Report of Schistosomiasis and Soil Transmitted Helminths Epidemiological Mapping and Baseline Survey in Eleven Local Government
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

Living Through Nigeria's Six-Year
“When We Can’t See the Enemy, Civilians Become the Enemy” Living Through Nigeria’s Six-Year Insurgency About the Report This report explores the experiences of civilians and armed actors living through the conflict in northeastern Nigeria. The ultimate goal is to better understand the gaps in protection from all sides, how civilians perceive security actors, and what communities expect from those who are supposed to protect them from harm. With this understanding, we analyze the structural impediments to protecting civilians, and propose practical—and locally informed—solutions to improve civilian protection and response to the harm caused by all armed actors in this conflict. About Center for Civilians in Conflict Center for Civilians in Conflict (CIVIC) works to improve protection for civil- ians caught in conflicts around the world. We call on and advise international organizations, governments, militaries, and armed non-state actors to adopt and implement policies to prevent civilian harm. When civilians are harmed we advocate the provision of amends and post-harm assistance. We bring the voices of civilians themselves to those making decisions affecting their lives. The organization was founded as Campaign for Innocent Victims in Conflict in 2003 by Marla Ruzicka, a courageous humanitarian killed by a suicide bomber in 2005 while advocating for Iraqi families. T +1 202 558 6958 E [email protected] www.civiliansinconflict.org © 2015 Center for Civilians in Conflict “When We Can’t See the Enemy, Civilians Become the Enemy” Living Through Nigeria’s Six-Year Insurgency This report was authored by Kyle Dietrich, Senior Program Manager for Africa and Peacekeeping at CIVIC. -

PSWG Actors Oct 2016
protectionsector COMPLETED AND W O R K I N G G R O U P NIGERIA: PROTECTION ACTORS ON-GOING ACTIVITIES N I G E R I A Agencies with registered projects in OCHA Online Project Systems (OPS) JAN - OCT 2016 COOPI (Cooperazione Internazionale) DRC (Danish Refugee Council) IOM (International Organization for Migration) POPULATION POPULATION POPULATION REACHED 3,168 REACHED 13,363 REACHED 92,911 IMPLEMENTING PARTNERS IMPLEMENTING PARTNERS IMPLEMENTING PARTNERS YOBE BORNO Direct Implementation YOBE BORNO Direct Implementation YOBE BORNO Direct Implementation 3,168 10,988 66,908 JERE DIKWA MAIDUGURI 28 MAIDUGURI DAMATURU DAMATURU POTISKUM KONDUGA BAMA FIKA GWOZA BENEFICIARIES PER ACTIVITY CHIBOK GOMBE GOMBE MICHIKA GOMBE MUBI 2 Case Referrals NORTH GIRERI GIRERI BENEFICIARIES PER ACTIVITY 54 Capacity Building BENEFICIARIES PER ACTIVITY Unaccompanied and ADAMAWA 947 Multiple Needs ADAMAWA ADAMAWA 2 63 Livelihood Separated Children YOLA YOLA SOUTH NORTHYOLA Unaccompanied and YOLA Protection SOUTH 24 Multiple Needs 2,221 NORTH 82 Separated Children Mainstreaming FUFORE 2,375 25,975 175 Case Referrals 176 Awareness Raising / Sensitization 293 Capacity Building 271 Material Protection Assistance Psychosocial Distress Identification of 92,417 and Mental Disorder 3 6 1,727 Vulnerable Individuals 12 LOCAL GOVERNMENT LOCAL GOVERNMENT LOCAL GOVERNMENT UNIT COVERED UNIT COVERED 10,988 Dangers and Injuries UNIT COVERED NRC IRC (International Rescue Committee) NRC (Norwegian Refugee Council) Mercy Corps POPULATION POPULATION POPULATION REACHED 165,191 REACHED -

18 Socio-Economic Characteristics of Fuelwood Cutters in Gadam, Kwami
International Journal of Humanities and Social Science Research International Journal of Humanities and Social Science Research ISSN: 2455-2070; Impact Factor: RJIF 5.22 www.socialresearchjournals.com Volume 3; Issue 1; January 2017; Page No. 18-21 Socio-economic characteristics of fuelwood cutters in gadam, kwami LGA Gombe State, Nigeria * Muhammed Bello Bashir, Yahaya Ibrahim, Adamu Sani Jauro Department of Geography Faculty of Science, Gombe State University, Gombe, Gombe State, Nigeria Abstract The paper tries to explore the Socio-economic Characteristics of Fuelwood Cutters in Gadam. The socio- economic status of fuelwood cutters were studied, the nature of fuelwood cutting as well as the possible measures that are put in place to halt the reckless felling down of tress in the name of fuelwood. Both qualitative and quantitative data were used in the study. Questionnaire and interview schedule methods are the tools used in data collection. The data were analysed using simple statistical techniques, percentage tables. The result revealed that majority of the fuelwood cutters are men within the age bracket 25-35 mostly married with Qur, anic and primary level of education. The study further discovered that trees are cut indiscriminately. Mostly fresh ones are been cut and allow to dry before taken to nearby town for sale. Finally the study suggested that such measures should be put in place to halt the indiscriminate cutting down of tress, government to provide alternative sources of energy such as affordable and reliable electric, solar and kerosene stoves, Public enlightenment campaign should be intensified among others. Keywords: fuelwood, forest, economic, income, fuelwood cutters Introduction forest have varnished or were reduced to mere shrubs (Dovie Fuel wood is any wooden material used as fuel (FAO, 2010) et al 2004) [9]. -

Nigeria National Emergency Action Plan – January 2017
NATIONAL PRIMARY HEALTH CARE DEVELOPMENT AGENCY 2017 NIGERIA POLIO ERADICATION EMERGENCY PLAN January 2017, Abuja NPHCDA Plot 681/682 Port Harcourt Crescent Off Gimbiya street, off Ahmadu Bello Way Garki Area 11 Abuja 1 Abbreviations AFP Acute Flaccid Paralysis AVADAR Auto-Visual AFP detection and Reporting. bOPV Bivalent oral polio vaccine BMGF Bill and Melinda Gates Foundation CDC Centers for Disease Control and Prevention CJTF Civilian Joint Task Force cVDPV Circulating Vaccine Derived Poliovirus DOPV Directly observed polio vaccination EOC Emergency Operations Centre ERC Expert Review Committee of Polio Eradication and Routine Immunization EPI Expanded Programme on Immunization FCT Federal Capital Territory FMOH Federal Ministry of Health FOMWAN Federation of Muslim Women Associations in Nigeria FRR Financial Resources Requirements GAVI Global Alliance of Vaccines and Immunization ICC Inter-agency Coordination Committee IDPs Internally displaced populations IPC Inter-personal Communication IPDs Immunization Plus Days IMB Independent Monitoring Board LGA Local Government Area LQAS Lot quality assurance sampling mOPV Monovalent oral polio vaccine NCC National Certification Committee NICS National Immunization Coverage Survey NIFAA Nigeria Interfaith Action Association NPEEP National Polio Eradication Emergency Plan NTL Northern Traditional Leaders Committee on Primary Health Care Delivery NPHCDA National Primary Health Care Development Agency OPV Oral polio vaccine PEI Polio Eradication Initiative PTFoPE Presidential Task Force on Polio Eradication RES Reaching Every Settlement RI Routine Immunization SIAs Supplemental Immunization Activities STF State Task Force on Immunization UNICEF United Nations Children’s Fund VCM Volunteer Community Mobilizer VDPV2 Vaccine derived polio virus type 2 WHO World Health Organization WPV Wild polio virus 2 CONTENTS Executive Summary ………………………………………………………………………………………………………… 4 1.0 Introduction and context of the programme ……………………………………………………………. -

PSWG Actors Nov 2016
protectionsector COMPLETED AND W O R K I N G G R O U P NIGERIA: PROTECTION ACTORS ON-GOING ACTIVITIES N I G E R I A Agencies with registered projects in OCHA Online Project Systems (OPS) JAN - NOV 2016 COOPI (Cooperazione Internazionale) DRC (Danish Refugee Council) IOM (International Organization for Migration) POPULATION POPULATION POPULATION REACHED 3,305 REACHED 14,505 REACHED 112,221 IMPLEMENTING PARTNERS IMPLEMENTING PARTNERS IMPLEMENTING PARTNERS YOBE BORNO Direct Implementation YOBE BORNO Direct Implementation YOBE BORNO Direct Implementation 3,305 11,088 82,312 JERE DIKWA MAIDUGURI 68 MAIDUGURI DAMATURU DAMATURU POTISKUM KONDUGA BAMA FIKA GWOZA BENEFICIARIES PER ACTIVITY CHIBOK GOMBE GOMBE MICHIKA GOMBE MUBI NORTH GIRERI 2 Case Referrals GIRERI BENEFICIARIES PER ACTIVITY BENEFICIARIES PER ACTIVITY 32 Livelihood Unaccompanied and ADAMAWA 947 Multiple Needs ADAMAWA ADAMAWA 2 Protection Separated Children 28 YOLA Mainstreaming YOLA SOUTH NORTHYOLA Unaccompanied and YOLA SOUTH Multiple Needs 2,358 NORTH 24 Separated Children 248 Capacity Building FUFORE 3,417 29,841 175 Case Referrals 381 Awareness Raising / Sensitization 333 Capacity Building Identification of 388 Vulnerable Individuals 111,687 Psychosocial Distress 1,267 Material Protection and Mental Disorder 3 6 Assistance 12 LOCAL GOVERNMENT LOCAL GOVERNMENT LOCAL GOVERNMENT UNIT COVERED UNIT COVERED 10,988 Dangers and Injuries UNIT COVERED NRC IRC (International Rescue Committee) NRC (Norwegian Refugee Council) Mercy Corps POPULATION POPULATION POPULATION REACHED 332,790 REACHED -

The State Independent Electoral Commissions in Nigeria: a Study of Bauchi, Edo, Imo, Kaduna, Lagos and Plateau States
The State Independent Electoral Commissions in Nigeria: A Study of Bauchi, Edo, Imo, Kaduna, Lagos and Plateau States Edited by Massoud Omar 0 Contributors Musa Abutudu Associate Professor, Department of Political Science. University of Benin. Edo State, Nigeria. Chijioke K. Iwuamadi Research Fellow, Institute for Development Studies University of Nigeria. Enugu State, Nigeria. Massoud Omar Department of Local Government Studies Ahmadu Bello University. Zaria, Kaduna State. F. Adeleke Faculty of Law, Lagos State University. Lagos State, Nigeria. Habu Galadima Department of Political Science, Bayero University, P.M.B. 3011, Kano-Nigeria Dung Pam Sha Department of Political Science, 1 University of Jos. Plateau State. 2 Table of Contents Introduction 4-10 Chapter I Bauchi State Independent Electoral Commission Habu Galadima and Aisha Omar 7-61 Chapter II The Edo State Independent Electoral Commission Musa Abutudu 62-97 Chapter III The Imo State Independent Electoral Commission (SIEC) Chijioke K. Iwuamadi 98- 135 Chapter IV The Kaduna State Independent Electoral Commission Massoud Omar 136-159 Chapter V Lagos State State Independent Electoral Commission in F.A.R Adeleke 156-191 Chapter VI The Plateau State Independent Electoral Commission: Dung Pam Sha 192-240 Conclusion 241-242 3 List of Tables and Figures Table 1.1 State of Residence Table 1.2 Local Government Area Table 1.3 Gender Table 1.4 Age Table 1.5 Marital Status Table 1.6 Occupation Table 1.7 Awareness of SIEC’s conduct of Local Government Elections Table 1.8 Number of times Respondents -

A Study of Violence-Related Deaths in Nafada Local Government Area Of
# Makai DANIEL http://www.ifra-nigeria.org/IMG/pdf/violence-related-deaths-gombe-jigawa-state-nigeria.pdf A Study of Violence-Related Deaths in Nafada Local Government Area of Gombe State and Auyo, Gagarawa, Gumel, Gwiwa, Kaugama and Yankwasi Local Government Areas of Jigawa State (2006-2014) IFRA-Nigeria working papers series, n°46 20/01/2015 The ‘Invisible Violence’ Project Based in the premises of the French Institute for Research in Africa on the campus of the University of Ibadan, Nigeria Watch is a database project that has monitored fatal incidents and human security in Nigeria since 1 June 2006. The database compiles violent deaths on a daily basis, including fatalities resulting from accidents. It relies on a thorough reading of the Nigerian press (15 dailies & weeklies) and reports from human rights organisations. The two main objectives are to identify dangerous areas and assess the evolution of violence in the country. However, violence is not always reported by the media, especially in remote rural areas that are difficult to access. Hence, in the last 8 years, Nigeria Watch has not recorded any report of fatal incidents in some of the 774 Local Government Areas (LGAs) of the Nigerian Federation. There are two possibilities: either these places were very peaceful, or they were not covered by the media. This series of surveys thus investigates ‘invisible’ violence. By 1 November 2014, there were still 23 LGAs with no report of fatal incidents in the Nigeria Watch database: Udung Uko and Urue-Offong/Oruko (Akwa Ibom), Kwaya Kusar (Borno), Nafada (Gombe), Auyo, Gagarawa, Kaugama and Yankwashi (Jigawa), Ingawa and Matazu (Katsina), Sakaba (Kebbi), Bassa, Igalamela- Odolu and Mopa-Muro (Kogi), Toto (Nassarawa), Ifedayo (Osun), Gudu and Gwadabaw (Sokoto), Ussa (Taraba), and Karasuwa, Machina, Nguru and Yunusari (Yobe). -

The Application of Geospatial Analytical Techniques in The
Journal of Global Initiatives: Policy, Pedagogy, Perspective Volume 10 Article 9 Number 2 Sustainable Livelihoods and Conflict March 2016 The Application of Geospatial Analytical Techniques in the Assessment of Land Use Conflicts Among Farmers and Cross-Boundary Nomadic Cattle eH rders in the Gombe Region, Nigeria Whanda J. Shittu Gombe State University, Nigeria, [email protected] Mala Galtima Gombe State University, Nigeria, [email protected] Dan Yakubu Gombe State University, Nigeria, [email protected] Follow this and additional works at: https://digitalcommons.kennesaw.edu/jgi Part of the African History Commons, African Studies Commons, Agricultural and Resource Economics Commons, Growth and Development Commons, Peace and Conflict Studies Commons, and the Political Economy Commons This work is licensed under a Creative Commons Attribution 4.0 License. Recommended Citation Shittu, Whanda J.; Galtima, Mala; and Yakubu, Dan (2016) "The Application of Geospatial Analytical Techniques in the Assessment of Land Use Conflicts Among Farmers and Cross-Boundary Nomadic Cattle eH rders in the Gombe Region, Nigeria," Journal of Global Initiatives: Policy, Pedagogy, Perspective: Vol. 10 : No. 2 , Article 9. Available at: https://digitalcommons.kennesaw.edu/jgi/vol10/iss2/9 This Article is brought to you for free and open access by DigitalCommons@Kennesaw State University. It has been accepted for inclusion in Journal of Global Initiatives: Policy, Pedagogy, Perspective by an authorized editor of DigitalCommons@Kennesaw State University. -

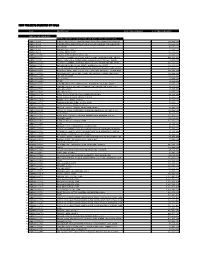
Gombe State Health Facility Listing
Gombe State Health Facility Listing LGA WARD Name of Health facility Facility Type OWNERSHIP (PUBLIC/ PRIVATE) CODE LGA State facility NO facility Ownership facility Type facility Akko Health clinic Primary Public 16 01 1 1 0001 Bula Dispensary Primary Public 16 01 1 1 0002 Bula Maternity Clinic Primary Public 16 01 1 1 0003 Akko Gamadadi Dispensary Primary Public 16 01 1 1 0004 Lawanti Dispensary Primary Public 16 01 1 1 0005 Wurodole Dispensary Primary Public 16 01 1 1 0006 Zongomari Dispensary Primary Public 16 01 1 1 0007 Arfa Medical Centre Secondary Private 16 01 2 2 0008 Bogo Maternity Clinic Primary Public 16 01 1 1 0009 Garko Dispensary Primary Public 16 01 1 1 0010 Kudulum Dispensary Primary Public 16 01 1 1 0011 Garko Gaskiya Medical Clinic Primary Private 16 01 1 2 0012 Ponon Medical Clinic Primary Private 16 01 1 2 0013 Dikko Clinic Primary Private 16 01 1 2 0014 Tabra Maternity Clinic Primary Public 16 01 1 1 0015 Tumpure Dispensary Primary Public 16 01 1 1 0016 Chilo Dispensary Primary Public 16 01 1 1 0017 Chilo Maternity Clinic Primary Public 16 01 1 1 0018 Kalshingi Gujuba Dispensary Primary Public 16 01 1 1 0019 Kalshingi Dispensary Primary Public 16 01 1 1 0020 Kalshingi (PHC) Primary Public 16 01 1 1 0021 Dongol Dispensary Primary Public 16 01 1 1 0022 Kaltanga Dispensary Primary Public 16 01 1 1 0023 Kashere Maternity Clinic Primary Public 16 01 1 1 0024 Kashere Kashere Health Centre Primary Public 16 01 1 1 0025 Kashere General Hospital Secondary Public 16 01 2 1 0026 Mispha Mat Home Primary Private 16 01 1 2 0027 Kembu Dispensary Primary Public 16 01 1 1 0028 Kidda Dispensary Primary Public 16 01 1 1 0029 Kembu Dispensary Primary Public 16 01 1 1 0030 Kumo - East Panda Maternity Clinic Primary Public 16 01 1 1 0031 Pandaya Dispensary Primary Public 16 01 1 1 0032 Tambie/Yolo Disp. -
Shelf Prospectus Within the Meaning of Rule 40 (C) of the Sec Rules and Regulations
THIS DOCUMENT IS IMPORTANT AND SHOULD BE READ CAREFULLY. IF YOU ARE IN ANY DOUBT ABOUT ITS CONTENTS OR THE ACTION TO BE TAKEN, PLEASE CONSULT YOUR BANKER, STOCKBROKER, ACCOUNTANT, SOLICITOR OR ANY OTHER PROFESSIONAL ADVISER FOR GUIDANCE IMMEDIATELY. FOR INFORMATION CONCERNING CERTAIN RISK FACTORS WHICH SHOULD BE CONSIDERED BY PROSPECTIVE INVESTORS, SEE “RISK FACTORS” COMMENCING ON PAGE 45 HEREOF. THIS DEBT ISSUANCE PROGRAMME PROSPECTUS CONSTITUTES A SHELF PROSPECTUS WITHIN THE MEANING OF RULE 40 (C) OF THE SEC RULES AND REGULATIONS GOMBE STATE GOVERNMENT OF NIGERIA BOND ISSUANCE PROGRAMME OF N30,000,000,000 This Shelf Prospectus is to be read and construed in conjunction with any supplement hereto and all documents which are incorporated herein by reference and, in relation to any Series or Tranches (as defined herein) of Bonds, together with the applicable Pricing Supplement. This Shelf Prospectus shall be read and construed on the basis that such documents are incorporated and form part of this Shelf Prospectus. This Shelf Prospectus has been seen and approved by the representatives of the State Executive Council (the “Executive Council”). The Gombe State Executive Council (“EXCO”) on behalf of the Gombe State Government have taken reasonable care to ensure that the material facts contained herein are true and accurate in all material respects and confirm having made all reasonable enquiries, that to the best of their knowledge and belief, there are no material facts, the omission of which would make any statement herein misleading or untrue. The contents of this Shelf Prospectus are not to be construed as legal, financial or tax advice. -
New Projects Inserted by Nass
NEW PROJECTS INSERTED BY NASS CODE MDA/PROJECT 2018 Proposed Budget 2018 Approved Budget FEDERAL MINISTRY OF AGRICULTURE AND RURAL SUPPLYFEDERAL AND MINISTRY INSTALLATION OF AGRICULTURE OF LIGHT AND UP COMMUNITYRURAL DEVELOPMENT (ALL-IN- ONE) HQTRS SOLAR 1 ERGP4145301 STREET LIGHTS WITH LITHIUM BATTERY 3000/5000 LUMENS WITH PIR FOR 0 100,000,000 2 ERGP4145302 PROVISIONCONSTRUCTION OF SOLAR AND INSTALLATION POWERED BOREHOLES OF SOLAR IN BORHEOLEOYO EAST HOSPITALFOR KOGI STATEROAD, 0 100,000,000 3 ERGP4145303 OYOCONSTRUCTION STATE OF 1.3KM ROAD, TOYIN SURVEYO B/SHOP, GBONGUDU, AKOBO 0 50,000,000 4 ERGP4145304 IBADAN,CONSTRUCTION OYO STATE OF BAGUDU WAZIRI ROAD (1.5KM) AND EFU MADAMI ROAD 0 50,000,000 5 ERGP4145305 CONSTRUCTION(1.7KM), NIGER STATEAND PROVISION OF BOREHOLES IN IDEATO NORTH/SOUTH 0 100,000,000 6 ERGP445000690 SUPPLYFEDERAL AND CONSTITUENCY, INSTALLATION IMO OF STATE SOLAR STREET LIGHTS IN NNEWI SOUTH LGA 0 30,000,000 7 ERGP445000691 TOPROVISION THE FOLLOWING OF SOLAR LOCATIONS: STREET LIGHTS ODIKPI IN GARKUWARI,(100M), AMAKOM SABON (100M), GARIN OKOFIAKANURI 0 400,000,000 8 ERGP21500101 SUPPLYNGURU, YOBEAND INSTALLATION STATE (UNDER OF RURAL SOLAR ACCESS STREET MOBILITY LIGHTS INPROJECT NNEWI (RAMP)SOUTH LGA 0 30,000,000 9 ERGP445000692 TOSUPPLY THE FOLLOWINGAND INSTALLATION LOCATIONS: OF SOLAR AKABO STREET (100M), LIGHTS UHUEBE IN AKOWAVILLAGE, (100M) UTUH 0 500,000,000 10 ERGP445000693 ANDEROSION ARONDIZUOGU CONTROL IN(100M), AMOSO IDEATO - NCHARA NORTH ROAD, LGA, ETITI IMO EDDA, STATE AKIPO SOUTH LGA 0 200,000,000 11 ERGP445000694