Basic Airway Management Ventilation Without Intubation Speaker Disclosures
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tracheal Intubation Following Traumatic Injury)
CLINICAL MANAGEMENT UPDATE The Journal of TRAUMA Injury, Infection, and Critical Care Guidelines for Emergency Tracheal Intubation Immediately after Traumatic Injury C. Michael Dunham, MD, Robert D. Barraco, MD, David E. Clark, MD, Brian J. Daley, MD, Frank E. Davis III, MD, Michael A. Gibbs, MD, Thomas Knuth, MD, Peter B. Letarte, MD, Fred A. Luchette, MD, Laurel Omert, MD, Leonard J. Weireter, MD, and Charles E. Wiles III, MD for the EAST Practice Management Guidelines Work Group J Trauma. 2003;55:162–179. REFERRALS TO THE EAST WEB SITE and impaired laryngeal reflexes are nonhypercarbic hypox- Because of the large size of the guidelines, specific emia and aspiration, respectively. Airway obstruction can sections have been deleted from this article, but are available occur with cervical spine injury, severe cognitive impairment on the Eastern Association for the Surgery of Trauma (EAST) (Glasgow Coma Scale [GCS] score Յ 8), severe neck injury, Web site (www.east.org/trauma practice guidelines/Emergency severe maxillofacial injury, or smoke inhalation. Hypoventi- Tracheal Intubation Following Traumatic Injury). lation can be found with airway obstruction, cardiac arrest, severe cognitive impairment, or cervical spinal cord injury. I. STATEMENT OF THE PROBLEM Aspiration is likely to occur with cardiac arrest, severe cog- ypoxia and obstruction of the airway are linked to nitive impairment, or severe maxillofacial injury. A major preventable and potentially preventable acute trauma clinical concern with thoracic injury is the development of Hdeaths.1–4 There is substantial documentation that hyp- nonhypercarbic hypoxemia. Lung injury and nonhypercarbic oxia is common in severe brain injury and worsens neuro- hypoxemia are also potential sequelae of aspiration. -

Airway Management for COVID 19
Airway Management in Critically Ill COVID-19 Patients KATHERINE HELLER, MD ASSISTANT PROFESSOR UNIVERSITY OF WASHINGTON SCHOOL OF MEDICINE DEPARTMENT OF ANESTHESIOLOGY MEDICAL DIRECTOR: UWMC SICU Disclosures (none) Outline Staff safety PPE Patient factors/ timing Adjuncts for oxygenation Intubation procedure Preparation Equipment/technique Unusual situations Difficult airways Tracheostomy Emergencies Opening Questions Please navigate to pollev.com/katherinehel603 Priorities Priority #1: Staff Safety Considerations for Staff Procedural planning Appropriate PPE takes time Avoid emergencies when able Consider rounding (remotely?) on known COVID patients PPE Any airway management is an Aerosol Generating Procedure (AGP) Need respirator level protections airborne + contact/droplet N95 vs PAPR N95 PAPR Pro Pro Easy to don Comfortable Fast Protect face, neck, head Allow use of stethoscope Reusable More readily available Con Con Allows contamination of Require power source face and neck Need assistance to don Less comfortable and doff May not fit everyone Noisy Fit can change Infection Control Choose what work for you and your institution More important to have clear protocols and expectations Minimize in room staff Have equipment easily available Filter in line on circuit Infection control Barrier Devices Not recommended Additional encumbrance to intubation without proven benefit Not a replacement for PPE May actually increase risk [11] Failed airway Breach of PPE FDA revoked EUA for barrier devices in -

Developing an Airway Management Bundle to Standardize Emergent
It Takes A Village: Developing an Airway Management Bundle to Standardize Emergent Intubation Processes in the Emergency Department James Sacca, MD, Daniel Casey Kim, MD, Dimitri Papanagnou, MD, MPH, EdD(c) Department of Emergency Medicine, Thomas Jefferson University Hospital 1. Crash Airway Pre-medicate: Glycopyrrolate: 0.2 mg RSI TIME OUT If patient arrives without airway device present Ondansetron: 4 mg Pre-oxygenate and prepare for immediate intubation Nebulized or atomized Lidocaine: Patient Name__________________________________ If patient arrives with supraglottic device present 4 ml of 4% or 8 ml of 2% Needs Assessment Strategy #2 TJUH AIRWAY BUNDLE Problem Definition If able to oxygenate and ventilate, delay intubation Sedation: Code status permits intubation: Y or N or Unknown If patient arrives with ETT present Ketamine: 1 mg/kg bolus NPO since__________________ Confirm ETT placement (see 5.) Consider paralytic once successful Unconscious, Consider visualization with laryngoscopy Allergies______________________________ or NKDA Unreactive, D. Delayed sequence intubation 2. RSI Patient delirious/agitated so can’t pre-oxygenate We performed a FMEA to uncover latent threats through in situ Height___________________ Near death? Pre-medicate: Mallampati score_____________ Pretreatment: Glycopyrrolate: 0.2 mg Yes No For reactive airway disease: Lidocaine 1.5 mg/kg IV Ondansetron: 4 mg [ ] dentures removed Yes Airway management is at the core of emergent patient care. Emergent 1 For cardiovascular disease: Fentanyl 3 mcg/kg Sedation: simulation, as well as real patient intubations. A in situ simulation of Crash airway Difficult airway? For elevated ICP: both of the above meds/doses Ketamine: 1.5 mg/kg IBW bolus Personnel Pre-oxygenate No Induction: Paralyze intubations in the Emergency Department (ED) at Thomas Jefferson 1. -

Importance of Validation Risk Prediction Tools
Art: toc Input-citi 22:40 12/2/7 12؍balt6/z7i-anesth/z7i-anesth/z7i00812/contents panickes S ON THE COVER: David Mackey, M.D., has organized a fascinating series of commentaries by national leaders In this issue of ANESTHESIOLOGY, two original research articles and three editorial views examine in the construction and use of clinical data registries by regulatory agencies and physician the use of data in clinical decision making. practices, the first two of which appear in this month’s issue: ● Kheterpal et al.: Impact of a Novel Multiparameter Decision Support System on Intraoperative ● Mackey: Can We Finally Conquer the Problem of Medical Quality? The Systems-based Processes of Care and Postoperative Outcomes, p. 272 Opportunities of Data Registries and Medical Teamwork, p. 225 ● Liu et al.: Defining the Intrinsic Cardiac Risks of Operations to Improve Preoperative Cardiac ● Jain et al.: A Public-Private Strategy to Advance the Use of Clinical Registries, p. 227 Risk Assessments, p. 283 Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/128/2/A1/364553/20180200_0-00001.pdf by guest on 01 October 2021 ● Sessler: Decision Support Alerts: Importance of Validation, p. 241 ● Glance et al.: Risk Prediction Tools: The Need for Greater Transparency, p. 244 ● Javitt: Regulatory Landscape for Clinical Decision Support Technology, p. 247 ᭛ THIS MONTH IN ANESTHESIOLOGY 9A ᭛◆ THISEDITORIAL MONTH VIEWS IN ANESTHESIOLOGY 1A . Can We Finally Conquer the Problem of Medical Quality? The Systems-based ◼ SCIENCE, MEDICINE, AND THE ANESTHESIOLOGIST 15A Opportunities of Data Registries and Medical Teamwork 225 David C. Mackey ◼ INFOGRAPHICS IN ANESTHESIOLOGY 19A . A Public-Private Strategy to Advance the Use of Clinical Registries 227 Sachin H. -
RN to EMT-Basic Transition Course
State of Wisconsin Registered Nurse to EMT-Basic Transition Course November 2010 Wisconsin EMS Section State of Wisconsin RN to EMT-Basic Transition Course TABLE OF CONTENTS Introduction .....................................................................................................iv List of Appendices...........................................................................................vi Module 1 – Preparatory 1-1 Introduction to Emergency Care .................................................. 1-1 1-2 Well-Being of the EMT Basic ....................................................... 1-6 1-3 Medical/Legal and Ethical Issues............................................... 1-12 1-5 Lifting and Moving Patients........................................................ 1-16 1-6 Evaluation .................................................................................. 1-25 Module 2 - Patient Assessment 2-1 Scene Size-up ............................................................................. 2-1 2-2 Initial Assessment........................................................................ 2-6 2-3 Baseline Vital Signs, SAMPLE History and the Use of Pulse Oximetry .......................................................................... 2-11 2-4 Focused History and Physical Exam: Trauma ........................... 2-16 2-5 Focused History and Physical Exam: Medical ........................... 2-22 2-6 Detailed Physical Exam ............................................................. 2-27 2-7 On-Going Assessment.............................................................. -
Brevital Sodium Methohexital Sodium for Injection
BREVITAL® SODIUM METHOHEXITAL SODIUM FOR INJECTION, USP For Intravenous Use in Adults For Rectal and Intramuscular Use Only in Pediatric Patients WARNING Brevital should be used only in hospital or ambulatory care settings that provide for continuous monitoring of respiratory (e.g. pulse oximetry) and cardiac function. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation and personnel trained in their use and skilled in airway management should be assured. For deeply sedated patients, a designated individual other than the practitioner performing the procedure should be present to continuously monitor the patient. (See WARNINGS) DESCRIPTION Brevital® Sodium (Methohexital Sodium for Injection, USP) is 2,4,6 (1H, 3H, 5H)- Pyrimidinetrione, 1-methyl-5-(1-methyl-2-pentynyl)-5-(2-propenyl)-, (±)-, monosodium salt and has the empirical formula C14H17N2NaO3. Its molecular weight is 284.29. The structural formula is as follows: Methohexital sodium is a rapid, ultrashort-acting barbiturate anesthetic. Methohexital sodium for injection is a freeze-dried, sterile, nonpyrogenic mixture of methohexital sodium with 6% anhydrous sodium carbonate added as a buffer. It contains not less than 90% and not more than 110% of the labeled amount of methohexital sodium. It occurs as a white, freeze-dried plug that is freely soluble in water. This product is oxygen sensitive. The pH of the 1% solution is between 10 and 11; the pH of the 0.2% solution in 5% dextrose is between 9.5 and 10.5. Methohexital sodium may be administered by direct intravenous injection or continuous intravenous drip, intramuscular or rectal routes (see PRECAUTIONS—Pediatric Use). -

Airway Management in Anaesthesia Care
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1205 Airway management in anaesthesia care – professional and patient perspectives KATI KNUDSEN ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 ISBN 978-91-554-9534-3 UPPSALA urn:nbn:se:uu:diva-281905 2016 Dissertation presented at Uppsala University to be publicly examined in Brömssalen, Gävle sjukhus, Lasaretsleden 1, Gävle, Friday, 20 May 2016 at 13:00 for the degree of Doctor of Philosophy (Faculty of Medicine). The examination will be conducted in Swedish. Faculty examiner: Ingegerd Bergbom (Institutionen för vårdvetenskap och hälsa, Göteborgs Universitet). Abstract Knudsen, K. 2016. Airway management in anaesthesia care. – professional and patient perspectives. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1205. 56 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-554-9534-3. Background: Careful airway management, including tracheal intubation, is important when performing anaesthesia in order to achieve safe tracheal intubation. Aim: To study airway management in anaesthesia care from both the professional and patient perspectives. Methods: 11 RNAs performed three airway tests in 87 patients, monitored in a study-specific questionnaire. The tests usefulness for predicting an easy intubation was analysed (Study I). 68 of 74 anaesthesia departments in Sweden answered a self-reported questionnaire about the presence of airway guidelines (Study II). 20 anaesthesiologists were interviewed; a phenomenographic analysis was performed to describe how anaesthesiologists' understand algorithms for management of the difficult airway (Study III). 13 patients were interviewed; content analysis was performed to describe patients' experiences of being awake fiberoptic intubated (Study IV). Results: The Mallampati classification is a good screening test for predicting easy intubation and intubation can be safely performed by RNAs (Study I). -

Midazolam Injection, USP
Midazolam Injection, USP Rx only PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION WARNING ADULTS AND PEDIATRICS: Intravenous midazolam has been associated with respiratory depression and respiratory arrest, especially when used for sedation in noncritical care settings. In some cases, where this was not recognized promptly and treated effectively, death or hypoxic encephalopathy has resulted. Intravenous midazolam should be used only in hospital or ambulatory care settings, including physicians’ and dental offices, that provide for continuous monitoring of respiratory and cardiac function, i.e., pulse oximetry. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation, and personnel trained in their use and skilled in airway management should be assured (see WARNINGS). For deeply sedated pediatric patients, a dedicated individual, other than the practitioner performing the procedure, should monitor the patient throughout the procedures. The initial intravenous dose for sedation in adult patients may be as little as 1 mg, but should not exceed 2.5 mg in a normal healthy adult. Lower doses are necessary for older (over 60 years) or debilitated patients and in patients receiving concomitant narcotics or other central nervous system (CNS) depressants. The initial dose and all subsequent doses should always be titrated slowly; administer over at least 2 minutes and 1 allow an additional 2 or more minutes to fully evaluate the sedative effect. The dilution of the 5 mg/mL formulation is recommended to facilitate slower injection. Doses of sedative medications in pediatric patients must be calculated on a mg/kg basis, and initial doses and all subsequent doses should always be titrated slowly. -
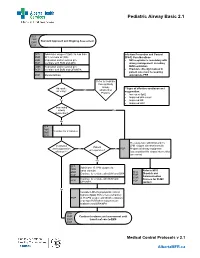
Pediatric Airway Basic 2.1
Pediatric Airway Basic 2.1 SFA FMR Standard Approach and Ongoing Assessment EMR PCP SFA Administer oxygen if SpO2 Is less than Infection Prevention and Control FMR 94% on room air (RA) (IP&C) Considerations EMR Reposition and/or suction prn • N95 respirator is mandatory with PCP Ventilate with BVM and OPA airway management, including EMR Reposition and/or suction prn BVM ventilation PCP Ventilate with BVM and OPA/NPA • Providers directly involved in patient care must be wearing PCP Monitor EtCO2 appropriate PPE Refer to Pediatric Foreign Body Airway Adequate **Signs of effective ventilation and No Obstruction air entry? oxygenation: Protocol • Increased Sp02 • Improved skin colour Yes • Improved HR • Improved LOC Impending airway Yes obstruction? No SFA FMR Ventilate for 2 minutes EMR PCP Pre-oxygenate with NRB and 15 Ventilation LPM oxygen via nasal cannula Patient and oxygenation No No PCP Prepare all airway equipment unresponsive? effective?** Assess patient for airway intervention (see notes) Yes SFA Administer 15 LPM oxygen via FMR nasal cannula Refer to MFR EMR SFA Continue to ventilate with BVM and OPA Dispatch and PCP FMR Communication EMR Continue to ventilate with BVM and Process for OLMC PCP PCP OPA/NPA contact Yes Consider LMA if symptomatic critical hypoxia (SpO2 85% or less) refractory PCP to 15 LPM oxygen with BVM ventilation (2-person BVM when resources are available) and OPA/NPA SFA FMR Continue treatment and assessment until EMR transfer of care to EMS PCP Medical Control Protocols v 2.1 AlbertaMFR.ca Pediatric Airway Basic 2.1 Definition Basic airway management is known to improve patient survival rates in the prehospital field. -

Airway Management and Ventilation: 1 W4444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444
Airway: 2 Airway Management and Ventilation: 1 W4444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444444 UNIT TERMINAL OBJECTIVE 2-1 At the completion of this unit, the EMT-Intermediate student will be able to establish and/ or maintain a patent airway, oxygenate, and ventilate a patient. COGNITIVE OBJECTIVES At the completion of this unit, the EMT-Intermediate student will be able to: 2-1.1 Explain the primary objective of airway maintenance. (C-1) 2-1.2 Identify commonly neglected prehospital skills related to airway. (C-1) 2-1.3 Identify the anatomy and functions of the upper airway. (C-1) 2-1.4 Describe the anatomy and functions of the lower airway. (C-1) 2-1.5 Explain the differences between adult and pediatric airway anatomy. (C-1) 2-1.6 Define normal tidal volumes for the adult, child, and infant. (C-1) 2-1.7 Define atelectasis. (C-1) 2-1.8 Define FiO2. (C-1) 2-1.9 Explain the relationship between pulmonary circulation and respiration. (C-3) 2-1.10 List factors which cause decreased oxygen concentrations in the blood. (C-1) 2-1.11 List the factors which increase and decrease carbon dioxide production in the body. (C 2-1.12 Describe the measurement of oxygen in the blood. (C-1) 2-1.13 Describe the measurement of carbon dioxide in the blood. (C-1) 2-1.14 List the concentration of gases which comprise atmospheric air. (C-1) 2-1.15 List the factors which affect respiratory rate and depth. (C-1) 2-1.16 Describe the voluntary and involuntary regulation of respiration. -

An Anesthesiologist's Perspective on the History of Basic Airway Management
Anesthesiology ALN SPECIAL ARTICLE ANET anet ABSTRACT aln This fourth and last installment of my history of basic airway management dis- cusses the current (i.e., “modern”) era of anesthesia and resuscitation, from 1960 to the present. These years were notable for the implementation of inter- ALN An Anesthesiologist’s mittent positive pressure ventilation inside and outside the operating room. Basic airway management in cardiopulmonary resuscitation (i.e., expired air Perspective on the ventilation) was de-emphasized, as the “A-B-C” (airway-breathing-circula- ALN tion) protocol was replaced with the “C-A-B” (circulation-airway-breathing) History of Basic Airway intervention sequence. Basic airway management in the operating room 0003-3022 (i.e., face-mask ventilation) lost its predominant position to advanced airway Management management, as balanced anesthesia replaced inhalation anesthesia. The one-hand, generic face-mask ventilation technique was inherited from the 1528-1175 The “Modern” Era, 1960 to Present progressive era. In the new context of providing intermittent positive pres- sure ventilation, the generic technique generated an underpowered grip with Lippincott Williams & WilkinsHagerstown, MD Adrian A. Matioc, M.D. a less effective seal and an unspecified airway maneuver. The significant advancement that had been made in understanding the pathophysiology of ANESTHESIOLOGY 2019; 130:00–00 upper airway obstruction was thus poorly translated into practice. In contrast 10.1097/ALN.0000000000002646 to consistent progress in advanced airway management, progress in basic airway techniques and devices stagnated. “Anesthetists who have not tried this two-handed ANESTHESIOLOGY 2019; 130:00–00 hyperextension manipulation will be surprised to observe the combined effects of simultaneously Special Article pushing the vertex of the head backward and pulling The generic one-hand face-mask ventilation inher- upward on the symphysis of the mandible.” ited from the progressive era (i.e., the “E-C” technique) 2019 Editorial. -

Emerging Uses of Capnography in Emergency Medicine in Emergency Capnography Uses of Emerging
Emerging Uses of Capnography in Emergency Medicine WHITEPAPER INTRODUCTION The Physiologic Basis for Capnography Capnography is based on a discovery by chemist Joseph Black, who, in 1875, noted the properties of a gas released during exhalation that he called “fixed air.” That gas—carbon dioxide (CO2)—is produced as a consequence of cellular metabolism as the waste product of combining oxygen and glucose to produce energy. Carbon dioxide exits the body via the lungs. The concentration of CO2 in an exhaled breath reflects cardiac output and pulmonary blood flow as the gas is transported by the venous system to the right side of the heart and then pumped into the lungs by the right ventricle. Capnographs measure the concentration of CO2 at the end of each exhaled breath, commonly known as the end- tidal carbon dioxide (EtCO2). As long as the heart is beating and blood is flowing, CO2 is delivered continuously to the lungs for exhalation. An EtCO2 value outside the normal range in a patient with normal pulmonary blood flow indicates a problem with ventilation that may require immediate attention. Any deviation from normal ventilation quickly changes EtCO2, even when SpO2—the indirect measurement of oxygen saturation in the blood—remains normal. Thus, EtCO2 is a more sensitive and rapid indicator of ventilation problems than SpO2.1 Why EtCO2 Monitoring Is Important It is generally accepted that EtCO2 monitoring is the practice standard for determining whether endotracheal tubes are correctly placed. However, there are other important indications for its use as well. Ventilatory monitoring by EtCO2 measurement has long been a standard in the surgical and intensive care patient populations.