Issues in CPPD Nomenclature and Classification
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Physical Properties of Acidic Calcium Phosphate Cements
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Science and Technology 1195 Physical Properties of Acidic Calcium Phosphate Cements JOHANNA UNOSSON ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6214 ISBN 978-91-554-9081-2 UPPSALA urn:nbn:se:uu:diva-233637 2014 Dissertation presented at Uppsala University to be publicly examined in Polhemsalen, Ångströmlaboratoriet, Uppsala, Friday, 5 December 2014 at 09:15 for the degree of Doctor of Philosophy. The examination will be conducted in English. Faculty examiner: Professor Uwe Gbureck (University of Wuerzburg, Germany). Abstract Unosson, J. 2014. Physical Properties of Acidic Calcium Phosphate Cements. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Science and Technology 1195. 73 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-554-9081-2. The gold standard for bone replacement today, autologous bone, suffers from several disadvantages, such as the increased risk of infection due to the need for two surgeries. Degradable synthetic materials with properties similar to bone, such as calcium phosphate cements, are a promising alternative. Calcium phosphate cements are suited for a limited amount of applications and improving their physical properties could extend their use into areas previously not considered possible. For example, cement with increased strength could be used as load bearing support in selected applications. The focus of this thesis is, therefore, on how the physical properties of acidic calcium phosphate cements (brushite cements) are affected by compositional variations, with the ultimate aim of making it possible to formulate brushite cements with desired properties. In this thesis a method to measure the porosity of a cement was developed. -

Orthophosphoric Acid and Inorganic Phosphate Compounds, Including Ortho- and Condensed Phosphates) (Various Casrns Included in the Text)
EPA/690/R-11/040F l Final 3-01-2011 Provisional Peer-Reviewed Toxicity Values for Inorganic Phosphates (Orthophosphoric Acid and Inorganic Phosphate Compounds, Including Ortho- and Condensed Phosphates) (Various CASRNs included in the text) Superfund Health Risk Technical Support Center National Center for Environmental Assessment Office of Research and Development U.S. Environmental Protection Agency Cincinnati, OH 45268 AUTHORS, CONTRIBUTORS, AND REVIEWERS CHEMICAL MANAGER Custodio V. Muianga, PhD, MPH National Center for Environmental Assessment, Cincinnati, OH DRAFT DOCUMENT PREPARED BY ICF International 9300 Lee Highway Fairfax, VA 22031 PRIMARY INTERNAL REVIEWERS Dan D. Petersen, PhD, DABT National Center for Environmental Assessment, Cincinnati, OH Anuradha Mudipalli, MSc, PhD National Center for Environmental Assessment, Research Triangle Park, NC This document was externally peer reviewed under contract to Eastern Research Group, Inc. 110 Hartwell Avenue Lexington, MA 02421-3136 Questions regarding the contents of this document may be directed to the U.S. EPA Office of Research and Development’s National Center for Environmental Assessment, Superfund Health Risk Technical Support Center (513-569-7300). TABLE OF CONTENTS COMMONLY USED ABBREVIATIONS .................................................................................... ii BACKGROUND .............................................................................................................................3 HISTORY ...................................................................................................................................3 -
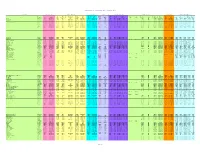
Chemical Specific Parameters May 2021
Regional Screening Level (RSL) Chemical-specific Parameters Supporting Table May 2021 Contaminant Molecular Weight Volatility Parameters Melting Point Density Diffusivity in Air and Water Partition Coefficients Water Solubility Tapwater Dermal Parameters H` HLC H` and HLC VP VP MP MP Density Density Dia Diw Dia and Diw Kd Kd Koc Koc log Kow log Kow S S B τevent t* Kp Kp Analyte CAS No. MW MW Ref (unitless) (atm-m3/mole) Ref (mmHg) Ref (C) Ref (g/cm3) Ref (cm2/s) (cm2/s) Ref (L/kg) Ref (L/kg) Ref (unitless) Ref (mg/L) Ref (unitless) (hr/event) (hr) (cm/hr) Ref Acephate 30560-19-1 1.8E+02 PHYSPROP 2.0E-11 5.0E-13 EPI 1.7E-06 PHYSPROP 8.8E+01 PHYSPROP 1.4E+00 CRC 3.7E-02 8.0E-06 WATER9 (U.S. EPA, 2001) 1.0E+01 EPI -8.5E-01 PHYSPROP 8.2E+05 PHYSPROP 2.1E-04 1.1E+00 2.7E+00 4.0E-05 EPI Acetaldehyde 75-07-0 4.4E+01 PHYSPROP 2.7E-03 6.7E-05 PHYSPROP 9.0E+02 PHYSPROP -1.2E+02 PHYSPROP 7.8E-01 CRC 1.3E-01 1.4E-05 WATER9 (U.S. EPA, 2001) 1.0E+00 EPI -3.4E-01 PHYSPROP 1.0E+06 PHYSPROP 1.3E-03 1.9E-01 4.5E-01 5.3E-04 EPI Acetochlor 34256-82-1 2.7E+02 PHYSPROP 9.1E-07 2.2E-08 PHYSPROP 2.8E-05 PHYSPROP 0.0E+00 EPI 1.1E+00 PubChem 2.2E-02 5.6E-06 WATER9 (U.S. -

A Review on Calcium Pyrophosphate and Other Related Phosphate Nano Bio-Materials and Their Applications
4R4ev. Adv. Mater. Sci. 48 (2017) 44-57 S. R. Vasant and M. J. Joshi A REVIEW ON CALCIUM PYROPHOSPHATE AND OTHER RELATED PHOSPHATE NANO BIO-MATERIALS AND THEIR APPLICATIONS Sonal R. Vasant1 and M. J. Joshi2 1Government Engineering College, Rajkot, Gujarat, India 2Department of Physics, Saurashtra University, Rajkot, Gujarat, India Received: July 29, 2016 Abstract. Over the past few decades, a little word with big potential has been rapidly insinuating into the world’s consciousness, nano. The nano-scale structures permit the control of funda- mental properties of the materials without changing their chemical structure. Living organisms can create amazing ways to produce high performance materials that involve not only creation of implants, replacing bone tissues and organs, but also synthesis of biologically active materials promoting the fullest restoration of tissues and maintenance of necessary functions of an organ- ism. In the biomaterial research field, nowadays, a great attention is given to bone substitute materials, particularly, calcium phosphate based bio-materials play important roles in clinical applications as it possesses high bio-compatibility and excellent ability to undergo varying de- grees of resorbability. These materials show a positive interaction with living tissue that includes differentiation of immature cells towards bone cells and also have chemical bonding to the bone along the interface, thought to be triggered by the adsorption of bone growth-mediating proteins at the bio-materials surface. In the present review paper an attempt is made to cover properties and applications of various phosphate nano bio-materials like calcium phosphate, calcium polyphosphate, calcium pyrophosphate etc over a time span right from 1920 to 2016. -

GRAS Notice 634: Calcium Chloride
GRAS Notice (GRN) No.634 http://www.fda.gov/Food/IngredientsPackagingLabeling/GRAS/NoticeInventory/default.htm ORIGINAL SUBMISSION Exponent 115 0 Connecticut Ave. , NW EXponenr Suite 1100 Washington, DC 20036 telephone 202-772-4900 facsimile 202-772-4979 www.exponent.com February 23 , 2016 fR1~CC~~~~[5) Paulette M. Gaynor, Ph.D. FEB 24 2016 Office of Food Additive Safety (HFS-200) Center for Food Safety and Applied Nutrition OFFICE OF Food and Drug Administration FOOI3> ADDITIVE SAFETY ~ ·--. '·-·· ·- -·. 5100 Paint Branch Parkway College Park, MD 20740-3835 GRN 00063 tf Subject: GRAS Notification for the Use of Calcium Chloride in Potato Snacks Dear Dr. Gaynor: . Pursuant to proposed 21 CFR 170.36 (62 FR 18960; April 17, 1997), PepsiCo , hereby provides notice of a claim that the food ingredient described in the enclosed notification document is exempt from the premarket approval requirement of the Federal Food, Drug, and Cosmetic Act because it has been determined to be generally recognized as safe (GRAS) , based on scientific procedures , for addition to potato snacks to reduce the formation of acrylamide. Three paper copies of the notification are provided as required; we also have provided a copy of the notification on the enclosed CD-ROM. If you have any questions or require additional information , please do not hesitate to contact me at 202-772-4915, or [email protected] . Sincerely, (b) (6) Nga Tran , DrPH, MPH Principal Scientist 0700231.003 - 8755 Exponent 1150 Connecticut Ave., NW Suite 1100 Washington, DC 20036 telephone 202-772-4900 facsimile 202-772-4979 www.exponent.com February 23, 2016 Paulette M. -

New Knowledge of Chondrocalcinosis
J Clin Pathol: first published as 10.1136/jcp.31.Suppl_12.214 on 1 January 1978. Downloaded from J. clin. Path., 31, Suppl. (Roy. Coll. Path.), 12, 214-222 New knowledge of chondrocalcinosis PAUL DIEPPE From the Department ofMedicine, University ofBristol There are three varieties of cartilage-hyaline, parathyroidism, haemachromatosis, hypothy- elastic, and fibrocartilage. Hyaline cartilage is the roidism, hypophosphataxia, hypomagnesaemia, precursor of bone. In the adult it is mainly found at gout(?), diabetes mellitus (?), Wilson's disease (?), bone ends, forming the load-bearing surface of ochronosis (?)). synovial joints. Extra-articular fibrocartilages such as those of the trachea and ribs often calcify with Historical perspective advancing age. Articular cartilage, however, usually remains free from mineral deposits. The term Intra-articular calcification has been recognisedforat 'chondrocalcinosis' may be defined as a pathological least a century. It was mentioned by Garrod (1876) state characterised by the precipitation of insoluble and by Adams (1872). With the advent of joint calcium salts in articular and periarticular cartilage. radiography there were a number of reports of The presence of chondrocalcinosis can be proved calcification of knee menisci (Pearson and Davin, only by crystallographic examination. Its presence 1921). Wolke (1935) described five cases from 2569 may be inferred by radiological examination or the knee radiographs. Zit'nan and Sifaj (1957) described discovery of crystals in synovial fluid. In addition, 12 cases, and they later identified familial cases with articular chondrocalcinosis is sometimes accom- polyarticular lesions and an associated arthritis by copyright. panied by arthritis. There are therefore three (2itnian and Silaj, 1976). separate phenomena associated with chondrocal- While 2ithan and Sifaj surveyed joint radiographs cinosis-radiological changes, crystals in synovial Hollander and McCarty (1961) examined joint fluid, and arthritis. -

ANR Rule Filing Package
Emergency Rule Coversheet Julie S. Moore, Secretary Agency of Natural Resources Revised Aug 14, 2018 page 2 Emergency Rule Coversheet 1. TITLE OF RULE FILING: Investigation and Remediation of Contaminated Properties Rule 2. ADOPTING AGENCY: Agency of Natural Resources 3. PRIMARY CONTACT PERSON: (A PERSON WHO IS ABLE TO ANSWER QUESTIONS ABOUT THE CONTENT OF THE RULE). Name: Chuck Schwer Agency: Agency of Natural Resources Mailing Address: 1 National Life Drive, Davis 1, Montpelier, Vermont 05620 Telephone: 802 249 - 5324 Fax: - E-Mail: Web URL(WHERE THE RULE WILL BE POSTED): http://dec.vermont.gov/commissioners-office/pfoa 4. SECONDARY CONTACT PERSON: (A SPECIFIC PERSON FROM WHOM COPIES OF FILINGS MAY BE REQUESTED OR WHO MAY ANSWER QUESTIONS ABOUT FORMS SUBMITTED FOR FILING IF DIFFERENT FROM THE PRIMARY CONTACT PERSON). Name: Diane Sherman Agency: Agency of Natural Resources Mailing Address: 1 National Life Drive, Davis 2, Montpelier, Vermont 05620 Telephone: 802 505 - 0125 Fax: - E-Mail: [email protected] 5. RECORDS EXEMPTION INCLUDED WITHIN RULE: (DOES THE RULE CONTAIN ANY PROVISION DESIGNATING INFORMATION AS CONFIDENTIAL; LIMITING ITS PUBLIC RELEASE; OR OTHERWISE EXEMPTING IT FROM INSPECTION AND COPYING?) No IF YES, CITE THE STATUTORY AUTHORITY FOR THE EXEMPTION: PLEASE SUMMARIZE THE REASON FOR THE EXEMPTION: 6. LEGAL AUTHORITY / ENABLING LEGISLATION: Revised Aug 14, 2018 page 3 Emergency Rule Coversheet (THE SPECIFIC STATUTORY OR LEGAL CITATION FROM SESSION LAW INDICATING WHO THE ADOPTING ENTITY IS AND THUS WHO THE SIGNATORY SHOULD BE. THIS SHOULD BE A SPECIFIC CITATION NOT A CHAPTER CITATION). 10 V.S.A. § 6603 7. EXPLANTION OF HOW THE RULE IS WITHIN THE AUTHORITY OF THE AGENCY: SECTION 6603 OF TITLE 10 OF THE VERMONT STATUTES ANNOTATED ASSIGNS THE AGENCY OF NATURAL RESOURCES WITH THE RESPONSIBILITY TO ADOPT RULES IMPLEMENTING THE PROVISIONS OF THE CHAPTER, INCLUDING THE DEFINITION OF HAZARDOUS MATERIAL IN 10 V.S.A. -

IDEM Remediation Closure Guide
INDIANA DEPARTMENT OF ENVIRONMENTAL MANAGEMENT Remediation Closure Guide March 22, 2012 With corrections through July 9, 2012 Office of Land Quality Indiana Department of Environmental Management Disclaimer This Nonrule Policy Document (NPD) is being established by the Indiana Department of Environmental Management (IDEM) consistent with its authority under IC 13-14-1-11.5. It is intended solely as guidance and shall be used in conjunction with applicable rules or laws. It does not replace applicable rules or laws, and if it conflicts with these rules or laws, the rules or laws shall control. Pursuant to IC 13-14-1-11.5, this NPD will be available for public inspection for at least forty-five (45) days prior to presentation to the appropriate State Environmental Board, and may be put into effect by IDEM thirty (30) days afterward. If the NPD is presented to more than one board, it will be effective thirty (30) days after presentation to the last State Environmental Board. IDEM also will submit the NPD to the Indiana Register for publication. INDIANA DEPARTMENT OF ENVIRONMENTAL MANAGEMENT Acknowledgements The Department of Environmental Management (IDEM) - Office of Land Quality would like to thank the following organizations and individuals who contributed either directly or indirectly to the development of the Remediation Closure Guide Nonrule Policy Document. Technical Workgroups Background Jia Guo, URS; Brian Magee, ARCADIS U.S., Inc.; Ray Milejczak, Seabreeze Technologies; Steve Schubring, AECOM Closure Tables Lisa Bradley, AECOM; Robinan Gentry, ENVIRON; Melissa Hamer-Bailey, Enviro-Assist Plume Stability John Mundell, Mundell & Associates; Joe Ricker, Premier Environmental; Ron St. -

Materials Management Plan 39Th Avenue Greenway and Park Hill Detention Denver, Colorado
January 29, 2019 Revision 3 Materials Management Plan 39th Avenue Greenway and Park Hill Detention Denver, Colorado Prepared For: City and County of Denver 200 West 14th Avenue, Department 310 Denver, Colorado 80204 Pinyon Project No.: 1/16-007-05 January 29, 2019 Revision 3 Materials Management Plan 39th Avenue Greenway and Park Hill Detention Denver, Colorado Prepared For: City and County of Denver 200 West 14th Avenue, Department 310 Denver, Colorado 80204 Pinyon Project No.: 1/16-007-05 Prepared by: ____________________ Brian R. Partington Principal Reviewed by: ____________________ Russ Cirillo, P.E. Technical Group Manager - Remediation Version History REV0 January 11, 2018 REV1 March 8, 2018 REV2 September 14, 2018 REV3 January 29, 2019 Table of Contents 1. Introduction ......................................................................................................................................................................... 1 1.1 Proposed Action ....................................................................................................................................................... 1 1.1.1 39th Avenue Greenway ....................................................................................................................................... 1 1.1.2 Park Hill Detention ............................................................................................................................................. 2 1.2 Key Parties and Responsibilities ........................................................................................................................... -

Fish Bone As a Source of Raw Material for Synthesis of Calcium Phosphate
Materials Research. 2019; 22(suppl. 1): e20190486 DOI: http://dx.doi.org/10.1590/1980-5373-MR-2019-0486 Fish Bone as a Source of Raw Material for Synthesis of Calcium Phosphate Tarcília Henrique Amaral Corrêaa , José Nilson França Holandaa,b aPrograma de Pós-Graduação em Ciência e Engenharia de Materiais - PPGECM, Universidade Estadual do Norte Fluminense - UENF, 28013-602, Campos dos Goytacazes, RJ, Brasil bLaboratório de Materiais Avançados - LAMAV, Universidade Estadual do Norte Fluminense - UENF, 28013-602, Campos dos Goytacazes, RJ, Brasil Received: August 27, 2019; Accepted: September 3, 2019 Fish bone is rich in calcium carbonate, which makes it an alternative source of low cost calcium carbonate for the synthesis of calcium phosphate bioceramic for use in bone regeneration. The calcium phosphate bioceramic was prepared by a wet precipitation method with acid and base reactions. The synthesized bioceramic was characterized in terms of X-ray diffraction (XRD), scanning electron microscopy (SEM/EDS), thermogravimetric analysis (TGA), Fourier transform infrared spectroscopy (FTIR), average crystallite size and refinement by the Rietveld method for the quantification of crystalline phases. The results indicated the formation of a biphasic calcium phosphate bioceramic comprising 67.6 % of β-calcium pyrophosphate (β-CPP) and 32.1 % of β-tricalcium phosphate (β-TCP). This biphasic calcium phosphate bioceramic synthesized using fish bone waste presented nanostructured nature with an average crystallite size of 69.58 nm, which is very promising for biomedical applications. Keywords: Calcium phosphate, biphasic bioceramic, fish bone waste, nanocrystallites. 1. Introduction In Brazil, the aquaculture sector has been showing great prominence in the last years in the growth especially in the Around the world, bone defects are caused by trauma, production of fish (fish farming). -

Safety Assessment of Ammonia and Ammonium Hydroxide As Used in Cosmetics
Safety Assessment of Ammonia and Ammonium Hydroxide as Used in Cosmetics Status: Draft Report for Panel Review Release Date: August 18, 2017 Panel Date: September 11-12, 2017 The 2017 Cosmetic Ingredient Review Expert Panel members are: Chair, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D.; Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Interim Director is Bart Heldreth, Ph.D. This report was prepared by Wilbur Johnson, Jr., M.S., Senior Scientific Analyst and Ivan Boyer, Ph.D., Toxicologist. © Cosmetic Ingredient Review 1620 L STREET, NW, SUITE 1200 ◊ WASHINGTON, DC 20036-4702 ◊ PH 202.331.0651 ◊ FAX 202.331.0088 ◊ [email protected] Commitment & Credibility since 1976 Memorandum To: CIR Expert Panel Members and Liaisons From: Wilbur Johnson, Jr. Senior Scientific Analyst Date: August 18, 2017 Subject: Draft Report on Ammonia and Ammonium Hydroxide A Scientific Literature Review (SLR) on Ammonia and Ammonium Hydroxide was issued on July 7, 2017. The attached use concentration data that are (ammoni092017data1 and ammoni092017data2) included in this report were received from the Council prior to issuance of the SLR. Also included in this package for your review are the Draft Report (ammoni092017rep), the CIR report history (ammoni092017hist), Flow chart (ammoni092017flow.docx), Literature search strategy (ammoni092017strat.docx), Ingredient data profile (ammoni092017prof), 2017 FDA VCRP data (ammoni092017FDA), the CIR final report on Phosphoric Acid and Its Salts (ammoni092017prev), and Comments that were received from the Council (ammoni092017pcpc), which have been addressed. -
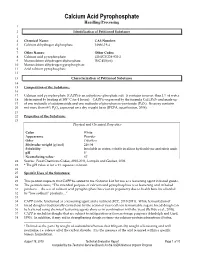
Calcium Acid Pyrophosphate
Calcium Acid Pyrophosphate Handling/Processing 1 2 Identification of Petitioned Substance 3 4 Chemical Name: CAS Number: 5 Calcium dihydrogen diphosphate 14866-19-4 6 7 Other Names: Other Codes: 8 Calcium acid pyrophosphate EINECS 238-933-2 9 Monocalcium dihydrogen diphosphate INC 450(vii) 10 Monocalcium dihydrogen pyrophosphate 11 Acid calcium pyrophosphate 12 13 Characterization of Petitioned Substance 14 15 Composition of the Substance: 16 17 Calcium acid pyrophosphate (CAPP) is an anhydrous phosphate salt. It contains no more than 1% of water 18 (determined by heating at 105° C for 4 hours). CAPP is expressed by the formula CaH2P2O7 and made up 19 of one molecule of calcium oxide and one molecule of phosphorous pentoxide (P2O5). Its assay contains 20 not more than 64% P2O5 expressed on a dry weight basis (JFCFA, specification, 2006). 21 22 Properties of the Substance: 23 Physical and Chemical Properties Color White Appearance Powder Odor Odorless Molecular weight (g/mol) 216.04 Solubility Insoluble in water; soluble in dilute hydrochloric and nitric acids pH 3* Neutralizing value1 67 24 Source: Food Chemicals Codex, 2010-2011; Lampila and Goober, 2002. 25 * The pH value is for a 1% aqueous solution. 26 27 Specific Uses of the Substance: 28 29 This petition requests that CAPP be added to the National List for use as a leavening agent in baked goods. 30 The petition states, ―The intended purpose of calcium acid pyrophosphate is as leavening acid in baked 31 products… the use of calcium acid pyrophosphate has risen in popularity due to health benefits afforded 32 by ―low sodium‖ products…‖ 33 34 CAPP can be functioned as a leavening agent and a nutrient (FCC, 2010-2011).