UHC-Pilot in Tamil Nadu: Has It Delivered What Was Expected?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
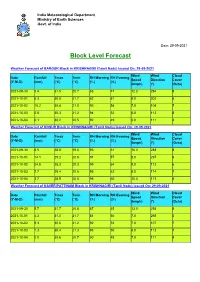
Block Level Forecast
India Meteorological Department Ministry of Earth Sciences Govt. of India Date: 29-09-2021 Block Level Forecast Weather Forecast of BARGUR Block in KRISHNAGIRI (Tamil Nadu) Issued On: 29-09-2021 Wind Wind Cloud Date Rainfall Tmax Tmin RH Morning RH Evening Speed Direction Cover (Y-M-D) (mm) (°C) (°C) (%) (%) (kmph) (°) (Octa) 2021-09-30 5.4 31.5 20.7 88 47 12.0 294 8 2021-10-01 5.3 30.8 21.7 82 51 6.0 302 5 2021-10-02 10.2 30.4 21.0 93 54 7.0 108 7 2021-10-03 0.8 30.3 21.2 94 52 6.0 113 8 2021-10-04 0.1 30.2 20.5 92 49 6.0 111 4 Weather Forecast of HOSUR Block in KRISHNAGIRI (Tamil Nadu) Issued On: 29-09-2021 Wind Wind Cloud Date Rainfall Tmax Tmin RH Morning RH Evening Speed Direction Cover (Y-M-D) (mm) (°C) (°C) (%) (%) (kmph) (°) (Octa) 2021-09-30 8.5 28.8 19.6 93 61 16.0 288 8 2021-10-01 14.1 29.2 20.6 91 57 8.0 297 6 2021-10-02 24.8 28.3 20.3 95 64 9.0 113 6 2021-10-03 2.7 28.4 20.6 95 62 8.0 114 7 2021-10-04 3.7 28.9 20.0 95 60 10.0 113 4 Weather Forecast of KAVERIPATTINAM Block in KRISHNAGIRI (Tamil Nadu) Issued On: 29-09-2021 Wind Wind Cloud Date Rainfall Tmax Tmin RH Morning RH Evening Speed Direction Cover (Y-M-D) (mm) (°C) (°C) (%) (%) (kmph) (°) (Octa) 2021-09-30 5.7 31.7 20.8 87 45 13.0 293 8 2021-10-01 4.3 31.0 21.7 81 50 7.0 298 5 2021-10-02 9.3 30.6 21.2 92 53 7.0 107 7 2021-10-03 1.3 30.4 21.3 93 50 6.0 113 7 2021-10-04 0.0 30.6 20.7 90 48 7.0 111 4 India Meteorological Department Ministry of Earth Sciences Govt. -
Annual Report 2019
ANNUAL REPORT 2019 #4/637, Krishnagiri Road, Tel: +91 4348 232451 Rayakottai – 635116, Email: [email protected] Krishnagiri District, Web: www.arcod.in Tamilnadu. 2 TABLE OF CONTENTS Facilitating Quality Learning by Linguistic Minority Children __ 3 Children of Krishnagiri _______________________________ 8 CHILDLINE - 1098 ________________________________ 10 TANSACS – Targeted Intervention ____________________ 13 LAMP – Promoting Girls Education ____________________ 14 PROMOTION OF FARMER PRODUCER COMPANY _____ 17 BOARD MEETINGS _______________________________ 18 OUR AUDITOR __________________________________________ 18 OUR BOARD MEMBERS ___________________________________ 18 OUR GRATITUDE TO DONORS _____________________________ 18 OUR INDIVIDUAL DONORS ________________________ 19 ACKNOLWEDGEMENT ____________________________________ 19 3 FACILITATING QUALITY LEARNING BY LINGUISTIC MINORITY CHILDREN ARCOD has been working since 2013 to strengthen the functions of School Management Committees (SMCs) and Anganwadis to ensure quality learning by children of linguistic minorities by orienting them on the importance of their role. The project is supported by India Literacy Project, USA. The following activities were carried out under the project during the reporting period. Refresher Training to Anganwadi Workers Refresher Training to the 1st batch of Anganwadi Workers was organized on 25th July 2018 in Nagamangalam and on 16th October 2018 in Thally for 2nd batch. During the training Ms. Alamealu, Ms. Mala, Senior Anganwadi Workers & Mr. K. Loganathan, Project Manager facilitated the sessions. The workers were oriented on the Assessment of Activity, Preparation of Low cost learning materials, Child development assessment and proper maintenance of records. 24 workers from Kelamangalam block and 26 workers from Thally Block participated in the training. School Libraries 8 school libraries were set up in the previous years. 2 more school libraries were established in the current year in GHS, Pathakotta and GHS, Devasanapalli, Shoolagiri Block. -
Krishnagiri District Diagnostic Report (DDR)
Department of Rural Development & Panchayat Raj Government of Tamil Nadu Krishnagiri District Diagnostic Report (DDR) Tamil Nadu Rural Transformation Project – TNRTP Krishnagiri District DDS – Krishnagiri, 2019 TABLE OF CONTENTS Summary 3 Objectives of the District Diagnostic Study ....................................................................... 3 Krishnagiri-An Introduction ............................................................................................... 4 Socio Demographic Profile of the District .......................................................................... 5 Sex Ratio ........................................................................................................................... 9 Literacy ............................................................................................................................. 9 SC & ST Population ........................................................................................................... 9 Occupation Profile ............................................................................................................11 Geographical Features Topography ...................................................................................13 Climate and Rainfall .........................................................................................................14 Cropping Intensity ............................................................................................................15 Soil ..................................................................................................................................16 -

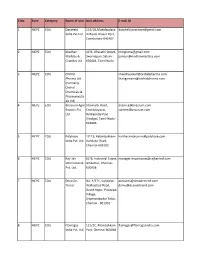
List of Food Safety Officers
LIST OF FOOD SAFETY OFFICER State S.No Name of Food Safety Area of Operation Address Contact No. Email address Officer /District ANDAMAN & 1. Smti. Sangeeta Naseem South Andaman District Food Safety Office, 09434274484 [email protected] NICOBAR District Directorate of Health Service, G. m ISLANDS B. Pant Road, Port Blair-744101 2. Smti. K. Sahaya Baby South Andaman -do- 09474213356 [email protected] District 3. Shri. A. Khalid South Andaman -do- 09474238383 [email protected] District 4. Shri. R. V. Murugaraj South Andaman -do- 09434266560 [email protected] District m 5. Shri. Tahseen Ali South Andaman -do- 09474288888 [email protected] District 6. Shri. Abdul Shahid South Andaman -do- 09434288608 [email protected] District 7. Smti. Kusum Rai South Andaman -do- 09434271940 [email protected] District 8. Smti. S. Nisha South Andaman -do- 09434269494 [email protected] District 9. Shri. S. S. Santhosh South Andaman -do- 09474272373 [email protected] District 10. Smti. N. Rekha South Andaman -do- 09434267055 [email protected] District 11. Shri. NagoorMeeran North & Middle District Food Safety Unit, 09434260017 [email protected] Andaman District Lucknow, Mayabunder-744204 12. Shri. Abdul Aziz North & Middle -do- 09434299786 [email protected] Andaman District 13. Shri. K. Kumar North & Middle -do- 09434296087 kkumarbudha68@gmail. Andaman District com 14. Smti. Sareena Nadeem Nicobar District District Food Safety Unit, Office 09434288913 [email protected] of the Deputy Commissioner , m Car Nicobar ANDHRA 1. G.Prabhakara Rao, Division-I, O/o The Gazetted Food 7659045567 [email protected] PRDESH Food Safety Officer Srikakulam District Inspector, Kalinga Road, 2. K.Kurmanayakulu, Division-II, Srikakulam District, 7659045567 [email protected] LIST OF FOOD SAFETY OFFICER State S.No Name of Food Safety Area of Operation Address Contact No. -

Annual Report 2010-11
ANNUAL REPORT 2010-11 (FOR THE PERIOD APRIL 2010 TO MARCH 2011) KRISHI VIGYAN KENDRA (KRISHNAGIRI) 1 ANNUAL REPORT APRIL 2010 – MARCH 2011 PART I - GENERAL INFORMATION ABOUT THE KVK 1.1. Name and address of KVK with phone, fax and e-mail Web Address Telephone E – mail Address Office FAX Dr. Perumal Krishi Vigyan Kendra, Elumichangiri Village, Mallinayanapalli (Post), [email protected] - 04343- 04343- Krishnagiri Taluk and District, 296039 268351 Pin – 635 120. 1.2 .Name and address of host organization with phone, fax and e-mail Web Address Telephone E - mail Address Tamil Nadu Board of Rural Office FAX Development, 24, IInd Floor, [email protected] - 044 - 044 – Crescent Park Street, T.Nagar, 24360234 24360234 Chennai – 17. 1.3. Name of the Programme Coordinator with Phone & Mobile No Telephone / Contact Name Residence Mobile E-mail Dr. T. Sundarraj - 09443888644 [email protected] 1.4. Year of sanction : 1994 2 1.5. Staff Position (as on 31st March 2011) Highest Category Sl. Name of the Qualification Pay Date of Permanent (SC/ST/ Sanctioned post Designation M/F Discipline Basic pay No. incumbent (for PC, SMS and Scale joining KVK /Temporary OBC/ Prog. Asstt.) Others) Programme Programme Plant (12,000 -420- 1 Dr.T.Sundarraj M Ph.D 14,520 06.12.2004 Permanent OBC Coordinator Coordinator Pathology 18,000) SMS (8,000-275- 2 SMS Mr.S.Sekar M Agronomy M.Sc.(Ag.) 8,275 09.10.2009 Permanent OBC (Agronomy) 13,500) SMS (8,000-275- 3 SMS Mr.T.I.Ramesh Babu M Horticulture M.Sc.(Horti.) 9,650 06.12.2004 Permanent OC (Horticulture) 13,500) SMS (Animal Animal M.V.Sc.(Poultry (8,000-275- 4 SMS Dr.K.Sakthivelkumar M 8,000 13.12.2010 Permanent OBC Science) Science Science) 13,500) SMS (Agrl. -
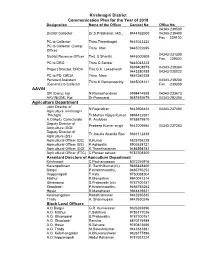
Krishnagiri District Communication Plan for the Year of 2018 AAVIN
Krishnagiri District Communication Plan for the Year of 2018 Designation Name of the Officer Contact No Office No 04343-239500 District Collector Dr.S.Prabhakar, IAS., 9444162000 04343-239400 Fax : 239100 PC to Collector Thiru.Theerthagiri 9445043224 PC to Collector (Camp Thiru. Irfan 9445022695 Office) 04343-231300 District Revenue Officer Tmt. S.Shanthi 9445000909 Fax: 239300 PC to DRO Thiru.C.Sankar 9445043223 8939408978 04343-239364 Project Director, DRDA Tmt.G.K. Lokeshwari 9443380158 04343-230022 PC to PD, DRDA Thiru. Mani 9487580158 Persoanl Assistant 04343-239200 Thiru.K.Ramamoorthy 9445008141 (General) to Collector Fax -239300 AAVIN DR (Dairy), kgi N.Ramachandiran 9994414938 04343-233673 AAVIN(GM), Kgi Dr.Pasavaraj 9487492679 04343-292204 Agriculture Department Joint Director of N.Rajendiran 9443906424 04343-237404 Agriculture, krishnagiri PA(Agri) Tr.Mohan Vijaya Kumar 9894422591 A.O(Agri), Collectorate R. Aruldoss 9788879810 Deputy Director of Pradeep Kumar singh 9443006664 04343-237363 Agriculture (GOI) Deputy Director of Tr.Jakulla Akanda Rao 9361112438 Agriculture (SS) Agricultural Officer (QC) K.Kumar 8825756228 Agricultural Officer (SS) P.Adhipathi 8903638121 Agricultural Officer (GOI) K.Theertharaman 9486598182 Agricultural Officer (FTC) C.Paneer selvam 9787508300 Assistant Directors of Agriculture Department Krishnagiri C.Pachaiyappan 8072245916 Kaveripattinam E. Senthilkumar(i/c) 9486448460 Bargur P.Krishnmoorthy, 9486755252 Veppanapalli T.Kala 9750058204 Mathur R.Mangalam 9940041314 Uthangarai S.Prabavathi (i/c) 9787700151 Shoolagiri P.Krishnmoorthy, 9486755252 Hosur R.Manoharan 9944439331 Kelamangalam RadaKrishnnan 9442395835 Thally A. Shanmugam 9442630246 Block Level Officers A.O Bargur G.R. Kumaresan 9626269396 A.O. Mathur T.Sakthivel 9786177026 A.O. Uthangarai S.Prabavathy 9787700151 A.O. Shoolagiri Renuka 8870176988 A.O. -
Krishnagiri District Communication Plan 2017 Index Disaster
Krishnagiri District Disaster Management - Communication Plan Communication Plan 2017 Index Name of the Department Page No District Collector, District Revenue Officer, 1 Project Director DRDA, P.A.(General) to Collector AAVIN 1 Agriculture Department 1 - 4 Agri - Engineering 4 Agriculture - Marketing 4 Aids Control Society 4 Animal Husbandary 4 Arasu Cable TV 4 Child Labour Erodication 4 Child Protection 4 Civil Supplies 4 Co-Operative 5 Commerical Tax 5 Differently Abled Welfare 5 District Employment Office 5 District Industries Centre (DIC) 5 Economic & Statastics 5 Educational Department 5 - 12 e-Governance 12 ELCOT 12 Election 12 Electricity Board / TANGEDCO 12 Ex-Service Men Office 13 Factories 13 Fire & Rescue Service 13 Fisheries 13 Food Safty Department 13 - 14 Forest Department 14 - 16 Geology & Mining 16 Government Pleader 16 Guest House/ TTDC Hotels 16 Health & Family Welfare 16 - 18 Highways Department 18 - 19 Name of the Department Page No Hindu Religious & Charitable 19 Endowments Horticulture Department 19 - 20 Housing Board 20 ICDS 20 Industrial Safety 20 Internal Audit 20 Labour Officer - Consulation 20 Labour Officer - Enforcement 20 Labour Officer - SSS 20 Library 20 Local Fund Audit 20 Mahalir Thittam 20 Motor Vehicle 21 Museum 21 Municipality - Hosur 21 Municipality - Krishnagiri 21 Music School 21 NABARD 21 National Highways 21 NIC 21 Noon Meal Project (NMP) 21 Police 21 - 24 Pollution Control Board 24 PRO 24 Press Reporters 24 - 25 Public Prosecutor 25 PWD Buildings 25 PWD Electrical 25 PWD(WRD) 25 Registration -

Sample Collection Centre for COVID
Sample Collection Centers # State District Centre Name Centre Address 1 TAMIL NADU Ariyalur ANDIMADAM MMU PHC ANDIMADAM 2 TAMIL NADU Ariyalur ANDIMADAM PHC ANDIMADAM 3 TAMIL NADU Ariyalur ANGANUR PHC ANGANUR 4 TAMIL NADU Ariyalur ARIYALUR URBAN MMU PHC ARIYALUR 5 TAMIL NADU Ariyalur ARIYALUR URBAN PHC ARIYALUR 6 TAMIL NADU Ariyalur ELAKURICHI PHC ELAKURICHI GOVERNMENT DISTRICT HEADQUATERS ARIYALUR 7 TAMIL NADU Ariyalur HOSPITAL 8 TAMIL NADU Ariyalur GOVT. DISTRICT HQ HOSPITAL ARIYALUR 9 TAMIL NADU Ariyalur JAYAMKONDAM GH JAYAMKONDAM GH 10 TAMIL NADU Ariyalur JAYAMKONDAM GH JAYAMKONDAM 11 TAMIL NADU Ariyalur JAYANKONDAM URBAN PHC JAYANKONDAM 12 TAMIL NADU Ariyalur KADUGUR UGPHC KADUGUR 13 TAMIL NADU Ariyalur KALLANKURICHY PHC KALLANKURICHY 14 TAMIL NADU Ariyalur KEELAPALUR PHC KEELAPALUR 15 TAMIL NADU Ariyalur KULUMUR PHC KULUMUR 16 TAMIL NADU Ariyalur KUMILIYAM ICTC UGPHC KUMILIYAM 17 TAMIL NADU Ariyalur KUMILIYAM UGPHC KUMILIYAM 18 TAMIL NADU Ariyalur KURUVADI MMU PHC GURUVADI 19 TAMIL NADU Ariyalur KURUVADI PHC KURUVADI 20 TAMIL NADU Ariyalur MANAKKAL PHC MANAKKAL 21 TAMIL NADU Ariyalur MANAKUDAIYAN PHC MANAKUDAIYAN .SENDHURAI MANAKUDIAYAN PRIMARY HEALTH CENTRE MANAKUDAIYAN 22 TAMIL NADU Ariyalur 23 TAMIL NADU Ariyalur MARUTHUR PHC MARUTHUR 24 TAMIL NADU Ariyalur MEENSURITI BLOCK PHC ICTC MEENSURITI 25 TAMIL NADU Ariyalur MEENSURITY CHC MEENSURITY JAYAKONDAM 26 TAMIL NADU Ariyalur MEENSURITY UGPHC MEENSURITY 27 TAMIL NADU Ariyalur PONPARAPPI PHC PONPARAPPI POYYATHANALLUR PRIMARY HEALTH CENTRE POYYATHANALLUR 28 TAMIL NADU Ariyalur 29 TAMIL NADU Ariyalur POYYUR PRIMARY HEALTH CENTRE POYYUR 30 TAMIL NADU Ariyalur SENDHURAI GH SENDHURAI 31 TAMIL NADU Ariyalur SUNDAKUDI PHC SUNDAKUDI 32 TAMIL NADU Ariyalur SUTHAMALLI PHC SUTHAMALLI 33 TAMIL NADU Ariyalur T PALUR CHC T PALUR 34 TAMIL NADU Ariyalur T PALUR MMU T PALUR COMMUNITY HEALTH CENTRE 35 TAMIL NADU Ariyalur T POTTAKOLLAI PRIMARY HEALTH CENTRE T POTTAKOLLAI 36 TAMIL NADU Ariyalur T. -

(Amount in Rs.) Actual Disbursement of Subsidy to Units Will Be Done by Banks After Fulfillment of Stipulated Terms & Condit
Tamilnadu Industrial Investment Corporation Limited Actual disbursement of subsidy to Units will be done by banks after fulfillment of stipulated terms & conditions Date of issue 04-07-2013 vide sanction order No. 22/CLTUC/RF-10/TNA/11-12 (Amount in Rs.) Amount of Sl.No. Unit Name & Address sanctioned subsidy 1 Mahadev Granites, S.No.222/2B, Seemanur Road, Achamangalam Village & Post, Krishnagiri Taluk & District. 667700 2 B.R. Hi-Tech CNC,83, Rajalakshmi Nagar, TVS Main Road, Near Anthivadi Check Post, Hosur - 635109. 558000 3 Srivari Industries,120, V Cross Street, Annai Sathya Nagar, 254600 4 Allfa Industries, No.37, Women's Indl. Estate, Kattur, Thirumullaivoyal, CH-62. 290800 5 Smartech Engg. & Services,DP-59, SIDCO Indl. Estate, Kakkalur, Tiruvallur - 602003. 702000 6 Kodan Products, Plot No.66, SIDCO Women Indl. Park, Kattur, Vellanur, Chennai 943000 7 Transmission Systems,Plot No.D-1/A, Industrial Estate, Ambattur, Chennai - 600 058. 616700 8 Sri Mariamman Engg. Works, 9-A, Mariamman Koil Street,Korattur, Chennai - 600 080. 482200 9 A.G.S. Irrigation, 3/11, Kalasathamman Koil St.,Selavoyal, Chennai - 600 051. 735000 10 Lokesh Industries,114-B, Mahavir Street,Sathya Nagar, Padi, Chennai. 266000 11 Mahalakshmi Granites, 9/3, Bysuhalli Village, Palacode Taluk, Dharmapuri Dt. 593000 12 Roopraj Granites,S.F.No.36/3A2, Bargur Block, Kondappanayanapalli Village, Krishnagiri Tk., Dharmapuri Dt. 381000 13 V.K.N. Auto Components,1&2, Padmavathy Nagar,Kamatchi Nagar Extention, Mangadu, Chennai - 600 122. 281000 14 Zymass Auto Systems, D-20, Industrial Estate,Ambattur, Chennai - 600058. 281600 15 Rohit Granites, S.No.81/2C, Krishnagiri - Tiruvannamalai High Road, Jagadevipalayam Village,Krishnagiri - 635203. -
List of EOU SEZ Units and Developers (1).Xlsx
S.No. Zone Category Name of unit Unit address E-mail ID 1 MEPZ EOU Datafield 119/1B,Mudalipalaya [email protected] India Pvt Ltd m Road, Arasur Post, Coimbatore-641407 2 MEPZ EOU Madhav 4/36, Bharathi Street, [email protected] Marbles & Swarnapuri, Salem- [email protected] Granites Ltd 636004, Tamil Nadu 3 MEPZ EOU Orchid [email protected] Pharma Ltd. [email protected] (Formerly Orchid Chemicals & Pharmaceutic als Ltd) 4 MEPZ EOU Bnazrum Agro Strumalai Road, [email protected] Exports Pvt Erandalaparai, [email protected] Ltd Rettiapatty Post Dindigul, Tamil Nadu - 624006 5 MEPZ EOU Polyhose 1/119, Kelambakkam- [email protected] India Pvt. Ltd. Vandalur Road, Chennai-603103 6 MEPZ EOU Raj Hair 6/76, Industrial Estate, [email protected] International Ambattur, Chennai- Pvt. Ltd. 600058 7 MEPZ EOU Deco De- No. 4/371, Vandalur- [email protected] Trend Wallajabad Road, [email protected] David Nagar, Padappai Village, Sriperumbudur Taluk, Chennai - 601301 8 MEPZ EOU Flamagas 121/2C, Mambakkam [email protected] India Pvt. Ltd. Psot, Chennai-600048 9 MEPZ EOU SVG Exports Plot No. 73, Phase II, [email protected] Pvt. Ltd. SIPCOT Indl. Complex, [email protected] Hasur-635109 10 MEPZ EOU Ramesh Plot No. A62 (A) [email protected] Flowers Pvt SIPCOT Industrial [email protected] Ltd Complex, Therku Veerapandiapuram P.O. Tuticorin-628002 11 MEPZ EOU Different Hair No. 36 and No. 37, [email protected] Pvt. Ltd. SIDCI Industrial Estate Thirumazhisai, Poonamallee, Tamil Nadu, Chennai- 602107 12 MEPZ EOU Tamilnadu 406, Madhepalli [email protected] Minerals Village, Kanimedu, [email protected] Limited. -
An Economic Analysis of Production of Cut Roses in Krishnagiri District of Uttar Pradesh, India Tamilnadu” Was Conducted in the Year 2019-2020
Journal of Pharmacognosy and Phytochemistry 2021; Sp 10(1): 01-04 E-ISSN: 2278-4136 P-ISSN: 2349-8234 www.phytojournal.com An economic analysis of production of cut roses in JPP 2021; Sp 10(1): 01-04 Received: 21-10-2020 Krishnagiri district of Tamil Nadu Accepted: 02-12-2020 Balaji KS Balaji KS and Mukesh Kumar Maurya Department of Agricultural Economics, Naini Agricultural Abstract Institute, SHUATS, Prayagraj, The present study entitled “An Economic Analysis of Production of Cut roses in Krishnagiri district of Uttar Pradesh, India Tamilnadu” was conducted in the year 2019-2020. The study made use of multi stage random sampling Mukesh Kumar Maurya technique to select 105 farmers from the selected villages of the study area. Well-structured Department of Agricultural questionnaires and interview schedule were conducted for the purpose of data collection. The production Economics, Naini Agricultural of cut roses has increased largely in the area due to increase in productivity of the crop. Resource use Institute, SHUATS, Prayagraj, structure was found varied among the three size groups. The per cost of cultivation was highest on small Uttar Pradesh, India size farms (Rs. 107241/ha) compared to medium (Rs. 105332/ha) and large farms (Rs. 103300/ha). Gross returns per hectare is highest in large farms than medium and small farms. Input output ratio is highest in large farms and lowest in small farms. The study gives clear information of extent of production of cut roses in Krishnagiri district of Tamilnadu. Keywords: Cut rose, cost and returns, input output ratio Introduction Cut Rose has become a part and parcel of life. -

Krishnagiri District Human Development Report 2017
Contents Title Page No Message by Member Secretary, State Planning Commission i Preface by the District Collector iii Acknowledgement v List of Boxes vii List of Figures viii List of Tables ix Chapters 1. District Profile 1 2. Status of Human Development 11 3. Employment, Income and Poverty 22 4. Demography, Health and Nutrition 33 5. Literacy and Education 52 6. Gender 70 7. Social Security 79 8. Infrastructure 83 9. Summary and way forward 89 Annexures Technical Notes 115 Abbreviations 124 KRISHNAGIRI DISTRICT HUMAN DEVELOPMENT REPORT 2017 District Administration, Krishnagiri and State Planning Commission, Tamil Nadu in association with MYRADA, HOSUR Contents Title Page No Message by Member Secretary, State Planning Commission i Preface by the District Collector iii Acknowledgement v List of Boxes vii List of Figures viii List of Tables ix Chapters 1. District Profile 1 2. Status of Human Development 11 3. Employment, Income and Poverty 22 4. Demography, Health and Nutrition 33 5. Literacy and Education 52 6. Gender 70 7. Social Security 79 8. Infrastructure 83 9. Summary and way forward 89 Annexures Technical Notes 115 Abbreviations 124 . ii iii iv ACKNOWLEDGEMENT The assignment of preparation of Krishnagiri District Human Development Report was formulated by State Planning Commission, Government of Tamil Nadu. The intention of the report is to take a picture on the development of various dimensions and indicators which affect the overall development of the people. To prepare the human development report for Krishnagiri district, State Planning Commission and Krishnagiri District Planning Commission assigned the task to MYRADA. For this purpose, a district level committee was constituted under the Chairmanship of District Collector and different departments which are considered necessary for preparation of the report.