Desk Review Cover and Contents.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Usg Humanitarian Assistance to Burma
USG HUMANITARIAN ASSISTANCE TO BURMA RANGOON CITY AREA AFFECTED AREAS Affected Townships (as reported by the Government of Burma) American Red Cross aI SOURCE: MIMU ASEAN B Implementing NGO aD BAGO DIVISION IOM B Kyangin OCHA B (WEST) UNHCR I UNICEF DG JF Myanaung WFP E Seikgyikanaunglo WHO D UNICEF a WFP Ingapu DOD E RAKHINE b AYEYARWADY Dala STATE DIVISION UNICEF a Henzada WC AC INFORMA Lemyethna IC TI Hinthada PH O A N Rangoon R U G N O I T E G AYEYARWADY DIVISION ACF a U Zalun S A Taikkyi A D ID F MENTOR CARE a /DCHA/O D SC a Bago Yegyi Kyonpyaw Danubyu Hlegu Pathein Thabaung Maubin Twantay SC RANGOON a CWS/IDE AC CWS/IDE AC Hmawbi See Inset WC AC Htantabin Kyaunggon DIVISION Myaungmya Kyaiklat Nyaungdon Kayan Pathein Einme Rangoon SC/US JCa CWS/IDE AC Mayangone ! Pathein WC AC Î (Yangon) Thongwa Thanlyin Mawlamyinegyun Maubin Kyauktan Kangyidaunt Twantay CWS/IDE AC Myaungmya Wakema CWS/IDE Kyauktan AC PACT CIJ Myaungmya Kawhmu SC a Ngapudaw Kyaiklat Mawlamyinegyun Kungyangon UNDP/PACT C Kungyangon Mawlamyinegyun UNICEF Bogale Pyapon CARE a a Kawhmu Dedaye CWS/IDE AC Set San Pyapon Ngapudaw Labutta CWS/IDE AC UNICEF a CARE a IRC JEDa UNICEF a WC Set San AC SC a Ngapudaw Labutta Bogale KEY SC/US JCa USAID/OFDA USAID/FFP DOD Pyinkhayine Island Bogale A Agriculture and Food Security SC JC a Air Transport ACTED AC b Coordination and Information Management Labutta ACF a Pyapon B Economy and Market Systems CARE C !Thimphu ACTED a CARE Î AC a Emergency Food Assistance ADRA CWS/IDE AC CWS/IDE aIJ AC Emergency Relief Supplies Dhaka IOM a Î! CWS/IDE AC a UNICEF a D Health BURMA MERLIN PACT CJI DJ E Logistics PACT ICJ SC a Dedaye Vientiane F Nutrition Î! UNDP/PACT Rangoon SC C ! a Î ACTED AC G Protection UNDP/PACT C UNICEF a Bangkok CARE a IShelter and Settlements Î! UNICEF a WC AC J Water, Sanitation, and Hygiene WC WV GCJI AC 12/19/08 The boundaries and names used on this map do not imply official endorsement or acceptance by the U.S. -

Rail Infrastructure Development Plan and Planning for International Railway Connectivity in Myanmar
THE REPUBLIC OF THE UNION OF MYANMAR MINISTRY OF TRANSPORT AND COMMUNICATIONS MYANMA RAILWAYS Expert Group Meeting on the Use of New Technologies for Facilitation of International Railway Transport 9-12 December, 2019 Rail Infrastructure Development Plan and Planning for International Railway Connectivity in Myanmar Ba Myint Managing Director Myanma Railways Ministry of Transport and Communications MYANMAR Contents . Brief Introduction on situation of Transport Infrastructure in Myanmar . Formulation of National Transport Master Plan . Preparation for the National Logistics Master Plan Study (MYL‐Plan) . Status of Myanma Railways and Current Rail Infrastructure Development Projects . Planning for International Railway Connectivity in Myanmar 2 Brief Introduction on situation of Transport Infrastructure in Myanmar Myanma’s Profile . Population – 54.283 Million(March,2018) India . Area ‐676,578 Km² China . Coastal Line ‐ 2800 km . Road Length ‐ approximately 150,000 km . Railways Route Length ‐ 6110.5 Km . GDP per Capita – 1285 USD in 2018 Current Status Lao . Myanmar’s Transport system lags behind ASEAN . 60% of highways and rail lines in poor condition Thailand . 20 million People without basic road access . $45‐60 Billion investments needs (2016‐ 2030) Reduce transport costs by 30% Raise GDP by 13% Provide basic road access to 10 million people and save People’s lives on the roads. 4 Notable Geographical Feature of MYANMAR India China Bangaladesh Lao Thailand . As land ‐ bridge between South Asia and Southeast Asia as well as with China . Steep and long mountain ranges hamper the development of transport links with neighbors. 5 Notable Geographical Feature China 1,340 Mil. India 1,210 mil. Situated at a cross‐road of 3 large economic centers. -

46399E642.Pdf
PGDS in DOS Myanmar Atlas Map Population and Geographic Data Section As of January 2006 Division of Operational Support Email : [email protected] ((( Yüeh-hsi ((( ((( Zayü ((( ((( BANGLADESHBANGLADESH ((( Xichang ((( Zhongdian ((( Ho-pien-tsun Cox'sCox's BazarBazar ((( ((( ((( ((( Dibrugrh ((( ((( ((( (((Meiyu ((( Dechang THIMPHUTHIMPHU ((( ((( ((( Myanmar_Atlas_A3PC.WOR ((( Ningnan ((( ((( Qiaojia ((( Dayan ((( Yongsheng KutupalongKutupalong ((( Huili ((( ((( Golaghat ((( Jianchuan ((( Huize ((( ((( ((( Cooch Behar ((( North Gauhati Nowgong (((( ((( Goalpara (((( Gauhati MYANMARMYANMAR ((( MYANMARMYANMAR ((( MYANMARMYANMAR ((( MYANMARMYANMAR ((( MYANMARMYANMAR ((( MYANMARMYANMAR ((( Dinhata ((( ((( Gauripur ((( Dongch ((( ((( ((( Dengchuan ((( Longjie ((( Lalmanir Hat ((( Yanfeng ((( Rangpur ((( ((( ((( ((( Yuanmou ((( Yangbi((( INDIAINDIA ((( INDIAINDIA ((( INDIAINDIA ((( INDIAINDIA ((( INDIAINDIA ((( INDIAINDIA ((( ((( ((( ((( ((( ((( ((( Shillong ((((( Xundia ((( ((( Hai-tzu-hsin ((( Yongping ((( Xiangyun ((( ((( ((( Myitkyina ((( ((( ((( Heijing ((( Gaibanda NayaparaNayapara ((((( ((( (Sha-chiao(( ((( ((( ((( ((( Yipinglang ((( Baoshan TeknafTeknaf ButhidaungButhidaung (((TeknafTeknaf ((( ((( Nanjian ((( !! ((( Tengchong KanyinKanyin((( ChaungChaung !! Kunming ((( ((( ((( Anning ((( ((( ((( Changning MaungdawMaungdaw ((( MaungdawMaungdaw ((( ((( Imphal Mymensingh ((( ((( ((( ((( Jiuyingjiang ((( ((( Longling 000 202020 404040 BANGLADESHBANGLADESH((( 000 202020 404040 BANGLADESHBANGLADESH((( ((( ((( ((( ((( Yunxian ((( ((( ((( ((( -

Supply Annual Report 2019 Scaling up for Impact 2 UNICEF Supply Annual Report 2019 SCALING up for IMPACT 3
Supply Annual Report 2019 Scaling Up for Impact 2 UNICEF Supply Annual Report 2019 SCALING UP FOR IMPACT 3 Students smile at the camera in front of their school in the village of Tamroro, in the centre of Niger 4 UNICEF Supply Annual Report 2019 SCALING UP FOR IMPACT 5 Contents Foreword 7 SCALING UP FOR IMPACT Innovation at the heart of humanitarian response 10 From ships to schools: Finding construction solutions in local innovation 12 Warehouse in a pocket app scales up to improve supply chain efficiency 14 Scaling vaccine procurement in an evolving landscape of supply and demand 16 Strengthening domestic resources to deliver life-saving commodities 18 WORKING TOGETHER Keeping vaccines safe through the last mile of their journey 20 The UNICEF Supply Community behind our results 42 Improving nutrition supply chains for children 22 Supply Community testimonials 44 Strategic collaboration 46 Supply partnerships 48 RESPONDING TO EMERGENCIES UNICEF on the front lines 26 UNICEF supply response in the highest-level ACHIEVING RESULTS emergencies in 2019 28 Procurement overview 2019 52 Emergency overview highlights by country 30 Major commodity groups 54 Scaling up supply response Services 56 for global health emergencies 32 Country of supplier / Region of use 57 Juliette smiles on Responding with supplies the playground inside to Cyclones Idai and Kenneth 36 Savings overview 2019 58 Reaching new heights, a youth-friendly space in the Mahama Refugee Camp, home to thousands of Strategic prepositioning of supplies Burundian children, in South Sudan 38 ANNEXES such as herself for every child. Scaling up construction in Yemen 39 UNICEF global procurement statistics 60 6 UNICEF Supply Annual Report 2019 Foreword 7 Scaling up for impact In 2019, UNICEF annual procurement of goods and services for children reached a record $3.826 billion. -

Mimu875v01 120626 3W Livelihoods South East
Myanmar Information Management Unit 3W South East of Myanmar Livelihoods Border and Country Based Organizations Presence by Township Budalin Thantlang 94°23'EKani Wetlet 96°4'E Kyaukme 97°45'E 99°26'E 101°7'E Ayadaw Madaya Pangsang Hakha Nawnghkio Mongyai Yinmabin Hsipaw Tangyan Gangaw SAGAING Monywa Sagaing Mandalay Myinmu Pale .! Pyinoolwin Mongyang Madupi Salingyi .! Matman CHINA Ngazun Sagaing Tilin 1 Tada-U 1 1 2 Monghsu Mongkhet CHIN Myaing Yesagyo Kyaukse Myingyan 1 Mongkaung Kyethi Mongla Mindat Pauk Natogyi Lawksawk Kengtung Myittha Pakokku 1 1 Hopong Mongping Taungtha 1 2 Mongyawng Saw Wundwin Loilen Laihka Ü Nyaung-U Kunhing Seikphyu Mahlaing Ywangan Kanpetlet 1 21°6'N Paletwa 4 21°6'N MANDALAY 1 1 Monghpyak Kyaukpadaung Taunggyi Nansang Meiktila Thazi Pindaya SHAN (EAST) Chauk .! Salin 4 Mongnai Pyawbwe 2 Tachileik Minbya Sidoktaya Kalaw 2 Natmauk Yenangyaung 4 Taunggyi SHAN (SOUTH) Monghsat Yamethin Pwintbyu Nyaungshwe Magway Pinlaung 4 Mawkmai Myothit 1 Mongpan 3 .! Nay Pyi Hsihseng 1 Minbu Taw-Tatkon 3 Mongton Myebon Langkho Ngape Magway 3 Nay Pyi Taw LAOS Ann MAGWAY Taungdwingyi [(!Nay Pyi Taw- Loikaw Minhla Nay Pyi Pyinmana 3 .! 3 3 Sinbaungwe Taw-Lewe Shadaw Pekon 3 3 Loikaw 2 RAKHINE Thayet Demoso Mindon Aunglan 19°25'N Yedashe 1 KAYAH 19°25'N 4 Thandaunggyi Hpruso 2 Ramree Kamma 2 3 Toungup Paukkhaung Taungoo Bawlakhe Pyay Htantabin 2 Oktwin Hpasawng Paungde 1 Mese Padaung Thegon Nattalin BAGOPhyu (EAST) BAGO (WEST) 3 Zigon Thandwe Kyangin Kyaukkyi Okpho Kyauktaga Hpapun 1 Myanaung Shwegyin 5 Minhla Ingapu 3 Gwa Letpadan -
The Union Report the Union Report : Census Report Volume 2 Census Report Volume 2
THE REPUBLIC OF THE UNION OF MYANMAR The 2014 Myanmar Population and Housing Census The Union Report The Union Report : Census Report Volume 2 Volume Report : Census The Union Report Census Report Volume 2 Department of Population Ministry of Immigration and Population May 2015 The 2014 Myanmar Population and Housing Census The Union Report Census Report Volume 2 For more information contact: Department of Population Ministry of Immigration and Population Office No. 48 Nay Pyi Taw Tel: +95 67 431 062 www.dop.gov.mm May, 2015 Figure 1: Map of Myanmar by State, Region and District Census Report Volume 2 (Union) i Foreword The 2014 Myanmar Population and Housing Census (2014 MPHC) was conducted from 29th March to 10th April 2014 on a de facto basis. The successful planning and implementation of the census activities, followed by the timely release of the provisional results in August 2014 and now the main results in May 2015, is a clear testimony of the Government’s resolve to publish all information collected from respondents in accordance with the Population and Housing Census Law No. 19 of 2013. It is my hope that the main census results will be interpreted correctly and will effectively inform the planning and decision-making processes in our quest for national development. The census structures put in place, including the Central Census Commission, Census Committees and Offices at all administrative levels and the International Technical Advisory Board (ITAB), a group of 15 experts from different countries and institutions involved in censuses and statistics internationally, provided the requisite administrative and technical inputs for the implementation of the census. -
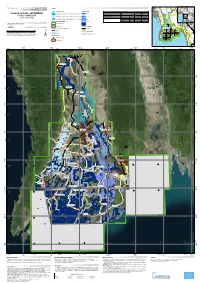
Irrawaddy Delta - MYANMAR Flooded Area Delineation 11/08/2015 11:46 UTC River R
Nepal (!Loikaw GLIDE number: N/A Activation ID: EMSR130 I Legend r n r India China e Product N.: 16IRRAWADDYDELTA, v2, English Magway a Rakhine w Bangladesh e a w l d a Vietnam Crisis Information Hydrology Consequences within the AOI on 09, 10, 11/08/2015 d Myanmar S Affected Total in AOI y Nay Pyi Taw Irrawaddy Delta - MYANMAR Flooded Area delineation 11/08/2015 11:46 UTC River R ha 428922,1 i v Laos Flooded area e ^ r S Flood - 01/08/2015 Flooded Area delineation 10/08/2015 23:49 UTC Stream Estimated population Inhabitants 4252141 11935674 it Bay of ( to Settlements Built-up area ha 35491,8 75542,0 A 10 Bago n Bengal Thailand y g Delineation Map e Flooded Area delineation 09/08/2015 11:13 UTC Lake y P Transportation Railways km 26,0 567,6 a Cambodia r i w Primary roads km 33,0 402,1 Andam an n a Gulf of General Information d Sea g Reservoir Secondary roads km 57,2 1702,3 Thailand 09 y Area of Interest ) Andam an Cartographic Information River Sea Missing data Transportation Bay of Bengal 08 Bago Tak Full color ISO A1, low resolution (100 dpi) 07 1:600000 Ayeyarwady Yangon (! Administrative boundaries Railway Kayin 0 12,5 25 50 Region km Primary Road Pathein 06 04 11 12 (! Province Mawlamyine Grid: WGS 1984 UTM Zone 46N map coordinate system Secondary Road 13 (! Tick marks: WGS 84 geographical coordinate system ± Settlements 03 02 01 ! Populated Place 14 15 Built-Up Area Gulf of Martaban Andaman Sea 650000 700000 750000 800000 850000 900000 950000 94°10'0"E 94°35'0"E 95°0'0"E 95°25'0"E 95°50'0"E 96°15'0"E 96°40'0"E 97°5'0"E N " 0 ' 5 -

October Chronology (Eng)
October 2015, Chronology Summary of the Current Situation As of the end of October, there are 112 political prisoners incarcerated in Burma and 486 activists currently awaiting trial for political actions. Detained Facebook Activists Patrick Kum Jaa Lee and Chaw Sandy Tun Accessed October 2015 Table of Contents Month in Review Detentions Incarcerations Conditions of Detentions Demonstrations and Related Restrictions on Political and Civil Liberties Land Issues Key International and Domestic Developments Conclusion Links and Resources “There can be no national reconciliation in Burma, as long as there are political prisoners” October 2015, Chronology MONTH IN REVIEW This month, 10 political activists were arrested political prisoners is preventing the upcoming in total, eight of whom are detained. Thirty- election from being free and fair. One were sentenced, and eight were released. Despite concerns over the legitimacy of the Nine political prisoners are reported to be in upcoming election, new arrests continued this bad health. month. Lu Zaw Soe Win, Patrick Kum Jaa Lee The Letpadan case was still not resolved this and Chaw Sandy Tun were all arrested and month, and 61 students and activists remain detained for allegedly posting to Facebook detained for charges relating to their images or insults defaming the government and participation in the National Education Bill received charges either under the protests in March. Fortify Rights and the Telecommunications Law or the Electronic Harvard Law School International Human Transactions Law. Patrick Kum Jaa Lee and Rights Clinic released a report detailing the Chaw Sandy Tun remain in detention. Maung abusive tactics used by police officials in the Saungkha also received charges under the violent crackdown. -

Ending Child Marriage and Stopping the Spread of HIV in Africa WHAT CAN BE DONE?
Webinar: Ending Child Marriage and Stopping the Spread of HIV in Africa WHAT CAN BE DONE? Webinar hosted by RIATT-ESA and The African Union DATE: 20 JUNE, 2017 Time 3pm east Africa/ 2 pm southern Africa/ 1pm UK Moderated by Ms Nyaradzayi, Gumbonzvanda - AU Goodwill Ambassador on Ending Child Marriage and Chief Executive Officer, Rozaria Memorial Trust. @vanyaradzayi Contact: www.riatt-esa.org @RIATTESA 1 Your first webinar? Don’t worry we got you covered. Attending a RIATT-ESA webinar is easier than riding a Raise your virtual hand to ask bike. Here is how you do it. an audio question at the end • When you first join a session, the Control Panel appears on the right side of your screen. Use the Control Panel to Type your comments and manage your session. questions here • Put your headphones on and turn up the sound. Type question here • During the webinar the attendees will be muted. But you can send us questions at any point via the chat box. • The panellists will answer your questions in the question and answer session. • If you have to step out don’t worry, the webinar is being recorded and you can watch it later. 2 About RIATT-ESA and The AU The Regional Inter-Agency Task Team on Children and AIDS in Eastern and Southern Africa (RIATT-ESA) is a unique, multi-sectoral partnership of organisations. Though a evidence driven approach RIATT-ESA influences global, regional and national policy formulation and implementation for children and their families affected by AIDS in eastern and southern Africa. -

Country Reports on Human Rights Practices - 2005 Released by the Bureau of Democracy, Human Rights, and Labor March 8, 2006
Burma Page 1 of 24 2005 Human Rights Report Released | Daily Press Briefing | Other News... Burma Country Reports on Human Rights Practices - 2005 Released by the Bureau of Democracy, Human Rights, and Labor March 8, 2006 Since 1962, Burma, with an estimated population of more than 52 million, has been ruled by a succession of highly authoritarian military regimes dominated by the majority Burman ethnic group. The current controlling military regime, the State Peace and Development Council (SPDC), led by Senior General Than Shwe, is the country's de facto government, with subordinate Peace and Development Councils ruling by decree at the division, state, city, township, ward, and village levels. In 1990 prodemocracy parties won more than 80 percent of the seats in a generally free and fair parliamentary election, but the junta refused to recognize the results. Twice during the year, the SPDC convened the National Convention (NC) as part of its purported "Seven-Step Road Map to Democracy." The NC, designed to produce a new constitution, excluded the largest opposition parties and did not allow free debate. The military government totally controlled the country's armed forces, excluding a few active insurgent groups. The government's human rights record worsened during the year, and the government continued to commit numerous serious abuses. The following human rights abuses were reported: abridgement of the right to change the government extrajudicial killings, including custodial deaths disappearances rape, torture, and beatings of -

Return Assessments - Bago East Myanmar South East Operation - UNHCR Hpa-An 30 June 2017
Return Assessments - Bago East Myanmar South East Operation - UNHCR Hpa-An 30 June 2017 Background information Since June 2013, UNHCR has been piloting a system to assess spontaneous returns in the Southeast of Myanmar, a process that may start in the absence of an organized Voluntary Repatriation operation. Total Assessments 9 A verified return village, therefore, is a village where UNHCR field staff have confirmed there are refugees and/or IDPs who have returned since January 2012 with the intention of remaining Verified Return Villages permanently. During the assessments, communities are also asked whether their village is a refugee 4 village of origin, by definition a village that is home to people residing in a refugee camp in Thailand. A village where UNHCR completes an assessment can be both a verified return village and a refugee Refugee Villages of Origin 3 village of origin, as the two are not mutually exclusive. Using a “do no harm” approach based around community level discussion, the return assessment collect information about the patterns and needs of returnees in the Southeast. The project does not, however, attempt to represent the total number of returnees in a state, or the region as a whole. The returnee monitoring project has been underway in Kayah State, Mon State and Tanintharyi Region since June 2013, and expanded to Kayin State in December 2013. Verified Return Villages by Township Loikaw Nay Pyi Taw Shan StateMai Nai Soi Camp ± Kyaukkyi 7 3 Magway Mae Surin Camp Region Thanatpin 1 0 Yedashe !. Kayah State Waw 1 1 Taungoo !. Assessments Verified Return Villages Oktwin !. -

Our Community Work in AFRICA
Our Community Work in AFRICA ohnson & Johnson has a long legacy of giving, with hundreds of programs Jsupported around the world each year. Our philanthropic mission is to make life-changing, long-term differences in human health by targeting the world’s major health-related issues. Our community work in Africa dates back over 80 years. Working together with over 100 community-based partners, we support efforts in more than 30 African countries. We focus on saving and improving the lives of women and children, preventing disease among the most vulnerable, and strengthening the health care workforce. The programs here highlight some examples of our efforts throughout Africa to help those most in need. Our Community Work in AFRICA with Save the Children. The partnership SAVING AND IMPROVING has trained almost 1000 skilled birth attendants, mostly midwives, in its THE LIVES OF WOMEN first 3 years. The program is designed for national scale-up by Ministries of Health in the longer term. In Kenya, AND CHILDREN Johnson & Johnson collaborates with the American Academy of Pediatrics and Amref Health Africa to provide HBB Reducing Neonatal training to midwives. Johnson & Johnson Improving Maternal & also partners with UN’s Health 4+ Mortality to train skilled birth attendants in Infant Health emergency obstetric and newborn care in Ethiopia and Tanzania, where neonatal mortality is high. Partnerships to End Fistula Johnson & Johnson has been a pioneer in investing in partners and programs that reduce the suffering and stigma of obstetric fistula, a birth injury caused by prolonged labor common in areas where it is difficult to access proper care.