Direct Thrombin Inhibitors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Enoxaparin Sodium Solution for Injection, Manufacturer's Standard
PRODUCT MONOGRAPH INCLUDING PATIENT MEDICATION INFORMATION PrLOVENOX® Enoxaparin sodium solution for injection 30 mg in 0.3 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 40 mg in 0.4 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 60 mg in 0.6 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 80 mg in 0.8 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 100 mg in 1 mL solution (100 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 300 mg in 3 mL solution (100 mg/mL), multidose vials for subcutaneous or intravenous injection PrLOVENOX® HP Enoxaparin sodium (High Potency) solution for injection 120 mg in 0.8 mL solution (150 mg/mL), pre-filled syringes for subcutaneous or intravenous injection 150 mg in 1 mL solution (150 mg/mL), pre-filled syringes for subcutaneous or intravenous injection Manufacturer’s standard Anticoagulant/Antithrombotic Agent ATC Code: B01AB05 Product Monograph – LOVENOX (enoxaparin) Page 1 of 113 sanofi-aventis Canada Inc. Date of Initial Approval: 2905 Place Louis-R.-Renaud February 9, 1993 Laval, Quebec H7V 0A3 Date of Revision September 7, 2021 Submission Control Number: 252514 s-a version 15.0 dated September 7, 2021 Product Monograph – LOVENOX (enoxaparin) Page 2 of 113 TABLE OF CONTENTS Sections or subsections that are not applicable at the time of authorization are not listed. TABLE OF CONTENTS .............................................................................................................. -

Evaluation of Clopidogrel Conjugation
DMD Fast Forward. Published on July 11, 2016 as DOI: 10.1124/dmd.116.071092 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 71092 TITLE PAGE EVALUATION OF CLOPIDOGREL CONJUGATION METABOLISM: PK STUDIES IN MAN AND MICE OF CLOPIDOGREL ACYL GLUCURONIDE Simona Nicoleta Savu, Luigi Silvestro, Mariana Surmeian, Lina Remis, Downloaded from Yuksel Rasit, Simona Rizea Savu, Constantin Mircioiu University of Medicine and Pharmacy "Carol Davila", Faculty of Pharmacy, Department of dmd.aspetjournals.org Biopharmacy, Bucharest, Romania (S.N.S., M.C.); 3S-Pharmacological Consultation & Research GmbH, Koenigsbergerstrasse 1 – 27243 Harpstedt, ; Germany (S.N.S, L.S., S.R.S.) at ASPET Journals on September 23, 2021 Pharma Serv International SRL., 52 Sabinelor Street, 5th District, 050853 Bucharest, Romania (M.S.); Clinical Hospital of the Ministry of Health of the Moldavian Republic, 51 Puskin Street, MD-2005 Chisinau, The Moldavian Republic (L.R.) National Institute for Chemical Pharmaceutical Research and Development (ICCF), Pharmacology Department, 112 Vitan Avenue, 3rd District, 031299 Bucharest, Romania (Y. R.) 1 DMD Fast Forward. Published on July 11, 2016 as DOI: 10.1124/dmd.116.071092 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 71092 RUNNING TITLE PAGE Running title: PK STUDIES IN MAN AND MICE OF CLOPIDOGREL ACYL GLUCURONIDE Corresponding author: Simona Nicoleta Savu Address: 52 Sabinelor Street, 5th District, 050853 Bucharest, Romania Downloaded from Mobile phone: +40 758 109 202 E-mail: [email protected] dmd.aspetjournals.org Document statistics: Abstract - 242 Introduction - 748 at ASPET Journals on September 23, 2021 Discussion - 1297 Tables - 2 Figures - 6 References - 34 Nonstandard abbreviations: AUC0-t - area under the curve from time 0 until the last quantifiable point AUC0-inf - area under the curve from time 0 to infinite CAG - clopidogrel acyl glucuronide CCA – clopidogrel carboxylic acid 2 DMD Fast Forward. -

Rivaroxaban Versus Warfarin for Treatment and Prevention Of
Costa et al. Thrombosis Journal (2020) 18:6 https://doi.org/10.1186/s12959-020-00219-w RESEARCH Open Access Rivaroxaban versus warfarin for treatment and prevention of recurrence of venous thromboembolism in African American patients: a retrospective cohort analysis Olivia S. Costa1,2, Stanley Thompson3, Veronica Ashton4, Michael Palladino5, Thomas J. Bunz6 and Craig I. Coleman1,2* Abstract Background: African Americans are under-represented in trials evaluating oral anticoagulants for the treatment of acute venous thromboembolism (VTE). The aim of this study was to evaluate the effectiveness and safety of rivaroxaban versus warfarin for the treatment of VTE in African Americans. Methods: We utilized Optum® De-Identified Electronic Health Record data from 11/1/2012–9/30/2018. We included African Americans experiencing an acute VTE during a hospital or emergency department visit, who received rivaroxaban or warfarin as their first oral anticoagulant within 7-days of the acute VTE event and had ≥1 provider visit in the prior 12-months. Differences in baseline characteristics between cohorts were adjusted using inverse probability-of-treatment weighting based on propensity scores (standard differences < 0.10 were achieved for all covariates). Our primary endpoint was the composite of recurrent VTE or major bleeding at 6-months. Three- and 12-month timepoints were also assessed. Secondary endpoints included recurrent VTE and major bleeding as individual endpoints. Cohort risk was compared using Cox regression and reported as hazard ratios (HRs) with 95% confidence intervals (CIs). Results: We identified 2097 rivaroxaban and 2842 warfarin users with incident VTE. At 6-months, no significant differences in the composite endpoint (HR = 0.96, 95%CI = 0.75–1.24), recurrent VTE (HR = 1.02, 95%CI = 0.76–1.36) or major bleeding alone (HR = 0.93, 95%CI = 0.59–1.47) were observed between cohorts. -

Surfen, a Small Molecule Antagonist of Heparan Sulfate
Surfen, a small molecule antagonist of heparan sulfate Manuela Schuksz*†, Mark M. Fuster‡, Jillian R. Brown§, Brett E. Crawford§, David P. Ditto¶, Roger Lawrence*, Charles A. Glass§, Lianchun Wang*, Yitzhak Torʈ, and Jeffrey D. Esko*,** *Department of Cellular and Molecular Medicine, Glycobiology Research and Training Center, †Biomedical Sciences Graduate Program, ‡Department of Medicine, Division of Pulmonary and Critical Care Medicine and Veteran’s Administration San Diego Medical Center, ¶Moores Cancer Center, and ʈDepartment of Chemistry and Biochemistry, University of California at San Diego, La Jolla, CA 92093; and §Zacharon Pharmaceuticals, Inc, 505 Coast Blvd, South, La Jolla, CA 92037 Communicated by Carolyn R. Bertozzi, University of California, Berkeley, CA, June 18, 2008 (received for review May 26, 2007) In a search for small molecule antagonists of heparan sulfate, Surfen (bis-2-methyl-4-amino-quinolyl-6-carbamide) was first we examined the activity of bis-2-methyl-4-amino-quinolyl-6- described in 1938 as an excipient for the production of depot carbamide, also known as surfen. Fluorescence-based titrations insulin (16). Subsequent studies have shown that surfen can indicated that surfen bound to glycosaminoglycans, and the extent block C5a receptor binding (17) and lethal factor (LF) produced of binding increased according to charge density in the order by anthrax (18). It was also reported to have modest heparin- heparin > dermatan sulfate > heparan sulfate > chondroitin neutralizing effects in an oral feeding experiments in rats (19), sulfate. All charged groups in heparin (N-sulfates, O-sulfates, and but to our knowledge, no further studies involving heparin have carboxyl groups) contributed to binding, consistent with the idea been conducted, and its effects on HS are completely unknown. -

Kengrexal, INN-Cangrelor Tetrasodium
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Kengrexal 50 mg powder for concentrate for solution for injection/infusion 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each vial contains cangrelor tetrasodium corresponding to 50 mg cangrelor. After reconstitution 1 mL of concentrate contains 10 mg cangrelor. After dilution 1 mL of solution contains 200 micrograms cangrelor. Excipient with known effect Each vial contains 52.2 mg sorbitol. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Powder for concentrate for solution for injection/infusion. White to off-white lyophilised powder. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Kengrexal, co-administered with acetylsalicylic acid (ASA), is indicated for the reduction of thrombotic cardiovascular events in adult patients with coronary artery disease undergoing percutaneous coronary intervention (PCI) who have not received an oral P2Y12 inhibitor prior to the PCI procedure and in whom oral therapy with P2Y12 inhibitors is not feasible or desirable. 4.2 Posology and method of administration Kengrexal should be administered by a physician experienced in either acute coronary care or in coronary intervention procedures and is intended for specialised use in an acute and hospital setting. Posology The recommended dose of Kengrexal for patients undergoing PCI is a 30 micrograms/kg intravenous bolus followed immediately by 4 micrograms/kg/min intravenous infusion. The bolus and infusion should be initiated prior to the procedure and continued for at least two hours or for the duration of the procedure, whichever is longer. At the discretion of the physician, the infusion may be continued for a total duration of four hours, see section 5.1. -

The Evolving Role of Direct Thrombin Inhibitors in Acute Coronary
View metadata, citation and similar papers at core.ac.uk brought to you by CORE Journal of the American College of Cardiology providedVol. by 41, Elsevier No. 4 - SupplPublisher S Connector © 2003 by the American College of Cardiology Foundation ISSN 0735-1097/03/$30.00 Published by Elsevier Science Inc. PII S0735-1097(02)02687-6 The Evolving Role of Direct Thrombin Inhibitors in Acute Coronary Syndromes John Eikelboom, MBBS, MSC, FRACP, FRCPA,* Harvey White, MB, CHB, DSC, FRACP, FACC,† Salim Yusuf, MBBS, DPHIL, FRCP (UK), FRCPC, FACC‡ Perth, Australia; Auckland, New Zealand; and Hamilton, Ontario, Canada The central role of thrombin in the initiation and propagation of intravascular thrombus provides a strong rationale for direct thrombin inhibitors in acute coronary syndromes (ACS). Direct thrombin inhibitors are theoretically likely to be more effective than indirect thrombin inhibitors, such as unfractionated heparin or low-molecular-weight heparin, because the heparins block only circulating thrombin, whereas direct thrombin inhibitors block both circulating and clot-bound thrombin. Several initial phase 3 trials did not demonstrate a convincing benefit of direct thrombin inhibitors over unfractionated heparin. However, the Direct Thrombin Inhibitor Trialists’ Collaboration meta-analysis confirms the superiority of direct thrombin inhibitors, particularly hirudin and bivalirudin, over unfractionated heparin for the prevention of death or myocardial infarction (MI) during treatment in patients with ACS, primarily due to a reduction in MI (odds ratio, 0.80; 95% confidence interval, 0.70 to 0.91) with little impact on death. The absolute risk reduction in the composite of death or MI at the end of treatment (0.8%) was similar at 30 days (0.7%), indicating no loss of benefit after cessation of therapy. -

Dermatan Sulfate Composition
Europäisches Patentamt *EP000671414B1* (19) European Patent Office Office européen des brevets (11) EP 0 671 414 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.7: C08B 37/00, A61K 31/715 of the grant of the patent: 02.01.2002 Bulletin 2002/01 (86) International application number: PCT/JP94/01643 (21) Application number: 94927827.9 (87) International publication number: (22) Date of filing: 30.09.1994 WO 95/09188 (06.04.1995 Gazette 1995/15) (54) DERMATAN SULFATE COMPOSITION AS ANTITHROMBOTIC DERMATANSULFATEZUSAMMENSETZUNG ALS ANTITHROMOTISCHES MITTEL COMPOSITION DE DERMATANE SULFATE UTILISE COMME ANTITHROMBOTIQUE (84) Designated Contracting States: • YOSHIDA, Keiichi AT BE CH DE DK ES FR GB IT LI NL PT SE Tokyo 189 (JP) (30) Priority: 30.09.1993 JP 26975893 (74) Representative: Davies, Jonathan Mark Reddie & Grose 16 Theobalds Road (43) Date of publication of application: London WC1X 8PL (GB) 13.09.1995 Bulletin 1995/37 (56) References cited: (60) Divisional application: EP-A- 0 112 122 EP-A- 0 199 033 01201321.5 / 1 125 977 EP-A- 0 238 994 WO-A-93/05074 JP-A- 59 138 202 JP-B- 2 100 241 (73) Proprietor: SEIKAGAKU KOGYO KABUSHIKI JP-B- 6 009 042 KAISHA Tokyo 103 (JP) • CARBOHYDRATE RESEARCH , vol. 131, no. 2, 1984 NL, pages 301-314, K. NAGASAWA ET AL. (72) Inventors: ’The structure of rooster-comb dermatan • TAKADA, Akikazu sulfate. Characterization and quantitative Shizuoka 431-31 (JP) determination of copolymeric, isomeric tetra- • ONAYA, Junichi and hexa-saccharides’ Higashiyamato-shi Tokyo 207 (JP) • ARAI, Mikio Remarks: Higashiyamato-shi Tokyo 207 (JP) The file contains technical information submitted • MIYAUCHI, Satoshi after the application was filed and not included in this Tokyo 208 (JP) specification • KYOGASHIMA, Mamoru Tokyo 207 (JP) Note: Within nine months from the publication of the mention of the grant of the European patent, any person may give notice to the European Patent Office of opposition to the European patent granted. -

201370Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 201370Orig1s000 MEDICAL REVIEW(S) M E M O R A N D U M DEPARTMENT OF HEALTH AND HUMAN SERVICES PUBLIC HEALTH SERVICE FOOD AND DRUG ADMINISTRATION CENTER FOR DRUG EVALUATION AND RESEARCH Date: July 8, 2011 From: Kathy M. Robie-Suh, M.D., Ph.D. Medical Team Leader Division of Hematology Products Subject: NDA 201370, resubmission April 11, 2011 Heparin Sodium Injection (heparin sodium, USP) Sponsor: Pfizer, Inc. 235 East 42nd Street New York, NY 10017-5755 To: NDA 201370 This is the second review cycle for this 505(b)(2) application for a new Heparin Sodium Injection product derived from porcine intestine. The presentations include several containing benzyl alcohol as a preservative and one preservative-free presentation. The first cycle review of the NDA found the application acceptable from a clinical viewpoint. However, manufacturing facilities inspection identified deficiencies that precluded approval and a Complete Response (CR) letter was issued on April 7, 2011. Labeling review was not completed at that time. In the current resubmission the sponsor has responded to the identified deficiencies deleting the two heparin supplier sites where deficiencies were found. The Amended Cross-Discipline Team Leader Review by Dr. Ali Al-Hakim (6/28/2011) comments that Office of Compliance has updated its recommendation in the Establishment Evaluation System and issued “ACCEPTABLE” overall recommendation for this NDA on June 27, 2011 and therefore the NDA is recommended for approval. No new clinical information is included in the resubmission. Clinical review of the original application and the resubmission was conducted by Dr. -
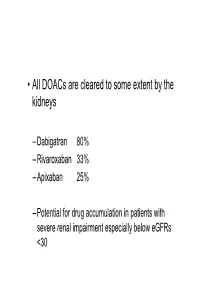
• All Doacs Are Cleared to Some Extent by the Kidneys
• All DOACs are cleared to some extent by the kidneys – Dabigatran 80% – Rivaroxaban 33% – Apixaban 25% – Potential for drug accumulation in patients with severe renal impairment especially below eGFRs <30 Warfarin is unaffected by renal impairment (only • Rivaroxaban & Apixaban are both oral direct inhibitor of factor Xa. • Rivaroxaban doses recommended for clinical use are 15mg od and 20 mg od (15 mg bd for first 3 weeks of treatment of DVT). • Apixaban 5mg bd or 2.5mg bd • Rivaroxaban peak plasma levels are reached 2 to 3 h after ingestion • Apixaban peak plasma levels are reached ~3hrs after ingestion • Rivaroxaban is taken with food – Apixaban without food • Rivaroxaban is 33% renaly excreted and has a half-life of 9 h in patients with normal renal function. – There is an analogy with Therapeutic LMWH – We very rarely ask for an anti-Xa assay • And what is the clinical significance of a Xa assay ? (Cut off values are largely arbitrary) – Fixed doses – Importance of When the last dose was taken ? – Importance of What is the renal function ? – If bleeding • What is the nature of the bleeding ? • In extremis we can give protamine sulphate (? Efficacy) • How to manage bleeding on a DOAC? –How severe is the bleeding ? –When was the last dose of medication ? –What is the renal function ? – Recheck –If minor bleeding; epistaxis, gingival, bruising, menorrhagia • Withhold the NOAC (when was the last dose taken?) • Recheck renal function • Check FBC • Local measures • Unlikely to require further intervention – Re-challenge – ? Switch NOAC -

Low Molecular Weight Heparins and Heparinoids
NEW DRUGS, OLD DRUGS NEW DRUGS, OLD DRUGS Low molecular weight heparins and heparinoids John W Eikelboom and Graeme J Hankey UNFRACTIONATED HEPARIN has been used in clinical ABSTRACT practice for more than 50 years and is established as an effective parenteral anticoagulant for the prevention and ■ Several low molecular weight (LMW) heparin treatment of various thrombotic disorders. However, low preparations, including dalteparin, enoxaparin and molecularThe Medical weight Journal (LMW) of heparinsAustralia haveISSN: recently 0025-729X emerged 7 October as nadroparin, as well as the heparinoid danaparoid sodium, more2002 convenient, 177 6 379-383 safe and effective alternatives to unfrac- are approved for use in Australia. 1 tionated©The heparin Medical (BoxJournal 1). of AustraliaIn Australia, 2002 wwwLMW.mja.com.au heparins are ■ LMW heparins are replacing unfractionated heparin for replacingNew Drugs,unfractionated Old Drugs heparin for preventing and treating the prevention and treatment of venous thromboembolism venous thromboembolism and for the initial treatment of and the treatment of non-ST-segment-elevation acute unstable acute coronary syndromes. The LMW heparinoid coronary syndromes. danaparoid sodium is widely used to treat immune heparin- ■ induced thrombocytopenia. The advantages of LMW heparins over unfractionated heparin include a longer half-life (allowing once-daily or twice-daily subcutaneous dosing), high bioavailability and Limitations of unfractionated heparin predictable anticoagulant response (avoiding the need -

Rtpa) for the Treatment of Hepatic Veno-Occlusive Disease (VOD
Bone Marrow Transplantation, (1999) 23, 803–807 1999 Stockton Press All rights reserved 0268–3369/99 $12.00 http://www.stockton-press.co.uk/bmt Recombinant tissue plasminogen activator (rtPA) for the treatment of hepatic veno-occlusive disease (VOD) S Kulkarni1, M Rodriguez2, A Lafuente2, P Mateos2, J Mehta1, S Singhal1, R Saso3, D Tait4, JG Treleaven3 and RL Powles1 Departments of 1Medical Oncology, 3Haematology and 4Radiotherapy, Royal Marsden NHS Trust, Sutton, Surrey, UK; and 2Haematology Department, Hospital La Paz, Madrid, Spain Summary: clinical syndrome characterized by hyperbilirubinemia, hepatomegaly and fluid retention,2,3 and results from dam- Seventeen patients who developed hepatic veno-occlus- age to structures in zone 3 of the liver acinus.4 In patients ive disease (VOD) following hematopoietic stem cell who have undergone hematopoietic stem cell transplan- transplantation were treated with recombinant tissue tation, chemoradiotherapy-induced endothelial cell damage plasminogen activator (rtPA) with or without heparin. is likely to be responsible for the pathogenesis of vessel rtPA was started a median of 13 days post transplant obstruction.5 (range 4–35). All patients received rtPA at a dose of 10 Treatment of established VOD has primarily been sup- mg/day as a starting dose, and 12 patients also received portive and any specific measures have resulted in little heparin (1500 U bolus; then 100 U/kg/day as a continu- impact on outcome. Based on the available evidence for ous i.v. infusion). The median number of days of rtPA involvement of hemostatic mechanisms and cytokines in therapy was 2.5 (1–12). The median total serum biliru- the pathogenesis of VOD,6–8 anti-thrombotic and anti-cyto- bin level was 116 mmol/l (range 63–194) at the begin- kine agents have been assessed for their role in treatment. -

Heparin Induced Thrombocytopenia – Adult – Inpatient– Clinical Practice Guideline
Heparin Induced Thrombocytopenia – Adult – Inpatient– Clinical Practice Guideline Table of Contents EXECUTIVE SUMMARY ........................................................................................................... 2 SCOPE ...................................................................................................................................... 6 METHODOLOGY ...................................................................................................................... 6 DEFINITIONS (OPTIONAL): ..................................................................................................... 7 INTRODUCTION ....................................................................................................................... 7 RECOMMENDATIONS .............................................................................................................. 7 BENEFITS/HARMS OF IMPLEMENTATION ...........................................................................17 IMPLEMENTATION PLAN AND TOOLS ........................ERROR! BOOKMARK NOT DEFINED. REFERENCES .........................................................................................................................17 APPENDIX A ............................................................................................................................17 Note: Active Table of Contents Click to follow link CPG Contact for Changes: CPG Contact for Content: Name: Philip J Trapskin, PharmD,BCPS Name: Anne E. Rose, PharmD Phone Number: 263-1328 Phone Number: