Conservation ISSN 0960-3115 Biodivers Conserv DOI 10.1007/s10531-012-0285-3 1 23 Your article is protected by copyright and all rights are held exclusively by Springer Science+Business Media B.V.. This e-offprint is for personal use only and shall not be self- archived in electronic repositories. If you wish to self-archive your work, please use the accepted author’s version for posting to your own website or your institution’s repository. You may further deposit the accepted author’s version on a funder’s repository at a funder’s request, provided it is not made publicly available until 12 months after publication. 1 23 Author's personal copy Biodivers Conserv DOI 10.1007/s10531-012-0285-3 ORIGINAL PAPER Addressing target two of the Global Strategy for Plant Conservation by rapidly identifying plants at risk James S. Miller • Holly A. Porter-Morgan • Hannah Stevens • Brian Boom • Gary A. Krupnick • Pedro Acevedo-Rodrı´guez • James Fleming • Micah Gensler Received: 1 December 2011 / Accepted: 23 March 2012 Ó Springer Science+Business Media B.V. 2012 Abstract Target two of the 2002 Global Strategy for Plant Conservation (GSPC), ‘‘A preliminary assessment of the conservation status of all known plant species, at national, regional, and international levels’’ was not accomplished by its original 2010 target date and has therefore been included as a revised 2020 target, ‘‘An assessment of the conservation status of all known plant species, as far as possible, to guide conservation action.’’ The most widely used system to estimate risk of extinction, the International Union for the Conservation of Nature Red List, provides conservation assessments for fewer than 15,000 plant species. -

A Preliminary List of the Vascular Plants and Wildlife at the Village Of
A Floristic Evaluation of the Natural Plant Communities and Grounds Occurring at The Key West Botanical Garden, Stock Island, Monroe County, Florida Steven W. Woodmansee [email protected] January 20, 2006 Submitted by The Institute for Regional Conservation 22601 S.W. 152 Avenue, Miami, Florida 33170 George D. Gann, Executive Director Submitted to CarolAnn Sharkey Key West Botanical Garden 5210 College Road Key West, Florida 33040 and Kate Marks Heritage Preservation 1012 14th Street, NW, Suite 1200 Washington DC 20005 Introduction The Key West Botanical Garden (KWBG) is located at 5210 College Road on Stock Island, Monroe County, Florida. It is a 7.5 acre conservation area, owned by the City of Key West. The KWBG requested that The Institute for Regional Conservation (IRC) conduct a floristic evaluation of its natural areas and grounds and to provide recommendations. Study Design On August 9-10, 2005 an inventory of all vascular plants was conducted at the KWBG. All areas of the KWBG were visited, including the newly acquired property to the south. Special attention was paid toward the remnant natural habitats. A preliminary plant list was established. Plant taxonomy generally follows Wunderlin (1998) and Bailey et al. (1976). Results Five distinct habitats were recorded for the KWBG. Two of which are human altered and are artificial being classified as developed upland and modified wetland. In addition, three natural habitats are found at the KWBG. They are coastal berm (here termed buttonwood hammock), rockland hammock, and tidal swamp habitats. Developed and Modified Habitats Garden and Developed Upland Areas The developed upland portions include the maintained garden areas as well as the cleared parking areas, building edges, and paths. -

Volume Ii Tomo Ii Diagnosis Biotic Environmen
Pöyry Tecnologia Ltda. Av. Alfredo Egídio de Souza Aranha, 100 Bloco B - 5° andar 04726-170 São Paulo - SP BRASIL Tel. +55 11 3472 6955 Fax +55 11 3472 6980 ENVIRONMENTAL IMPACT E-mail: [email protected] STUDY (EIA-RIMA) Date 19.10.2018 N° Reference 109000573-001-0000-E-1501 Page 1 LD Celulose S.A. Dissolving pulp mill in Indianópolis and Araguari, Minas Gerais VOLUME II – ENVIRONMENTAL DIAGNOSIS TOMO II – BIOTIC ENVIRONMENT Content Annex Distribution LD Celulose S.A. E PÖYRY - Orig. 19/10/18 –hbo 19/10/18 – bvv 19/10/18 – hfw 19/10/18 – hfw Para informação Rev. Data/Autor Data/Verificado Data/Aprovado Data/Autorizado Observações 109000573-001-0000-E-1501 2 SUMARY 8.3 Biotic Environment ................................................................................................................ 8 8.3.1 Objective .................................................................................................................... 8 8.3.2 Studied Area ............................................................................................................... 9 8.3.3 Regional Context ...................................................................................................... 10 8.3.4 Terrestrian Flora and Fauna....................................................................................... 15 8.3.5 Aquatic fauna .......................................................................................................... 167 8.3.6 Conservation Units (UC) and Priority Areas for Biodiversity Conservation (APCB) 219 8.3.7 -

Trichilia Dregeana | Plantz Africa About:Reader?Url=
Trichilia dregeana | Plantz Africa about:reader?url=http://pza.sanbi.org/trichilia-dregeana pza.sanbi.org Trichilia dregeana | Plantz Africa Introduction Trichilia dregeana is a lovely large tree that inhabits evergreen forests in high rainfall areas. It is a highly ornamental species with considerable cultural and ecological value to match. Description Description A significant feature of the forest mahogany, particularly evident in those growing in open situations, is the beautiful dark foliage and large rounded crown. Impressive heights of up to 35 m have been recorded, the tall main stem assuming a relatively straight and sometimes buttressed habit, up to 1.8 m in diameter. The grey bark is smooth in texture, but often rough and segmented around the base of the main stem on older specimens. 1 of 5 2016/12/15 01:48 PM Trichilia dregeana | Plantz Africa about:reader?url=http://pza.sanbi.org/trichilia-dregeana The compound leaves can reach lengths of 70 cm and are imparipinnate with 3-5 pairs of leaflets and a terminal one, the petiole being 8-10 cm in length. The leaflets are entire, opposite to alternate, glossy and dark green in colour, and can attain a size of 21 cm in length and 8.5 cm in width. They exhibit 8-12 pairs of side veins, petiolules around 1 cm in length, and an undersurface that is hairless to slightly hairy and notably paler than above. The creamy-white flowers, produced from October to December, are borne in dense, branched axillary inflorescences, with petals that are velvety on both surfaces and 1.4 cm-2.4 cm in length. -

Floristic Composition, Structure and Regeneration Status of Riverine Forest at Nech Sar National Park of Ethiopia
Journal of Natural Sciences Research www.iiste.org ISSN 2224-3186 (Paper) ISSN 2225-0921 (Online) Vol.7, No.7, 2017 Floristic Composition, Structure and Regeneration Status of Riverine Forest at Nech Sar National Park of Ethiopia Mulugeta Kebebew 1 Hewan Demissie 2 1.Department of Biology, Arba Minch University, Arba Minch Ethiopia 2.School of Plant and Horticulture Science, College of Agriculture, Hawassa University, Hawassa, P o Box 1417 Abstract This Study was conducted in Nech Sar National park, Gamo Gofa Zone, Southern Ethiopia for analyzing floristic composition, structure and regeneration status of woody plant species. The floristic composition and population structure of woody plant species were recorded in 76 quadrats, each of which 20 m x 20 m size. Data on species cover abundance, DBH, height and numbers of individuals per species and altitude were recorded from each quadrat. From NNP Riverine Forest 86 vascular plant species, representing 65 genera and 30 families were recorded. The family Fabaceae had the highest number of species (11) followed by Euphorbiaceae each with 7 species, Sapindaceae and Tiliaceae each by 5 species. The four most abundant woody plant species in the forest were Lecaniodiscus fraxinifolus, Trichilia dregeana, Syzygium guineense, Euclea divinorum. Moreover, the five most frequently distributed woody plant species were Lecaniodiscus fraxinifolus, Trichilia dregeana, Syzygium guineense, Euclea divinorum and Maytenus senegalensis. Three communities: Lecaniodiscus fraxinifolius-Trichilia dregeana community, Trichilia dregeana-Syzygium guineense community and Syzygium guineense -Lecaniodiscus fraxinifolius community were recognized, with similarity coefficients of 0.65, indicating that there are moderate similarity among the communities. The Shannon-Wiener diversity and evenness in the forest were 2.92 and 0.68 respectively, indicating high diversity. -

Iheringia, Série Botânica, Porto Alegre, 73(Supl.):301-307, 15 De Março De 2018
Iheringia Série Botânica Museu de Ciências Naturais ISSN ON-LINE 2446-8231 Fundação Zoobotânica do Rio Grande do Sul Check-list de Picramniales e Sapindales (exceto Sapindaceae) do estado de Mato Grosso do Sul José Rubens Pirani & Cíntia Luíza da Silva-Luz Universidade de São Paulo. Instituto de Biociências, Rua do Matão 277, Cidade Universitária, CEP 05508-090, São Paulo, SP. [email protected] Recebido em 27.IX.2014 Aceito em 06.IX.2016 DOI 10.21826/2446-8231201873s301 RESUMO – As listas de espécies de Picramniales e Sapindales (exceto Sapindaceae) ocorrentes no Mato Grosso do Sul foram compiladas com base em monografi as, fl oras e revisões taxonômicas publicadas, e dados da Lista de Espécies do Brasil e dos acervos de vários herbários. Os seguintes números de espécies foram reportados em cada família: Picramniaceae (duas spp.), Anacardiaceae (15 spp.); Burseraceae (quatro spp.), Meliaceae (15 spp.), Rutaceae (22 spp.), Simaroubaceae (cinco spp.). Cada táxon é acompanhado de citação de um voucher e dos domínios e habitats em que ocorre no Mato Grosso do Sul. Palavras-chave: Anacardiaceae, Burseraceae, Meliaceae, Rutaceae, Simaroubaceae. ABSTRACT – Checklist of Picramniales and Sapindales (excluding Sapindaceae) from the state of Mato Grosso do Sul. This compilation of species of Picramniales and Sapindales (except Sapindaceae) occurring in Mato Grosso do Sul, Brazil, is based on data from monographs, fl oras and taxonomic revisions, from the Lista de Espécies do Brasil, and from several herbaria. The following numbers of species were reported for each family: Picramniaceae (two spp.), Anacardiaceae (15 spp.), Burseraceae (four spp.), Meliaceae (15 spp.), Rutaceae (22 spp.) Simaroubaceae (fi ve spp.). -

Taxonomic Study of Species of Meliaceae Juss. State of the Espírito Santo
UNIVERSIDADE ESTADUAL DE CAMPINAS INSTITUTO DE BIOLOGIA THIAGO BEVILACQUA FLORES ESTUDO TAXONÔMICO DAS ESPÉCIES DE MELIACEAE JUSS. DO ESTADO DO ESPÍRITO SANTO TAXONOMIC STUDY OF SPECIES OF MELIACEAE JUSS. STATE OF THE ESPÍRITO SANTO. CAMPINAS 2015 AGRADECIMENTOS Ao Prof. Dr. Vinicius Castro Souza, pela orientação nesse projeto. A Fundação de Amparo à Pesquisa do Estado de São Paulo ± FAPESP ± pelo projeto regular de auxílio à pesquisa processo: 2012/00964-7. A Coordenação de Aperfeiçoamento de Pessoal de Nível Superior ± CAPES ± pela bolsa de Mestrado. A Universidade Estadual de Campinas ± UNICAMP ± pelos subsídios para desenvolvimento desse trabalho. $ (VFROD 6XSHULRU GH $JULFXOWXUD ³/XL] GH 4XHLUR]´ ± ESALQ-USP ± pela infraestrutura para o desenvolvimento desse trabalho. A todo corpo técnico da ESALQ e UNICAMP que de forma direta ou indireta contribuíram para esse trabalho. À Roseli, da Secretária de Pós-graduação em Biologia Vegetal do Instituto de Biologia da UNICAMP, por sempre me atender prontamente. Sem você não teria chegado até aqui. Aos curadores dos herbários visitados ou consultados ao longo desse trabalho. Aos colegas de laboratório e campo, Cássio, Danilo, Juliana, Maria, Mariana, Priscila, Renata, Tamaris e Vanessa, pelos momentos agradáveis que passamos juntos. A todos os colegas de pós-graduação da Unicamp, em especial à Deise Josely, *XVWDYR6KLPL]XH0DUFHOR0RQJHSHORVHQVLQDPHQWRVVREUHD³YLGD´QD8QLFDPS Ao Prof. Dr. Pedro Dias pelos conselhos e dicas na finalização desse projeto. À minha grande amiga Daniele Muniz, pelo auxílio nos momentos finais dessa empreitada. Aos meus irmãos da botânica, Gabriel Dalla Colletta, Juliana Kuntz Galvão, 5XEHQV*D\RVR&RHOKR³35$&,0$'(/(6 DENILSON ´ Aos meus familiares, por todo o amor, confiança e dedicação ao longo desses anos. -

Community Patterns and Nitrogen Dynamics of Epiphytic Lichen in Jack
Ecological and Ethnoecological Classification of a Forested Landscape in the Tayal Mrqwang Territories, Taiwan (ROC) by Kevan James Berg A Thesis presented to The University of Guelph In partial fulfilment of requirements for the degree of Doctor of Philosophy in Integrative Biology Guelph, Ontario, Canada © Kevan J. Berg, May 2013 ABSTRACT ECOLOGICAL AND ETHNOECOLOGICAL CLASSIFICATION OF A FORESTED LANDSCAPE IN THE TAYAL MRQWANG TERRITORIES, TAIWAN (ROC) Kevan James Berg Advisor: University of Guelph, 2013 Dr. Steven G. Newmaster In landscape ecology, it is widely acknowledged that landscape is as much a social and cultural entity as it is biophysical, and that people and place must be jointly considered to fully understand the evolution of spatial pattern. This thesis explores the overlapping biophysical and human dimensions of landscape in the context of an (i) ecological and (ii) ethnoecological classification on the local landscape of the Tayal Mrqwang indigenous people in north central Taiwan. The goal of the ecological classification was to identify ecosystem types for a ~3000 acre landscape by relating vegetation patterns to gradients of physiography, soil, humidity, light, pixel brightness, and human modification across 76 transect sample plots. Using multivariate analyses, seven ecosystem types were identified, ranging from xeric through submesic pine, bamboo, alder, and laurel forests to mesic evergreen broadleaved and mixed coniferous forests. At the broad scale, ecosystems were distributed along gradients of elevation, soil, humidity and human modification, while factors related to local variability in physiography and soil development were more important at the fine scale (i.e., within elevational ecoregions). Within lower elevation sites in particular, patterns of forest variation and soil development were resonant of ancestral practices, including shifting cultivation, terrace farming, arboriculture, and selective extraction.