Operative Management of Neurogenic Bladder Dysfunction in Children: Ureterostomy JAMES LISTER, R
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

General Catalogue GENERAL CATALOGUE
Coloplast develops products and services that make life easier for people with very personal and private medical conditions. Working closely with the people who use our products, we create solutions that are sensitive to their special needs. We call this intimate healthcare. Our business includes ostomy care, urology and continence care, wound and skin care. & Gynaecology Urology We operate globally and employ more than 10 000 employees. General Catalogue GENERAL CATALOGUE Urology & Gynaecology The Coloplast logo and Porgès logo are registered trademarks of Coloplast A/S. © [2016- 05.] All rights reserved. Coloplast A/S, 3050 Humlebaek, Denmark. 2016 - 000NGLOBALCATEN01 INTRODUCTION Introduction With a world class innovative spirit and the ultimate objective of always being able to make your life easier, Coloplast presents its latest dedicated Urology Care catalogue including all of our disposables and implants for urology and gynaecology. For over 120 years, we have supported the medical progress through the development of the latest techniques and devices in co-operation with our leading surgeon partners. Our know-how and high quality industrial processes permit us to offer you medical materials of the very highest standards with worldwide recognition and expertise. Within this catalogue you will find all of the latest products you will need for your daily operating practice: • Endourology : A wide range of disposable products for stone management like Dormia stone extractors, Ureteral stents, Access sheath (Retrace) and guidewires. We have extended our line with a new innovative digital solution to remove ureteral stents in one step: ISIRIS α . The product is a combination between a single use flexible cystoscope with an integrated grasper and a reusable portable device • Female Pelvic Health: slings (Altis, Aris), and lightweight meshes (Restorelle), to treat stress urinary incontinence and pelvic organ prolapses. -
Radical Cystectomy and Cutaneous Ureterostomy in 4 Dogs with Trigonal Transitional Cell Carcinoma: Description of Technique and Case Series
Received: 15 July 2015 | Accepted: 18 June 2016 DOI 10.1111/vsu.12583 ORIGINAL ARTICLE Radical Cystectomy and Cutaneous Ureterostomy in 4 Dogs with Trigonal Transitional Cell Carcinoma: Description of Technique and Case Series Rafael Ricardo Huppes1 | Leandro Z. Crivellenti2,3 | Andrigo Barboza De Nardi3 | Bruno Roque Lima4 | Cristiane Alves Cintra2 | Jorge Luiz Costa Castro5 | Christopher A. Adin6 1 Department of Veterinary Clinic and Abstract Surgery, Faculdade Uninga, Maringa, Brazil Objective: To describe radical cystectomy followed by cutaneous ureterostomy as a 2 Department of Veterinary Clinic and treatment of invasive bladder neoplasia in dogs. Surgery, Franca University Study Design: Retrospective study. (UNIFRAN), Franca, Brazil Animals: Client-owned dogs with transitional cell carcinoma of the bladder trigone 3 Department of Veterinary Clinic and (n54). Surgery, S~ao Paulo State University, Jaboticabal, Brazil Methods: Perioperative complications and long-term outcomes of dogs that under- 4 went cutaneous ureterostomy following radical cystectomy and lymphadenectomy Veterinary College, Universidade Unimontes, Santos, Brazil for transitional cell carcinoma of the urinary bladder trigone were reviewed. Both ure- ters were transected and anastomosed to the ventral abdominal skin. Polyvinyl 5 Veterinary College, Pontifícia chloride catheters were placed in the ureteral stomas and maintained for 5 days. After Universidade Catolica do Parana, catheter removal, dogs were managed with an absorbent diaper over the stomas. Curitiba, Brazil Long-term outcome and survival were documented by follow-up visits or phone 6 Department of Clinical Sciences, contact. College of Veterinary Medicine, North Carolina State University, Results: Median age at the time of surgery was 10.3 years (range, 8–12). Average Raleigh, North Carolina procedural time was 4.7 hours (range, 3.8–6.1). -

How I Do It Open Distal Ureteroureterostomy for Ectopic Ureters in Infants with Duplex Systems and No Vesicoureteral Reflux Under 6 Months of Age ______
SURGICAL TECHNIQUE Vol. 47 (3): 610-614, May - June, 2021 doi: 10.1590/S1677-5538.IBJU.2020.0742 How I do it open distal ureteroureterostomy for ectopic ureters in infants with duplex systems and no vesicoureteral reflux under 6 months of age _______________________________________________ Yuding Wang 1, Luis H. Braga 1 1 Departament of Surgery, McMaster University, Hamilton, Canada ABSTRACT ARTICLE INFO We describe a step by step technique for open distal ureteroureterostomy (UU) in infants Luis H. Braga less than 6 months presenting with duplex collecting system and upper pole ectopic https://orcid.org/0000-0002-3953-7353 ureter in the absence of vesicoureteral reflux (VUR). Keywords: Vesico-Ureteral Reflux; Ureter; Infant BACKGROUND Int Braz J Urol. 2021; 47: 610-4 Approximately 70% of ectopic ureters occur with ureteral duplication, with 80% of cases including contralateral duplication. They are found mainly _____________________ in Caucasian children and are four to seven times more common in females Submitted for publication: August 20, 2020 (1). The typical patient used to present with recurrent UTIs, flank pain from obstruction, or continuous incontinence (2). However, currently, the great ma- jority of these patients are discovered incidentally on routine investigation of _____________________ prenatal hydronephrosis (2). Accepted after revision: It has been common practice to defer surgical intervention of the September 10, 2020 patients diagnosed in the neonatal period until 12 months of age. Possi- ble management options include upper pole heminephrectomy, pyelou- reterostomy, common sheath ureteral reimplantation, upper pole ureteral _____________________ Published as Ahead of Print: clipping, and ipsilateral proximal or distal ureteroureterostomy. The deci- October 20, 2020 sion towards an ablative versus a reconstructive approach has traditionally been influenced by upper pole function, as well as surgeon preference. -

The Basics of a Radical Cystectomy and Ileal Conduits Dr. Alexander Kutikov
The Basics of A Radical Cystectomy and Ileal Conduits Dr. Alexander Kutikov: But we're here to really talk about cystectomy, and let's talk a little bit about anatomy. This is what's called the retroperitoneum, which is a fancy word for the organs that live behind the bowel sack. This is kind of the anatomy that we're used to seeing, and this lives behind it. These are the kidneys. These are the ureters, the tubes that go from the kidneys to the bladder. This is the bladder, and this is the prostate in the male. We'll talk about female urological anatomy in a minute. The inner lining of the bladder is the same as the inner lining of the ureters and the same as the inner lining of the kidneys. When we talk about urothelial carcinoma, which is basically the main type of cancer that bladder cancer patients have, that is the same lining that lines the ureters and the kidneys. So patients with bladder cancer are at risk of developing tumors along their ureters and inside of the kidney. It's very important for those people that are being monitored for bladder cancer, whether they had or didn't have a cystectomy, is to have routine imaging of their upper tract. The upper tract, we basically call the kidneys and the ureters. These blue and red pipes are the great vessels. This is the aorta that brings blood away from the heart and goes down to the legs. The blue are the veins. This is the iliac veins and the vena cava. -

And Long-Term Evaluation of Renal Function After Radical Cystectomy and Cutaneous Ureterostomy in High-Risk Patients
Journal of Clinical Medicine Article Short- and Long-Term Evaluation of Renal Function after Radical Cystectomy and Cutaneous Ureterostomy in High-Risk Patients Massimiliano Creta 1,*, Ferdinando Fusco 2, Roberto La Rocca 1, Marco Capece 1 , Giuseppe Celentano 1, Ciro Imbimbo 1, Vittorio Imperatore 3, Luigi Russo 4, Francesco Mangiapia 1, Vincenzo Mirone 1, Domenico Russo 5 and Nicola Longo 1 1 Urologic Section, Department of Neurosciences, Sciences of Reproduction, and Odontostomatology, University of Naples Federico II, 80131 Naples, Italy; [email protected] (R.L.R.); [email protected] (M.C.); [email protected] (G.C.); [email protected] (C.I.); [email protected] (F.M.); [email protected] (V.M.); [email protected] (N.L.) 2 Department of Urology, Luigi Vanvitelli University of Naples, 80131 Naples, Italy; [email protected] 3 Urology Unit, Buon Consiglio Fatebenefratelli Hospital, 80123 Naples, Italy; [email protected] 4 Nephrology Unit, Ospedale del Mare; 80131 Naples, Italy; [email protected] 5 Nephrology Unit, Department of Public Health; University of Naples Federico II, 80131 Naples, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-08-1746-2611; Fax: +39-08-1545-2959 Received: 24 April 2020; Accepted: 8 July 2020; Published: 11 July 2020 Abstract: Deterioration of renal function has been reported after radical cystectomy (RC) with urinary diversion. We investigated renal function changes in elderly bladder cancer (BCa) patients who underwent RC with cutaneous ureterostomy (CU) urinary diversion. We performed a retrospective, observational study. BCa patients aged 75 with an American Society of Anesthesiologists (ASA) ≥ class greater than II were included. -

Temporary Cutaneous Ureterostomy in the Management of Advanced Congenital Urinary Obstruction* by J
Arch Dis Child: first published as 10.1136/adc.38.198.161 on 1 April 1963. Downloaded from Arch. Dis. Childh., 1963, 38, 161. TEMPORARY CUTANEOUS URETEROSTOMY IN THE MANAGEMENT OF ADVANCED CONGENITAL URINARY OBSTRUCTION* BY J. H. JOHNSTON From Alder Hey Children's Hospital, Liverpool The most extreme effects of chronic urinary I have had experience in 10 patients with severely obstruction are seen in the child who has suffered damaged urinary tracts from a variety of causes, a severe lower tract obstruction during foetal is that of temporary cutaneous ureterostomy with existence. In such cases the renal tract is dilated, later restoration of the normal urinary route after sometimes dysplastic and often decompensated, so the obstruction has been removed. Six of the that urinary stasis commonly persists after the patients were infant boys with urethral valves; removal of the original obstruction. One has to four of them had bilateral ureterostomy and two deal with a urinary system which has in many unilateral since these each had only one functioning instances never been normal and which, in most, is kidney. One of these children died of staphylo- quite incapable of approaching normality. Some coccal pneumonia; his renal function was extremely cases have insufficient renal tissue to maintain life, poor, the para-aminohippuric acid (PAH) clearance but many, if given the chance, have the capacity being only 2-5 %O of normal. An infant girl with for considerable improvement in the function both bilateral ectopic ureteroceles obstructing all four of the urinary tract musculature and of the renal duplicated ureters and with only one double kidney copyright. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Management of Prenatally Diagnosed Uropathies
Arch Dis Child: first published as 10.1136/adc.64.1_Spec_No.58 on 1 January 1989. Downloaded from Archives of Disease in Childhood, 1989, 64, 58-63 Personal practice Management of prenatally diagnosed uropathies D F M THOMAS AND A C GORDON St James's University Hospital and The General Infirmary, Leeds It is not unrealistic to anticipate that by the turn of more realistic to regard prenatal ultrasound as a the century virtually every child in the United means of screening fetuses for uropathies that will Kingdom with an appreciable urological abnormal- require investigation in postnatal life. ity will have been diagnosed by ultrasound before A recent analysis of about 47 000 pregnancies birth. There is a possibility, however, that our over a five year period in Leeds yielded an incidence ability as clinicians to interpret and utilise informa- of prenatally diagnosed uropathies of 1/570 pregnan- tion derived from prenatal ultrasound will not keep cies. This figure includes those pregnancies that pace with the increasing sophistication and availabil- were terminated and those that subsequently re- ity of the imaging techniques. Current management sulted in neonatal death from pulmonary hypopla- of prenatally diagnosed uropathies is based as much sia. If these non-viable fetuses are excluded from the on empiricism as on science. Therapeutic strategies calculation, we arrive at a figure of one live born and indications for surgery based on experience with neonate with a significant urological abnormality in by copyright. symptomatic conditions in older children are not every 800 live births. Thus the 'pick-up' rate for necessarily relevant to neonates with asymptomatic prenatal diagnosis is now within the incidence range anomalies diagnosed prenatally. -

Urology Privilege
SAN GORGONIO MEMORIAL HOSPITAL PRIVILEGE DELINEATION LIST UROLOGY NAME OF APPLICANT:____________________________________ DATE:________________ YEAR OF BOARD CERTIFICATION/RECERTIFICATION___________________________ PRIVILEGES QUALIFICATIONS/CRITERIA CATEGORY CATEGORY I USUAL AND CUSTOMARY PRIVILEGES (Procedures considered included in minimal formal training.) QUALIFICATIONS: 1. Successful completion of an accredited Urology residency training program, AND, 2. Board qualified/certified by the American Board of Urology with specific training and recent experience in privileges requested, OR, (in lieu of Board Certification) 3. Demonstrate comparable competency to perform the privileges requested based on proctoring reports, reference letters, activity/operative reports or other documentation acceptable to the Surgical Service, AND have been practicing in Urology for the past 5 years. 4. Privileges will be proctored per Surgical Service Rules and Regulations. MODERATE SEDATION I.V. MEDICATIONS FOR SPECIAL PROCEDURES (All medications with potential loss of protective reflexes regardless of route of administration) QUALIFICATIONS: Physicians with Urology privileges, by virtue of their specialty training are qualified for Moderate Sedation privileges as requested below, but must continue to demonstrate current competency as outlined in the Medical Staff Rules and Regulations. R # Done D P/O G CATEGORY 1 - USUAL AND CUSTOMARY PRIVELEGES 24 mos CORE PRIVILEGES: For the initial evaluation and management of patients of all ages for admission, work-up, pre and post-operative care, and ordering and prescribing medications per DEA certificate ENDOSCOPY: 1. Urethroscopy 2. Cystoscopy 3. Ureteroscopy 4. Nephroscopy RENAL: 5. Flank exploration, nephrectomy and/or partial 6. Removal of stones 7. Reconstruction 8. Trauma repair 9. Pyelotomy, Pyelolithotomy, Pyeloplasty 10. Retroperitoneal lymph node dissection 11. Nephroureterectomy 12. -

Obstruction of the Urinary Tract 2567
Chapter 540 ◆ Obstruction of the Urinary Tract 2567 Table 540-1 Types and Causes of Urinary Tract Obstruction LOCATION CAUSE Infundibula Congenital Calculi Inflammatory (tuberculosis) Traumatic Postsurgical Neoplastic Renal pelvis Congenital (infundibulopelvic stenosis) Inflammatory (tuberculosis) Calculi Neoplasia (Wilms tumor, neuroblastoma) Ureteropelvic junction Congenital stenosis Chapter 540 Calculi Neoplasia Inflammatory Obstruction of the Postsurgical Traumatic Ureter Congenital obstructive megaureter Urinary Tract Midureteral structure Jack S. Elder Ureteral ectopia Ureterocele Retrocaval ureter Ureteral fibroepithelial polyps Most childhood obstructive lesions are congenital, although urinary Ureteral valves tract obstruction can be caused by trauma, neoplasia, calculi, inflam- Calculi matory processes, or surgical procedures. Obstructive lesions occur at Postsurgical any level from the urethral meatus to the calyceal infundibula (Table Extrinsic compression 540-1). The pathophysiologic effects of obstruction depend on its level, Neoplasia (neuroblastoma, lymphoma, and other retroperitoneal or pelvic the extent of involvement, the child’s age at onset, and whether it is tumors) acute or chronic. Inflammatory (Crohn disease, chronic granulomatous disease) ETIOLOGY Hematoma, urinoma Ureteral obstruction occurring early in fetal life results in renal dys- Lymphocele plasia, ranging from multicystic kidney, which is associated with ure- Retroperitoneal fibrosis teral or pelvic atresia (see Fig. 537-2 in Chapter 537), to various -

MANY RENAL Transplant Candidates with End-Stage
Successful Long-Term Outcome Utilizing Existing Native Cutaneous Ureterostomy for Renal Transplant Drainage Without Ipsilateral Native Nephrectomy P.N. Bretan, Jr and R.S. Purohit ANY RENAL transplant candidates with end-stage tions, or pyelonephritis after CU. All patients had negative serial M renal disease (ESRD) have bladder or ureterove- pretransplant lavage cultures of their native kidneys and ureters to sicular junction dysfunction, and without modification these rule out the possibility asymptomatic bacteruria or subclinical candidates are considered to be poor candidates for renal pyelonephritis. Thus the rationale for safely leaving the native transplantation (RT).1 Currently, many of these patients kidney(s) depended on a high degree of confidence that there were no renal or ureteral focus for ongoing infections following trans- undergo urological reconstruction or repair before their 2 plantation. Stomal size ranged from 18 to 36 French. These highly transplant such as with ureteral undiversion to a previously selected patients elected to keep CU for urinary drainage for RT. dysfunctional bladder with bladder augmentation.3 These reconstructions seem to be associated with less morbidity Procedures compared to diversion procedures alone. However, for The kidneys were placed in the upright (normal) position in either many patients undiversion or bladder augmentation is not ileac fossa. The normal position of the allografts did not need to be an option, and they require urinary diversion prior to RT. altered for successful completion of the transplant uretero-native One alternative proposed by Levitt, et al in 1979 is uretero anastomosis. After the appropriate arterial and venous urinary diversion of transplanted kidneys through a cutane- anastomoses of transplanted kidneys, transplant ureters were spat- 4 ous ureterostomy (CU). -
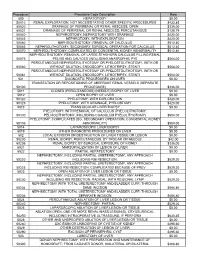
Procedure Procedure Code Description Rate 500
Procedure Procedure Code Description Rate 500 HEPATOTOMY $0.00 50010 RENAL EXPLORATION, NOT NECESSITATING OTHER SPECIFIC PROCEDURES $433.85 50020 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; OPEN $336.00 50021 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; PERCUTANIOUS $128.79 50040 NEPHROSTOMY, NEPHROTOMY WITH DRAINAGE $420.00 50045 NEPHROTOMY, WITH EXPLORATION $420.00 50060 NEPHROLITHOTOMY; REMOVAL OF CALCULUS $512.40 50065 NEPHROLITHOTOMY; SECONDARY SURGICAL OPERATION FOR CALCULUS $512.40 50070 NEPHROLITHOTOMY; COMPLICATED BY CONGENITAL KIDNEY ABNORMALITY $512.40 NEPHROLITHOTOMY; REMOVAL OF LARGE STAGHORN CALCULUS FILLING RENAL 50075 PELVIS AND CALYCES (INCLUDING ANATROPHIC PYE $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50080 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50081 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 501 DIAGNOSTIC PROCEDURES ON LIVER $0.00 TRANSECTION OR REPOSITIONING OF ABERRANT RENAL VESSELS (SEPARATE 50100 PROCEDURE) $336.00 5011 CLOSED (PERCUTANEOUS) (NEEDLE) BIOPSY OF LIVER $0.00 5012 OPEN BIOPSY OF LIVER $0.00 50120 PYELOTOMY; WITH EXPLORATION $420.00 50125 PYELOTOMY; WITH DRAINAGE, PYELOSTOMY $420.00 5013 TRANSJUGULAR LIVER BIOPSY $0.00 PYELOTOMY; WITH REMOVAL OF CALCULUS (PYELOLITHOTOMY, 50130 PELVIOLITHOTOMY, INCLUDING COAGULUM PYELOLITHOTOMY) $504.00 PYELOTOMY; COMPLICATED (EG, SECONDARY OPERATION, CONGENITAL KIDNEY 50135 ABNORMALITY) $504.00 5014 LAPAROSCOPIC LIVER BIOPSY $0.00 5019 OTHER DIAGNOSTIC PROCEDURES