De Maat, Proefschrift.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

In Ancient Egypt
THE ROLE OF THE CHANTRESS ($MW IN ANCIENT EGYPT SUZANNE LYNN ONSTINE A thesis submined in confonnity with the requirements for the degm of Ph.D. Graduate Department of Near and Middle Eastern Civiliations University of Toronto %) Copyright by Suzanne Lynn Onstine (200 1) . ~bsPdhorbasgmadr~ exclusive liceacc aiiowhg the ' Nationai hiof hada to reproduce, loan, distnia sdl copies of this thesis in miaof#m, pspa or elccmnic f-. L'atm criucrve la propri&C du droit d'autear qui protcge cette thtse. Ni la thèse Y des extraits substrrntiets deceMne&iveatetreimprimCs ouraitnmcrtrepoduitssanssoai aut&ntiom The Role of the Chmaes (fm~in Ancient Emt A doctorai dissertacion by Suzanne Lynn On*, submitted to the Department of Near and Middle Eastern Civilizations, University of Toronto, 200 1. The specitic nanire of the tiUe Wytor "cimûes", which occurrPd fcom the Middle Kingdom onwatd is imsiigated thrwgh the use of a dalabase cataloging 861 woinen whheld the title. Sorting the &ta based on a variety of delails has yielded pattern regatding their cbnological and demographical distribution. The changes in rhe social status and numbers of wbmen wbo bore the Weindicale that the Egyptians perceivecl the role and ams of the titk âiffefcntiy thugh tirne. Infomiation an the tities of ihe chantressw' family memkrs bas ailowed the author to make iderences cawming llse social status of the mmen who heu the title "chanms". MiMid Kingdom tifle-holders wverc of modest backgrounds and were quite rare. Eighteenth DMasty women were of the highest ranking families. The number of wamen who held the titk was also comparatively smaii, Nimeenth Dynasty women came [rom more modesi backgrounds and were more nwnennis. -
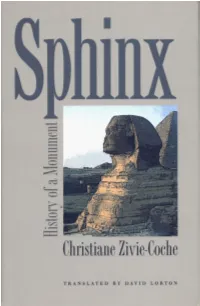
Sphinx Sphinx
SPHINX SPHINX History of a Monument CHRISTIANE ZIVIE-COCHE translated from the French by DAVID LORTON Cornell University Press Ithaca & London Original French edition, Sphinx! Le Pen la Terreur: Histoire d'une Statue, copyright © 1997 by Editions Noesis, Paris. All Rights Reserved. English translation copyright © 2002 by Cornell University All rights reserved. Except for brief quotations in a review, this book, or parts thereof, must not be reproduced in any form without permission in writing from the publisher. For information, address Cornell University Press, Sage House, 512 East State Street, Ithaca, New York 14850. First published 2002 by Cornell University Press Printed in the United States of America Library of Congress Cataloging-in-Publication Data Zivie-Coche, Christiane. Sphinx : history of a moument / Christiane Zivie-Coche ; translated from the French By David Lorton. p. cm. Includes bibliographical references and index. ISBN 0-8014-3962-0 (cloth : alk. paper) 1. Great Sphinx (Egypt)—History. I.Tide. DT62.S7 Z58 2002 932—dc2i 2002005494 Cornell University Press strives to use environmentally responsible suppliers and materials to the fullest extent possible in the publishing of its books. Such materi als include vegetable-based, low-VOC inks and acid-free papers that are recycled, totally chlorine-free, or partly composed of nonwood fibers. For further informa tion, visit our website at www.cornellpress.cornell.edu. Cloth printing 10 987654321 TO YOU PIEDRA en la piedra, el hombre, donde estuvo? —Canto general, Pablo Neruda Contents Acknowledgments ix Translator's Note xi Chronology xiii Introduction I 1. Sphinx—Sphinxes 4 The Hybrid Nature of the Sphinx The Word Sphinx 2. -

Overview of Incubation
1 Dream incubation: ancient techniques of dream influence (This document is a revised version of: T. Nielsen (1988). Ancient methods of dream incubation: Bodily methods of inducing spiritual presence. Bulletin of the Montreal Center for the Study of Dreams, 3(3- 4):6-10; please cite as T. Nielsen (2012), Dream incubation: ancient techniques of dream influence, www.dreamscience.ca) What is dream incubation? Dream incubation refers collectively to the practices, rituals, techniques and efforts that an individual applies to intentionally evoke helpful dreams. Derived from the Latin verb incubare (in- 'upon' + cubare 'to lie'), the term connotes the support and nurturance provided by a laying mother bird for her developing egg. The parallels with dream influence are all too appropriate; in antiquity, the aspirant for a dream laid down to sleep in a sacred precinct with the intention of nurturing a dream of healing or prophecy. In more modern times, the aspirant frequently sleeps in a more profane location, but the nurturing intention toward the ‘developing dream’ remains the same. The dream may be induced by engaging in several methods, techniques, rituals or other activities on the day prior to the intended dream and often just in the hours prior to falling asleep. The evoked dream is expected to address the question, situation or condition that motivated the incubation effort. To incubate a dream for a particular goal is thus to engage in an action that brings the dream content to address this goal—preferably in a direct manner. In the best case scenario, the dream will furnish a clear solution to a problem or will even depict an ailment as cured. -

Evidence for the Indo-European Origin of Two Ancient Chinese Deities
SINO-PLATONIC PAPERS Number 118 June, 2002 The Spider’s Web. Goddesses of Light and Loom: Examining the Evidence for the Indo-European Origin of Two Ancient Chinese Deities by Justine T. Snow Victor H. Mair, Editor Sino-Platonic Papers Department of East Asian Languages and Civilizations University of Pennsylvania Philadelphia, PA 19104-6305 USA [email protected] www.sino-platonic.org SINO-PLATONIC PAPERS FOUNDED 1986 Editor-in-Chief VICTOR H. MAIR Associate Editors PAULA ROBERTS MARK SWOFFORD ISSN 2157-9679 (print) 2157-9687 (online) SINO-PLATONIC PAPERS is an occasional series dedicated to making available to specialists and the interested public the results of research that, because of its unconventional or controversial nature, might otherwise go unpublished. The editor-in-chief actively encourages younger, not yet well established, scholars and independent authors to submit manuscripts for consideration. Contributions in any of the major scholarly languages of the world, including romanized modern standard Mandarin (MSM) and Japanese, are acceptable. In special circumstances, papers written in one of the Sinitic topolects (fangyan) may be considered for publication. Although the chief focus of Sino-Platonic Papers is on the intercultural relations of China with other peoples, challenging and creative studies on a wide variety of philological subjects will be entertained. This series is not the place for safe, sober, and stodgy presentations. Sino- Platonic Papers prefers lively work that, while taking reasonable risks to advance the field, capitalizes on brilliant new insights into the development of civilization. Submissions are regularly sent out to be refereed, and extensive editorial suggestions for revision may be offered. -

Dein „Göttliches“ Memory
Dein „Göttliches“ Memory Amun Bastet Amun ist der „König der Götter“ und eine der wich- Bastet ist eine Schutz- und Muttergöttin für schwan- tigsten Gottheiten Ägyptens. Er trägt meistens eine gere Frauen sowie Verstorbene. Allerdings hat sie Krone mit zwei hohen Federn, das Götter-Zepter und auch eine zweite, aggressive Seite. Darstellungen zei- ein Anch-Zeichen, das für „Leben“ steht. gen sie als Frau mit dem Kopf einer Löwin oder einer Katze sowie als Katze. Zu ihren Attributen zählen das Anubis Sistrum, eine Rassel, und ein Menit-Halsschmuck. Der Totengott Anubis führt die Toten ins Jenseits und Bes ist für die Mumifizierung zuständig. Beim Totenge- richt wiegt er das Herz des Verstorbenen gegen die Bes gehört zu den zwergengestaltigen Gottheiten. Er Feder der Maat, die für Wahrheit und Gerechtigkeit ist ein Schutzgott und wehrt Gefahren ab, insbeson- steht. Anubis wird als Mann mit Schakalskopf oder dere von Schwangeren, Gebärenden und Kindern. als Schakal dargestellt. Sein Gesicht ist fratzenhaft mit herausgestreckter Zunge, Bart und Löwenmähne. Oft trägt er einen Fe- Anukis derkopfschmuck auf seinem Kopf. Außerdem kann er Schutzsymbole wie Schlangen, Messer oder Musik- Anukis ist zusammen mit den Gottheiten Chnum und instrumente halten. Satis für die Nilflut zuständig. Sie lässt diese jährliche Überschwemmung zurückgehen. Sie trägt eine Fe- Chepri derkrone und ihr heiliges Tier ist die Gazelle. Chepri ist die im Osten aufgehende Sonne, also der Apis täglich neu geborene Sonnengott. Deshalb wurde er als fortwährende Erneuerung des Lebens verehrt. Er Der heilige Apis-Stier ist die irdische Manifestation wird als Skarabäus oder als Mann mit einem Skara- des Gottes Ptah. -

Size-Frequency Distribution of Boulders ≥7 M on Comet 67P/Churyumov
A&A 583, A37 (2015) Astronomy DOI: 10.1051/0004-6361/201525975 & c ESO 2015 Astrophysics Rosetta mission results pre-perihelion Special feature Size-frequency distribution of boulders ≥7moncomet 67P/Churyumov-Gerasimenko Maurizio Pajola1, Jean-Baptiste Vincent2, Carsten Güttler2, Jui-Chi Lee3, Ivano Bertini1, Matteo Massironi4, Emanuele Simioni5, Francesco Marzari6, Lorenza Giacomini4, Alice Lucchetti1, Cesare Barbieri1,6, Gabriele Cremonese7, Giampiero Naletto8, Antoine Pommerol9, Mohamed R. El-Maarry9, Sébastien Besse10, Michael Küppers11, Fiorangela La Forgia6, Monica Lazzarin6, Nicholas Thomas9, Anne-Thérèse Auger12, Holger Sierks2, Philippe Lamy12, Rafael Rodrigo13,14, Detlef Koschny11, Hans Rickman15,16, Horst U. Keller17, Jessica Agarwal2, Michael F. A’Hearn18, Maria A. Barucci19,20, Jean-Loup Bertaux21, Vania Da Deppo5, Björn Davidsson15, Mariolino De Cecco22, Stefano Debei23, Francesca Ferri1, Sonia Fornasier19,20, Marco Fulle24, Olivier Groussin12, Pedro J. Gutierrez25, Stubbe F. Hviid26, Wing-Huen Ip3, Laurent Jorda12, Jörg Knollenberg26, J.-Rainer Kramm2, Ekkehard Kürt26,LuisaM.Lara25, Zhong-Yi Lin3, Jose J. Lopez Moreno25, Sara Magrin6, Simone Marchi27, Harald Michalik28, Richard Moissl10, Stefano Mottola26, Nilda Oklay2, Frank Preusker26, Frank Scholten26, and Cecilia Tubiana2 (Affiliations can be found after the references) Received 26 February 2015 / Accepted 8 June 2015 ABSTRACT Aims. We derive for the first time the size-frequency distribution of boulders on a comet, 67P/Churyumov-Gerasimenko (67P), computed from the images taken by the Rosetta/OSIRIS imaging system. We highlight the possible physical processes that lead to these boulder size distributions. Methods. We used images acquired by the OSIRIS Narrow Angle Camera, NAC, on 5 and 6 August 2014. The scale of these images (2.44−2.03 m/px) is such that boulders ≥7 m can be identified and manually extracted from the datasets with the software ArcGIS. -

Livy, Folklore, and Magic: a Reappraisal of Rome's Foundational Mythology
LIVY, FOLKLORE, AND MAGIC: A REAPPRAISAL OF ROME'S FOUNDATIONAL MYTHOLOGY Jeremy Leonard Albrecht A Thesis Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of MASTER OF ARTS May 2020 Committee: Casey Stark, Advisor Amilcar Challu James Pfundstein © 2020 Jeremy Albrecht All Rights Reserved iii ABSTRACT Casey Stark, Advisor This paper argues for an additional manner in which the social and cultural history of Rome can be both examined and understand through the implementation of folkloric practices. While folklore and history are two distinct academic traditions, there exists a certain amount of overlap between the fields and this overlap is worth exploring in more detail. In the course of this paper, it is argued that many aspects of Roman social and cultural history can be understood and examined through folkloric means. In chapter one, a working definition of folklore is established and shown to apply to the foundational mythology of Rome as portrayed by Livy in his Ab Urbe Condita. Chapter two continues to examine Livy and provides an argument that, in the process of his writing, Livy himself was more concerned with a folkloric interpretation of Rome’s history than he was in staying firmly within the bounds of historical accuracy. Finally, chapter three branches off from Livy and focuses on the arcane and magical traditions which were prevalent in Rome to show that not only were folkloric traditions present in Rome’s traditional mythology, but can also be seen throughout the Republic and even into the early Empire. -

The Creation of the Gods According to Esna II, 163, 16-17
2018 9 Trabajos de Egiptología Papers on Ancient Egypt Trabajos de Egiptología The Tendrils of the Bat Emblem The High Priesthood of Memphis during the Old Kingdom Andrea RODRÍGUEZ VALLS and the First Intermediate Period: An Updated Study and Prosopography Workers in Perpetuity? Josep CERVELLÓ AUTUORI Notes about the mrt Workers of the Egyptian Middle Kingdom Based on the Stela CG 20516 Quelques observations sur l’écriture rétrograde Pablo M. ROSELL dans les tombes thébaines de l’époque tardive And Everything Began with Laughs and Tears… Silvia EINAUDI The Creation of the Gods According to Esna II, 163, 16-17; III 206, 8-9 (§13) and III, 272, 2-3: Interpreting Three Gold Coins from Ancient Egypt Precedents, Interpretation and the Ancient Near East at the Museo and Influences Casa de la Moneda, Madrid Josué SANTOS SAAVEDRA, Roger FORTEA BASTART Trabajos de Egiptología Miguel JARAMAGO Tabasety, the Temple Singer in Aarhus Egyptian Predynastic Lice Combs: Rogério SOUSA, Vinnie NØRSKOV Analysis of an Ancestral Tool Candelaria MARTÍN DEL RÍO ÁLVAREZ Who Painted the Tomb of Sennedjem? Gema MENÉNDEZ número 9 2018 And Everything Began with Laughs and Tears… The Creation of the Gods According to Esna II, 163, 16-17; III, 206, 8-9 (§13) and III, 272, 2-3: Precedents, Interpretation and Influences Josué SANTOS SAAVEDRA, Roger FORTEA BASTART Demiurge’s tears play a prominent role in ancient Egyptian cosmogonic traditions as far as the genesis of the human being is concerned. However, the creation of the gods as a consequence of the demiurge’s laughter seems to be a unicum of the texts of the temple of Esna. -

“Supra-Practical” Aspects of Mutilation in the Egyptian New Kingdom
Journal of the Economic and Social History of the Orient 60 (2017) 263-291 brill.com/jesh May my nose and ears be cut off: Practical and “supra-practical” Aspects of Mutilation in the Egyptian New Kingdom Alexandre Alexandrovich Loktionov University of Cambridge [email protected] Abstract This paper investigates mutilation of the nose and ears in New Kingdom Egypt (c. 1550- 1070BCE). The topic is first contextualised within cross-cultural mutilation research, before discussion shifts to focus more closely on Egypt. The threat of mutilation in oaths is considered, as is the possibility of mutilation not being enforced if such oaths were broken. The paper then investigates the lived experience of mutilation, encom- passing both physiological and social impairments. Finally, a ‘supra-practical’ aspect is proposed, considering the esoteric connotations of mutilation, this latter understood as a set of practices including but not confined to actual physical dismemberment. Keywords Mutilation – corporal punishment – lived experience – nose – ears * I am very grateful to Dr. Kate Spence and Dr. Hratch Papazian, both of the University of Cam- bridge, for their feedback on a draft of this paper. I also acknowledge the comments of four anonymous JESHO reviewers. For funding the main research, my thanks go to the Master and Fellows of St John’s College, Cambridge, who provided a Benefactors Research Scholarship. For funding subsequent refinements and the completion of this article, I must thank the Arts and Humanities Doctoral Training Partnership (AHRC DTP) of the University of Cambridge and Robinson College, Cambridge, who have supported my PhD through a Lewis-AHRC Stu- dentship (AH/L503897/1). -

The Historical Jesus and Mythical-Christ by Gerald Massey the Historical Jesus and Mythical-Christ
The Historical Jesus and Mythical-Christ by Gerald Massey The Historical Jesus and Mythical-Christ by Gerald Massey See "Natural Genesis." from the same author for original references Published in the 1900's In presenting my readers with some of the data which show that much of the Christian History was pre- extant as Egyptian Mythology. I have to ask you to bear in mind that the facts, like other foundations, have been buried out of sight for thousands of years in a hieroglyphical language, that was never really read by Greek or Roman, and could not be read until the lost clue was discovered by Champollion, almost the other day! In this way the original sources of our Mytholatry and Christology remained as hidden as those of the Nile, until the century in which we live. The mystical matter enshrouded in this language was sacredly entrusted to the keeping of the buried dead, who have faithfully preserved it as their Book of Life, which was placed beneath their pillows, or clasped to their bosoms, in their coffins and their tombs. Secondly, although I am able to read the hieroglyphics, nothing offered to you is based on my translation. I work too warily for that! The transcription and literal rendering of the hieroglyphic texts herein employed are by scholars of indisputable authority. There is no loophole of escape that way. I lectured upon the subject of Jesus many years ago. At that time I did not know how we had been misled, or that the "Christian scheme" (as it is aptly called) in the New Testament is a fraud, founded on a fable in the Old! I then accepted the Canonical Gospels as containing a veritable human history, and assumed, as others do, that the history proved itself. -

Legends of the Gods
LEGENDS OF THE GODS The Egyptian Texts, edited with Translations by E. A. Wallis Budge London, 1912 [Editorial note: Throughout the text "####" represents images which cannot be transcribed.] PREFACE The welcome which has been accorded to the volumes of this Series, and the fact that some of them have passed into second and third editions, suggest that these little books have been found useful by beginners in Egyptology and others. Hitherto the object of them has been to supply information about the Religion, Magic, Language, and History of the ancient Egyptians, and to provide editions of the original texts from which such information was derived. There are, however, many branches of Egyptology which need treatment in a similar manner in this Series, and it has been suggested in many quarters that the time has now arrived when the publication of a series of groups of texts illustrating Egyptian Literature in general might well be begun. Seeing that nothing is known about the authors of Egyptian works, not even their names, it is impossible to write a History of Egyptian Literature in the ordinary sense of the word. The only thing to be done is to print the actual works in the best and most complete form possible, with translations, and then to put them in the hands of the reader and leave them to his judgment. With this object in view, it has been decided to publish in the Series several volumes which shall be devoted to the reproduction in hieroglyphic type of the best and most typical examples of the various kinds of Egyptian Literature, with English translations, on a much larger scale than was possible in my "First Steps in Egyptian" or in my "Egyptian Reading Book." These volumes are intended to serve a double purpose, i.e., to supply the beginner in Egyptian with new material and a series of reading books, and to provide the general reader with translations of Egyptian works in a handy form. -

Death and Salvation in Ancient Egypt
Death and Salvation in Ancient Egypt by JAN ASSMANN Translated from the German by DAVID LORTON Abridged and updated by the author cornell university press Ithaca and London Original German edition, Tod und Jenseits im alten Ägypten, copyright © 2001 by C. H. Beck, Munich. All rights reserved. English translation copyright © 2005 by Cornell University The translation of this work was published with the assistance of Inter Nationes. All rights reserved. Except for brief quotations in a review, this book, or parts thereof, must not be reproduced in any form without permission in writing from the publisher. For information, address Cornell University Press, Sage House, 512 East State Street, Ithaca, New York 14850. English translation first published 2005 by Cornell University Press Printed in the United States of America Library of Congress Cataloging-in-Publication Data Assmann, Jan. [Tod und Jenseits im Alten Ägypten. English] Death and salvation in ancient Egypt / by Jan Assmann ; translated from the German by David Lorton. p. cm. Includes bibliographical references and indexes. ISBN 0-8014-4241-9 (cloth : alk. paper) 1. Eschatology, Egyptian. 2. Egypt—Religion. 3. Death—Religious aspects. I. Title. BL2450.E8A8813 2005 299¢.3123—dc22 2005002783 Cornell University Press strives to use environmentally responsible suppliers and materials to the fullest extent possible in the publishing of its books. Such materials include vegetable-based, low-VOC inks and acid-free papers that are recycled, totally chlorine-free, or partly composed of nonwood fibers. For further information, visit our website at www.cornellpress.cornell.edu. Cloth printing 10987654321 Permit me, permit me, my good engineer, to tell you something, to lay it upon your heart.