Chemotherapy-Induced Nausea and Vomiting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CP.PMN.158 Netupitant and Palonosetron (Akynzeo)
Clinical Policy: Netupitant and Palonosetron (Akynzeo), Fosnetupitant and Palonosetron (Akynzeo IV) Reference Number: CP.PMN.158 Effective Date: 09.01.06 Last Review Date: 02.21 Coding Implications Line of Business: HIM, Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Netupitant/palonosetron (Akynzeo®) and fosnetupitant/palonosetron are fixed combination products of netupitant, a substance P/neurokinin 1 (NK1) receptor antagonist, and palonosetron hydrochloride, a serotonin (5-HT3) receptor antagonist. FDA Approved Indication(s) Akynzeo capsules are indicated in combination with dexamethasone in adults for the prevention of acute and delayed nausea and vomiting associated with initial and repeat courses of cancer chemotherapy, including, but not limited to, highly emetogenic chemotherapy. Akynzeo for injection is indicated in combination with dexamethasone in adults for the prevention of acute and delayed nausea and vomiting associated with initial and repeat courses of highly emetogenic cancer chemotherapy. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Centene Corporation® that Akynzeo is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Prevention of Nausea and Vomiting Associated with Cancer Chemotherapy (must meet all): 1. Prescribed for the prevention of chemotherapy-induced nausea/vomiting; 2. Age ≥ 18 years; 3. If request is for Akynzeo capsules, member is scheduled to receive moderately to highly emetogenic cancer chemotherapy (see Appendix D); 4. If request is for Akynzeo for injection, member is scheduled to receive highly emetogenic cancer chemotherapy (see Appendix D); 5. -

203050Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 203050Orig1s000 LABELING HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------------CONTRAINDICATIONS-------------------------------- These highlights do not include all the information needed to use Hypersensitivity to the drug or any of its components (4) PALONOSETRON HYDROCHLORIDE INJECTION safely and effectively. See full prescribing information for PALONOSETRON ------------------------WARNINGS AND PRECAUTIONS------------------------- HYDROCHLORIDE INJECTION. • Hypersensitivity reactions, including anaphylaxis, have been reported with or without known hypersensitivity to other selective 5-HT3 receptor antagonists PALONOSETRON HYDROCHLORIDE injection, for intravenous (5.1) use • Serotonin syndrome has been reported with 5-HT3 receptor antagonists alone Initial U.S. Approval: 2003 but particularly with concomitant use of serotonergic drugs (5.2, 7.1) -------------------------INDICATIONS AND USAGE------------------------ --------------------------------ADVERSE REACTIONS------------------------------- Palonosetron Hydrochloride (HCl) Injection is a serotonin-3 (5-HT3) The most common adverse reactions in chemotherapy-induced nausea and receptor antagonist indicated in adults for: vomiting (≥5%) are headache and constipation (6.1) • Moderately emetogenic cancer chemotherapy -- prevention of acute and delayed nausea and vomiting associated with initial and repeat The most common adverse reactions in postoperative nausea and vomiting (≥ courses (1.1) 2%) are QT prolongation, -

Haloperidol As Prophylactic Treatment for Postoperative
Document downloaded from http://http://www.revcolanest.com.co, day 15/02/2013. This copy is for personal use. Any transmission of this document by any media or format is strictly prohibited. r e v c o l o m b a n e s t e s i o l . 2 0 1 3;4 1(1):34–43 Revista Colombiana de Anestesiología Colombian Journal of Anesthesiology www.revcolanest.com.co Review Haloperidol as prophylactic treatment for postoperative ଝ nausea and vomiting: Systematic literature review ∗ Catalina Chaparro , Diego Moreno, Verónica Ramírez, Angélica Fajardo, David González, Alejandra Sanín, Reinaldo Grueso Anesthesiology Service, Hospital Universitario San Ignacio, Bogotá, Colombia a r t i c l e i n f o a b s t r a c t Article history: Introduction: The effectiveness of haloperidol for the prophylaxis of postoperative nausea Received 3 July 2012 and vomiting (PONV) has been proven in prior trials summarized by Buttner in 2004. New Accepted 24 July 2012 evidence has surfaced since then. Our objective is thus to update the current knowledge on the topic. A systematic review and a meta-analysis were performed, in order to determine the effectiveness and safety of the use of haloperidol as prophylaxis for PONV. Keywords: Methodology: The systematic search, the selection of relevant articles, the extraction of data, Haloperidol the critical analysis of the primary studies, the comparisons and analyses were all based on Vomiting the recommendations of the Cochrane Collaboration and using RevMan5 software. Nausea Results: Ten controlled clinical trials published between 1962 and 2010, that included 2,711 Clinical trials patients, met the selection criteria. -

Safety and Efficacy of a Continuous Infusion, Patient Controlled Anti
Bone Marrow Transplantation, (1999) 24, 561–566 1999 Stockton Press All rights reserved 0268–3369/99 $15.00 http://www.stockton-press.co.uk/bmt Safety and efficacy of a continuous infusion, patient controlled anti- emetic pump to facilitate outpatient administration of high-dose chemotherapy SP Dix, MK Cord, SJ Howard, JL Coon, RJ Belt and RB Geller Blood and Marrow Transplant Program, Oncology and Hematology Associates and Saint Luke’s Hospital of Kansas City, Kansas City, MO, USA Summary: and colleagues1 described an outpatient BMT care model utilizing intensive clinic support following inpatient admin- We evaluated the combination of diphenhydramine, lor- istration of HDC. This approach facilitated early patient azepam, and dexamethasone delivered as a continuous discharge and significantly decreased the total number of i.v. infusion via an ambulatory infusion pump with days of hospitalization associated with BMT. More patient-activated intermittent dosing (BAD pump) for recently, equipped BMT centers have extended the out- prevention of acute and delayed nausea/vomiting in patient care approach to include administration of HDC in patients receiving high-dose chemotherapy (HDC) for the clinic setting. Success of the total outpatient care peripheral blood progenitor cell (PBPC) mobilization approach is dependent upon the availability of experienced (MOB) or prior to autologous PBPC rescue. The BAD staff and necessary resources as well as implementation of pump was titrated to patient response and tolerance, supportive care strategies designed to minimize morbidity and continued until the patient could tolerate oral anti- in the outpatient setting. emetics. Forty-four patients utilized the BAD pump Despite improvements in supportive care strategies, during 66 chemotherapy courses, 34 (52%) for MOB chemotherapy-induced nausea and vomiting continues to be and 32 (48%) for HDC with autologous PBPC rescue. -

Pathophysiology, Differential Diagnosis and Management of Rumination Syndrome Kathleen Blondeau, Veerle Boecxstaens, Nathalie Rommel, Jan Tack
Review article: pathophysiology, differential diagnosis and management of rumination syndrome Kathleen Blondeau, Veerle Boecxstaens, Nathalie Rommel, Jan Tack To cite this version: Kathleen Blondeau, Veerle Boecxstaens, Nathalie Rommel, Jan Tack. Review article: pathophysiol- ogy, differential diagnosis and management of rumination syndrome. Alimentary Pharmacology and Therapeutics, Wiley, 2011, 33 (7), pp.782. 10.1111/j.1365-2036.2011.04584.x. hal-00613928 HAL Id: hal-00613928 https://hal.archives-ouvertes.fr/hal-00613928 Submitted on 8 Aug 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Alimentary Pharmacology & Therapeutic Review article: pathophysiology, differential diagnosis and management of rumination syndrome ForJournal: Alimentary Peer Pharmacology Review & Therapeutics Manuscript ID: APT-1105-2010.R2 Wiley - Manuscript type: Review Article Date Submitted by the 09-Jan-2011 Author: Complete List of Authors: Blondeau, Kathleen; KULeuven, Lab G-I Physiopathology Boecxstaens, Veerle; University of Leuven, Center for Gastroenterological Research Rommel, Nathalie; University of Leuven, Center for Gastroenterological Research Tack, Jan; University Hospital, Center for Gastroenterological Research Functional GI diseases < Disease-based, Oesophagus < Organ- Keywords: based, Diagnostic tests < Topics, Motility < Topics Page 1 of 24 Alimentary Pharmacology & Therapeutic 1 2 3 EDITOR'S COMMENTS TO AUTHOR: 4 Please consider the points raised by the reviewers. -

Akynzeo™ (Netupitant and Palonosetron) Capsule/ Antiemetics
Drug Monograph Drug/Drug Akynzeo™ (netupitant and palonosetron) capsule/ Class: Antiemetics Prepared for: MO HealthNet Prepared by: Xerox Heritage, LLC New Criteria Revision of Existing Criteria Executive Summary The purpose of this monograph is to provide a review of new therapy to determine whether the reviewed drug should be made available on an open Purpose: access basis to prescribers, require a clinical edit or require prior authorization for use. Akynzeo™ is available as a 300 mg/0.5 mg capsule containing 300 mg of netupitant and 0.5 mg of palonosetron respectively. Dosage Forms & Manufacturer: Eisai Inc, Woodcliff Lake, NJ The efficacy of Akynzeo™ for the prevention of acute and delayed nausea and vomiting due to chemotherapy was demonstrated in two phase 3 clinical trials. Complete response rates (ie, no emesis and no rescue medication) for acute, delayed, and overall nausea and vomiting following a single cycle of moderately emetogenic chemotherapy (n=1455) were 88.4%, 76.9%, and 74.3% for Akynzeo™ plus dexamethasone compared Summary of with 85%, 69.5%, and 66.6% for palonosetron plus dexamethasone. In a Findings: second phase 3 study where patients were randomized to receive Akynzeo™ or aprepitant plus palonosetron (with all patients receiving dexamethasone) for repeated cycles of highly or moderately emetogenic chemotherapy (n=412), complete response rates for the overall phase of nausea and vomiting ranged from 81% to 92% for the Akynzeo™ arm and 76% to 88% for the aprepitant/palonosetron arm through 6 cycles of chemotherapy. Status Prior Authorization (PA) Required Open Access Recommendation: Clinical Edit PDL Type of PA Increased Risk of ADE Preferred Agent Criteria: Appropriate Indications Under Solicitation 2015 Xerox Heritage, LLC All Rights Reserved. -

5-HT3 Receptor Antagonists in Neurologic and Neuropsychiatric Disorders: the Iceberg Still Lies Beneath the Surface
1521-0081/71/3/383–412$35.00 https://doi.org/10.1124/pr.118.015487 PHARMACOLOGICAL REVIEWS Pharmacol Rev 71:383–412, July 2019 Copyright © 2019 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: JEFFREY M. WITKIN 5-HT3 Receptor Antagonists in Neurologic and Neuropsychiatric Disorders: The Iceberg Still Lies beneath the Surface Gohar Fakhfouri,1 Reza Rahimian,1 Jonas Dyhrfjeld-Johnsen, Mohammad Reza Zirak, and Jean-Martin Beaulieu Department of Psychiatry and Neuroscience, Faculty of Medicine, CERVO Brain Research Centre, Laval University, Quebec, Quebec, Canada (G.F., R.R.); Sensorion SA, Montpellier, France (J.D.-J.); Department of Pharmacodynamics and Toxicology, School of Pharmacy, Mashhad University of Medical Sciences, Mashhad, Iran (M.R.Z.); and Department of Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada (J.-M.B.) Abstract. ....................................................................................384 I. Introduction. ..............................................................................384 II. 5-HT3 Receptor Structure, Distribution, and Ligands.........................................384 A. 5-HT3 Receptor Agonists .................................................................385 B. 5-HT3 Receptor Antagonists. ............................................................385 Downloaded from 1. 5-HT3 Receptor Competitive Antagonists..............................................385 2. 5-HT3 Receptor -

The Vomiting Center and the Chemoreceptor Trigger Zone
Pharmacologic Control of Vomiting Todd R. Tams, DVM, Dipl. ACVIM VCA West Los Angeles Animal Hospital Pharmacologic Control of Acute Vomiting Initial nonspecific management of vomiting includes NPO (in minor cases a 6-12 hour period of nothing per os may be all that is required), fluid support, and antiemetics. Initial feeding includes small portions of a low fat, single source protein diet starting 6-12 hours after vomiting has ceased. Drugs used to control vomiting will be discussed here. The most effective antiemetics are those that act at both the vomiting center and the chemoreceptor trigger zone. Vomiting is a protective reflex and when it occurs only occasionally treatment is not generally required. However, patients that continue to vomit should be given antiemetics to help reduce fluid loss, pain and discomfort. For many years I strongly favored chlorpromazine (Thorazine), a phenothiazine drug, as the first choice for pharmacologic control of vomiting in most cases. The HT-3 receptor antagonists ondansetron (Zofran) and dolasetron (Anzemet) have also been highly effective antiemetic drugs for a variety of causes of vomiting. Metoclopramide (Reglan) is a reasonably good central antiemetic drug for dogs but not for cats. Maropitant (Cerenia) is a superior broad spectrum antiemetic drug and is now recognized as an excellent first choice for control of vomiting in dogs. Studies and clinical experience have now also shown maropitant to be an effective and safe antiemetic drug for cats. While it is labeled only for dogs, clinical experience has shown it is safe to use the drug in cats as well. Maropitant is also the first choice for prevention of motion sickness vomiting in both dogs and cats. -

Comparative Study of Palonosetron and Ondansetron in Prevention of Post Operative Nausea and Vomiting After Laparoscopic Gynaecological Surgeries
Indian Journal of Clinical Anaesthesia 2020;7(1):59–63 Content available at: iponlinejournal.com Indian Journal of Clinical Anaesthesia Journal homepage: www.innovativepublication.com Original Research Article Comparative study of palonosetron and ondansetron in prevention of post operative nausea and vomiting after laparoscopic gynaecological surgeries Ankita Choudhary1,*, Vinod Parashar1 1Dept. of Anaesthesiology, Santokba Durlabhji Memorial Hospital, Jaipur, Rajasthan, India ARTICLEINFO ABSTRACT Article history: Introduction: Post operative nausea and vomiting (PONV) is a common complication after general Received 13-04-2019 anaesthesia, specially post laparoscopic surgeries. This study compared efficacy of palonosetron with Accepted 20-11-2019 ondansetron for prevention and management of PONV in patients undergoing laparoscopic gynaecological Available online 28-02-2020 surgeries. Materials and Methods : 100 patients, undergoing laparoscopic gynaecological surgery were randomly divided in 2 groups of 50 each. They received either ondansetron(4mg IV) or palonosetron (0.075mg IV) Keywords: before induction of general anaesthesia. They were monitored post operatively till 72 hours for episodes of Palonosetron nausea, vomiting, overall PONV and adverse effects. Post operative nausea vomiting Result: The incidence of overall PONV was significantly less in patients who received palonosetron as Laparoscopic gynaecological compared those who received ondansetron. Also, ondansetron group demonstrated higher use of rescue surgeries anti-emetic drug as compared with palonosetron group. No significant difference was found in incidence Anti-emetic drugs of adverse effects in both groups. Ondansetron Conclusion: Palonosetron, having longer duration of action, is more effective in treating long term PONV compared to ondansetron in patients undergoing laparoscopic gynaecological surgeries under general anesthesia. © 2020 Published by Innovative Publication. -
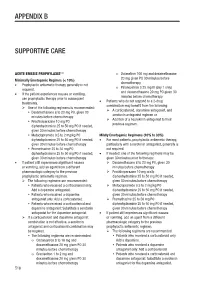
Appendix B Supportive Care
APPENDIX B SUPPORTIVE CARE 1-4 ACUTE EMESIS PROPHYLAXIS o Dolasetron 100 mg and dexamethasone 20 mg given PO 30 minutes before Minimally Emetogenic Regimes (< 10%) chemotherapy • Prophylactic antiemetic therapy generally is not Palonosetron 0.25 mg IV (day 1 only) required. o and dexamethasone 20 mg PO given 30 • If the patient experiences nausea or vomiting, minutes before chemotherapy use prophylactic therapy prior to subsequent Patients who do not respond to a 2-drug treatments. • combination may benefit from the following: One of the following regimens is recommended: A corticosteroid, dopamine antagonist, and Dexamethasone 8 to 20 mg PO, given 30 serotonin antagonist regimen or minutes before chemotherapy Addition of a neurokinin antagonist to their Prochlorperazine 10 mg PO ± previous regimen. diphenhydramine 25 to 50 mg PO if needed, given 30 minutes before chemotherapy Metoclopramide 0.5 to 2 mg/kg PO ± Mildly Emetogenic Regimens (10% to 30%) diphenhydramine 25 to 50 mg PO if needed, • For most patients, prophylactic antiemetic therapy, given 30 minutes before chemotherapy particularly with a serotonin antagonist, generally is Promethazine 25 to 50 mg PO ± not required. diphenhydramine 25 to 50 mg PO if needed, • If needed, one of the following regimens may be given 30 minutes before chemotherapy given 30 minutes prior to therapy: • If patient still experiences significant nausea Dexamethasone 8 to 20 mg PO, given 30 or vomiting, add an agent from a different minutes before chemotherapy pharmacologic category to the previous Prochlorperazine 10 mg orally ± prophylactic antiemetic regimen. diphenhydramine 25 to 50 mg PO if needed, The following regimens are recommended: given 30 minutes before chemotherapy Patients who received a corticosteroid only: Metoclopramide 0.5 to 2 mg/kg PO ± Add a dopamine antagonist. -

Economic Analysis of Palonosetron Versus
Shimizu et al. Journal of Pharmaceutical Health Care and Sciences (2018) 4:31 https://doi.org/10.1186/s40780-018-0128-9 RESEARCHARTICLE Open Access Economic analysis of palonosetron versus granisetron in the standard triplet regimen for preventing chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy in Japan (TRIPLE phase III trial) Hisanori Shimizu1,13* , Kenichi Suzuki2, Takeshi Uchikura1, Daiki Tsuji3, Takeharu Yamanaka4, Hironobu Hashimoto5, Koichi Goto6, Reiko Matsui7, Nobuhiko Seki8, Toshikazu Shimada9, Shunya Ikeda10, Naoki Ikegami11, Toshihiro Hama2, Nobuyuki Yamamoto12 and Tadanori Sasaki1 Abstract Background: We conducted an economic assessment using test data from the phase III TRIPLE study, which examined the efficacy of a 5-hydroxytryptamine 3 receptor antagonist as part of a standard triplet antiemetic regimen including aprepitant and dexamethasone in preventing chemotherapy-induced nausea and vomiting in patients receiving cisplatin-based highly emetogenic chemotherapy (HEC). Methods: We retrospectively investigated all medicines prescribed for antiemetic purposes within 120 h after the initiation of cisplatin administration during hospitalization. In the TRIPLE study, patients were assigned to treatment with granisetron (GRA) 1 mg (n = 413) or palonosetron (PALO) 0.75 mg (n = 414). The evaluation measure was the cost-effectiveness ratio (CER) assessed as the cost per complete response (CR; no vomiting/ retching and no rescue medication). The analysis was conducted from the public healthcare payer’s perspective. Results: The CR rates were 59.1% in the GRA group and 65.7% in the PALO group (P = 0.0539), and the total frequencies of rescue medication use for these groups were 717 (153/413 patients) and 573 (123/414 patients), respectively. -

ASCO's Antiemetics Drug, Dose, and Schedule Table
ASCO 2017 Antiemetics Guideline Update: Drug, Dose, Schedule Recommendations for Antiemetic Regimens Antiemetic Dosing by Chemotherapy Risk Category Agent Dose on Day of Chemotherapy Dose(s) on Subsequent Days High Emetic Risk: Cisplatin and other agents Aprepitant 125 mg oral 80 mg oral; days 2 and 3 Fosaprepitant 150 mg IV NK1 Receptor 300 mg netupitant/0.5 mg palonosetron oral in single Antagonist Netupitant-palonosetron capsule (NEPA) Rolapitant 180 mg oral 2 mg oral or 1 mg or 0.01 mg/kg IV or 1 transdermal Granisetron patch or 10 mg subcutaneous 8 mg oral twice daily or 8 mg oral dissolving tablet Ondansetron twice daily or three 8 mg oral soluble films or 8 mg or 5-HT3 Receptor 0.15 mg/kg IV Antagonista Palonosetron 0.50 mg oral or 0.25 mg IV Dolasetron 100 mg oral ONLY Tropisetron 5 mg oral or 5 mg IV Ramosetron 0.3 mg IV if aprepitant is usedb 12 mg oral or IV 8 mg oral or IV once daily on days 2-4 8 mg oral or IV on day 2; 8 mg oral or IV twice if fosaprepitant is usedb 12 mg oral or IV Dexamethasone daily on days 3-4 if netupitant-palonosetron 12 mg oral or IV 8 mg oral or IV once daily on days 2 to 4 is usedb This table is derived from recommendations in the Antiemetics Guideline Update (2017). This table is a practice tool based on ASCO® practice guidelines and is not intended to substitute for the independent professional judgment of the treating physician.