Respiratory Anatomy and Physiology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Infections of the Respiratory Tract
F70954-07.qxd 12/10/02 7:36 AM Page 71 Infections of the respiratory 7 tract the nasal hairs and by inertial impaction with mucus- 7.1 Pathogenesis 71 covered surfaces in the posterior nasopharynx (Fig. 11). 7.2 Diagnosis 72 The epiglottis, its closure reflex and the cough reflex all reduce the risk of microorganisms reaching the lower 7.3 Management 72 respiratory tract. Particles small enough to reach the tra- 7.4 Diseases and syndromes 73 chea and bronchi stick to the respiratory mucus lining their walls and are propelled towards the oropharynx 7.5 Organisms 79 by the action of cilia (the ‘mucociliary escalator’). Self-assessment: questions 80 Antimicrobial factors present in respiratory secretions further disable inhaled microorganisms. They include Self-assessment: answers 83 lysozyme, lactoferrin and secretory IgA. Particles in the size range 5–10 µm may penetrate further into the lungs and even reach the alveolar air Overview spaces. Here, alveolar macrophages are available to phagocytose potential pathogens, and if these are overwhelmed neutrophils can be recruited via the This chapter deals with infections of structures that constitute inflammatory response. The defences of the respira- the upper and lower respiratory tract. The general population tory tract are a reflection of its vulnerability to micro- commonly experiences upper respiratory tract infections, bial attack. Acquisition of microbial pathogens is which are often seen in general practice. Lower respiratory tract infections are less common but are more likely to cause serious illness and death. Diagnosis and specific chemotherapy of respiratory tract infections present a particular challenge to both the clinician and the laboratory staff. -

Pulmonary Surfactant: the Key to the Evolution of Air Breathing Christopher B
Pulmonary Surfactant: The Key to the Evolution of Air Breathing Christopher B. Daniels and Sandra Orgeig Department of Environmental Biology, University of Adelaide, Adelaide, South Australia 5005, Australia Pulmonary surfactant controls the surface tension at the air-liquid interface within the lung. This sys- tem had a single evolutionary origin that predates the evolution of the vertebrates and lungs. The lipid composition of surfactant has been subjected to evolutionary selection pressures, partic- ularly temperature, throughout the evolution of the vertebrates. ungs have evolved independently on several occasions pendent units, do not necessarily stretch upon inflation but Lover the past 300 million years in association with the radi- unpleat or unfold in a complex manner. Moreover, the many ation and diversification of the vertebrates, such that all major fluid-filled corners and crevices in the alveoli open and close vertebrate groups have members with lungs. However, lungs as the lung inflates and deflates. differ considerably in structure, embryological origin, and Surfactant in nonmammals exhibits an antiadhesive func- function between vertebrate groups. The bronchoalveolar lung tion, lining the interface between apposed epithelial surfaces of mammals is a branching “tree” of tubes leading to millions within regions of a collapsed lung. As the two apposing sur- of tiny respiratory exchange units, termed alveoli. In humans faces peel apart, the lipids rise to the surface of the hypophase there are ~25 branches and 300 million alveoli. This structure fluid at the expanding gas-liquid interface and lower the sur- allows for the generation of an enormous respiratory surface face tension of this fluid, thereby decreasing the work required area (up to 70 m2 in adult humans). -
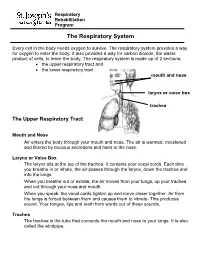
The Respiratory System
Respiratory Rehabilitation Program The Respiratory System Every cell in the body needs oxygen to survive. The respiratory system provides a way for oxygen to enter the body. It also provides a way for carbon dioxide, the waste product of cells, to leave the body. The respiratory system is made up of 2 sections: the upper respiratory tract and the lower respiratory tract mouth and nose larynx or voice box trachea The Upper Respiratory Tract Mouth and Nose Air enters the body through your mouth and nose. The air is warmed, moistened and filtered by mucous secretions and hairs in the nose. Larynx or Voice Box The larynx sits at the top of the trachea. It contains your vocal cords. Each time you breathe in or inhale, the air passes through the larynx, down the trachea and into the lungs. When you breathe out or exhale, the air moves from your lungs, up your trachea and out through your nose and mouth. When you speak, the vocal cords tighten up and move closer together. Air from the lungs is forced between them and causes them to vibrate. This produces sound. Your tongue, lips and teeth form words out of these sounds. Trachea The trachea is the tube that connects the mouth and nose to your lungs. It is also called the windpipe. The Lower Respiratory Tract Inside Lungs Outside Lungs bronchial tubes alveoli diaphragm (muscle) Bronchial Tubes The trachea splits into 2 bronchial tubes in your lungs. These are called the left bronchus and right bronchus. The bronchus tubes keep branching off into smaller and smaller tubes called bronchi. -

RESPIRATORY TRACT INFECTIONS Peter Zajac, DO, FACOFP, Author Amy J
OFP PATIENT EDUCATION HANDOUT RESPIRATORY TRACT INFECTIONS Peter Zajac, DO, FACOFP, Author Amy J. Keenum, DO, PharmD, Editor • Ronald Januchowski, DO, FACOFP, Health Literacy Editor HOME MANAGEMENT INCLUDES: • Drinking plenty of clear fuids and rest. Vitamin-C may help boost your immune system. Over-the-counter pain relievers such as acetaminophen and ibuprofen can be helpful for fevers and to ease any aches. Saline (salt) nose drops, lozenges, and vapor rubs can also help symptoms when used as directed by your physician. • A cool mist humidifer can make breathing easier by thinning mucus. • If you smoke, you should try to stop smoking for good! Avoid second-hand smoking also. • In most cases, antibiotics are not recommended because they are only effective if bacteria caused the infection. • Other treatments, that your Osteopathic Family Physician may prescribe, include Osteopathic Manipulative Therapy (OMT). OMT can help clear mucus, Respiratory tract infections are any relieve congestion, improve breathing and enhance comfort, relaxation, and infection that affect the nose, sinuses, immune function. and throat (i.e. the upper respiratory tract) or airways and lungs (i.e. the • Generally, the symptoms of a respiratory tract infection usually pass within lower respiratory tract). Viruses are one to two weeks. the main cause of the infections, but • To prevent spreading infections, sneeze into the arm of your shirt or in a tissue. bacteria can cause some. You can Also, practice good hygiene such as regularly washing your hands with soap and spread the infection to others through warm water. Wipe down common surfaces, such as door knobs and faucet handles, the air when you sneeze or cough. -

Pulmonary Surfactants and Their Role in Pathophysiology of Lung Disorders
Indian Journal of Experimental Biology Vol. 51, January 2013, pp. 5-22 Review Article Pulmonary surfactants and their role in pathophysiology of lung disorders Aparna Akella & Shripad B Deshpande* Department of Physiology, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221 005, India Surfactant is an agent that decreases the surface tension between two media. The surface tension between gaseous- aqueous interphase in the lungs is decreased by the presence of a thin layer of fluid known as pulmonary surfactant. The pulmonary surfactant is produced by the alveolar type-II (AT-II) cells of the lungs. It is essential for efficient exchange of gases and for maintaining the structural integrity of alveoli. Surfactant is a secretory product, composed of lipids and proteins. Phosphatidylcholine and phosphatidylglycerol are the major lipid constituents and SP-A, SP-B, SP-C, SP-D are four types of surfactant associated proteins. The lipid and protein components are synthesized separately and are packaged into the lamellar bodies in the AT-II cells. Lamellar bodies are the main organelle for the synthesis and metabolism of surfactants. The synthesis, secretion and recycling of the surfactant lipids and proteins is regulated by complex genetic and metabolic mechanisms. The lipid-protein interaction is very important for the structural organization of surfactant monolayer and its functioning. Alterations in surfactant homeostasis or biophysical properties can result in surfactant insufficiency which may be responsible for diseases like respiratory distress syndrome, lung proteinosis, interstitial lung diseases and chronic lung diseases. The biochemical, physiological, developmental and clinical aspects of pulmonary surfactant are presented in this article to understand the pathophysiological mechanisms of these diseases. -

Lipid–Protein and Protein–Protein Interactions in the Pulmonary Surfactant System and Their Role in Lung Homeostasis
International Journal of Molecular Sciences Review Lipid–Protein and Protein–Protein Interactions in the Pulmonary Surfactant System and Their Role in Lung Homeostasis Olga Cañadas 1,2,Bárbara Olmeda 1,2, Alejandro Alonso 1,2 and Jesús Pérez-Gil 1,2,* 1 Departament of Biochemistry and Molecular Biology, Faculty of Biology, Complutense University, 28040 Madrid, Spain; [email protected] (O.C.); [email protected] (B.O.); [email protected] (A.A.) 2 Research Institut “Hospital Doce de Octubre (imasdoce)”, 28040 Madrid, Spain * Correspondence: [email protected]; Tel.: +34-913944994 Received: 9 May 2020; Accepted: 22 May 2020; Published: 25 May 2020 Abstract: Pulmonary surfactant is a lipid/protein complex synthesized by the alveolar epithelium and secreted into the airspaces, where it coats and protects the large respiratory air–liquid interface. Surfactant, assembled as a complex network of membranous structures, integrates elements in charge of reducing surface tension to a minimum along the breathing cycle, thus maintaining a large surface open to gas exchange and also protecting the lung and the body from the entrance of a myriad of potentially pathogenic entities. Different molecules in the surfactant establish a multivalent crosstalk with the epithelium, the immune system and the lung microbiota, constituting a crucial platform to sustain homeostasis, under health and disease. This review summarizes some of the most important molecules and interactions within lung surfactant and how multiple lipid–protein and protein–protein interactions contribute to the proper maintenance of an operative respiratory surface. Keywords: pulmonary surfactant film; surfactant metabolism; surface tension; respiratory air–liquid interface; inflammation; antimicrobial activity; apoptosis; efferocytosis; tissue repair 1. -

Respiratory Tract Infections in the Tropics
9.1 CHAPTER 9 Respiratory Tract Infections in the Tropics Tim J.J. Inglis 9.1 INTRODUCTION Acute respiratory infections are the single most common infective cause of death worldwide. This is also the case in the tropics, where they are a major cause of death in children under five. Bacterial pneumonia is particularly common in children in the tropics, and is more often lethal. Pulmonary tuberculosis is the single most common fatal infection and is more prevalent in many parts of the tropics due to a combination of endemic HIV infection and widespread poverty. A lack of diagnostic tests, limited access to effective treatment and some traditional healing practices exacerbate the impact of respiratory infection in tropical communities. The rapid urbanisation of populations in the tropics has increased the risk of transmitting respiratory pathogens. A combination of poverty and overcrowding in the peri- urban zones of rapidly expanding tropical cities promotes the epidemic spread of acute respiratory infection. PART A. INFECTIONS OF THE LOWER RESPIRATORY TRACT 9.2 PNEUMONIA 9.2.1 Frequency Over four million people die from acute respiratory infection per annum, mostly in developing countries. There is considerable overlap between these respiratory deaths and deaths due to tuberculosis, the single commonest fatal infection. The frequency of acute respiratory infection differs with location due to host, pathogen and environmental factors. Detailed figures are difficult to find and often need to be interpreted carefully, even for tuberculosis where data collection is more consistent. But in urban settings the enormity of respiratory infection is clearly evident. Up to half the patients attending hospital outpatient departments in developing countries have an acute respiratory infection. -

Synthetic Surfactant with a Recombinant Surfactant Protein C Analogue Improves Lung Function and Attenuates Inflammation in a Mo
Zebialowicz Ahlström et al. Respiratory Research (2019) 20:245 https://doi.org/10.1186/s12931-019-1220-x RESEARCH Open Access Synthetic surfactant with a recombinant surfactant protein C analogue improves lung function and attenuates inflammation in a model of acute respiratory distress syndrome in adult rabbits J. Zebialowicz Ahlström1†, F. Massaro2†, P. Mikolka1,3†, R. Feinstein4, G. Perchiazzi5, O. Basabe-Burgos1, T. Curstedt6, A. Larsson5, J. Johansson1 and A. Rising1,7* Abstract Aim: In acute respiratory distress syndrome (ARDS) damaged alveolar epithelium, leakage of plasma proteins into the alveolar space and inactivation of pulmonary surfactant lead to respiratory dysfunction. Lung function could potentially be restored with exogenous surfactant therapy, but clinical trials have so far been disappointing. These negative results may be explained by inactivation and/or too low doses of the administered surfactant. Surfactant based on a recombinant surfactant protein C analogue (rSP-C33Leu) is easy to produce and in this study we compared its effects on lung function and inflammation with a commercial surfactant preparation in an adult rabbit model of ARDS. Methods: ARDS was induced in adult New Zealand rabbits by mild lung-lavages followed by injurious ventilation (VT 20 m/kg body weight) until P/F ratio < 26.7 kPa. The animals were treated with two intratracheal boluses of 2.5 mL/kg of 2% rSP-C33Leu in DPPC/egg PC/POPG, 50:40:10 or poractant alfa (Curosurf®), both surfactants containing 80 mg phospholipids/mL, or air as control. The animals were subsequently ventilated (VT 8–9 m/kg body weight) for an additional 3 h and lung function parameters were recorded. -

PHYSIOLOGY of RESPIRATION Respiration Includes 2 Processes: 1) External Respiration – Is the Uptake of O 2 and Excretion Of
PHYSIOLOGY OF RESPIRATION Respiration includes 2 processes: 1) External respiration – is the uptake of O 2 and excretion of CO 2 in the lungs 2) Internal respiration – means the O 2 and CO 2 exchange between the cells and capillary blood The quality of these respiration processes depends on: a) pulmonary ventilation – it means the inflow and outflow of air between the atmosphere and the lung alveoli b) diffusion of oxygen and CO 2 between the alveoli and the blood c) perfusion – of lungs with blood d) transport of O 2 and CO 2 in the blood e) regulation of respiration Nonrespiratory functions: - in voice production - protective reflexes (apnoea, laryngospasm) - defensive reflexes (cough, sneeze) - in thermoregulation STRUCTURE OF THE RESPIRATORY TRACT Upper airways - nose,nasopharynynx - borderline - larynx Lower airways - trachea, bronchi, bronchioles. The airways divide 23 times to 23 generations between the trachea and: Alveoli - 300 milion - total surface area 70 m 2 lined pneumocytes - type I -flat cells - type II - producers of the surfactant - lymphocytes, plasma cells, alveolar macrophages, mast cells.... Innervation : Smooth muscles innervated by autonomic nervous system: - parasympathetic - muscarinic - bronchoconstriction - sympathetic - beta 2 - receptors – bronchodilation - mainly to adrenalin - noncholinergic nonadrenergic innervation - VIP MECHANICS OF VENTILATION Inspiration - an active process - contraction of the inspiratory muscles: - Diaphragm - accounts for 60-75% of the tidal volume - External intercostal muscles - Auxiliary -accessory-inspiratory muscles: Scalene and sternocleidomasoid m.m. Expiration - quiet breathing - passive process - given by elasticity of the chest and lungs - forced expirium - active process – expiratory muscles: - Internal intercostal m.m. - Muscles of the anterior abdominal wall Innervation: Motoneurons: Diaphragm – n.n. -

Control of Breathing in Mechanically Ventilated Patients
Eur Respir J, 1996, 9, 2151–2160 Copyright ERS Journals Ltd 1996 DOI: 10.1183/09031936.96.09102151 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 SERIES "CLINICAL PHYSIOLOGY IN RESPIRATORY INTENSIVE CARE" Edited by A. Rossi and C. Roussos Control of breathing in mechanically ventilated patients D. Georgopoulos, C. Roussos Control of breathing in mechanically ventilated patients. D. Georgopoulos, C. Roussos. Pulmonary and Critical Care Dept, General ©ERS Journals Ltd 1996. Hospital "G. Papanicolaou", University of ABSTRACT: During mechanical ventilation, the respiratory system is under the Thessaloniki, Thessaloniki, Greece and influence of two pumps, the ventilator pump and the patient's own respiratory Critical Care Dept, "Evangelismos" Hospital, muscles. Depending on the mode of mechanical ventilatory support, ventilation University of Athens, Athens, Greece. may be totally controlled by the ventilator or may be determined by the interac- Correspondence: D. Georgopoulos tion between patient respiratory effort and ventilator function. In either case, com- General Hospital "G. Papanicolaou" pared to spontaneous breathing, the breathing pattern is altered and this may Pulmonary Dept influence: 1) force-length and force-velocity relationships of respiratory muscles Respiratory Failure Unit (mechanical feedback); 2) chemical stimuli (chemical feedback); 3) the activity of Exochi 57010 various receptors located in the respiratory tract, lung and chest wall (reflex feed- Thessaloniki back); and 4) behavioural response (behavioural feedback). Changes in these feed- Greece back systems may modify the function of the ventilator, in a way that is dependent Keywords: Behavioural feedback on the mode of mechanical ventilatory support, ventilator settings, mechanics of chemical feedback the respiratory system and the sleep/awake stage. -

Pulmonary Surfactant: a Front Line of Lung Host Defense
Pulmonary surfactant: a front line of lung host defense Jo Rae Wright J Clin Invest. 2003;111(10):1453-1455. https://doi.org/10.1172/JCI18650. Commentary The lung is a uniquely vulnerable organ. Residing at the interface of the body and the environment, the lung is optimized for gas exchange, having a very thin, delicate epithelium, abundant blood flow, and a vast surface area. Inherent in this structure is an enormous immunological burden from pathogens, allergens, and pollutants resident in the 11,000 liters of air inhaled daily. Fortunately, protective immune mechanisms act locally in the lung to facilitate clearance of inhaled pathogens and to modulate inflammatory responses. These defensive mechanisms include both innate (nonantibody- mediated) and adaptive (antibody-mediated) systems. The purpose of this commentary is to review briefly the functions of one unique lung innate immune system, pulmonary surfactant, and to highlight the recent findings of Wu et al. (1) described in this issue of the JCI. Wu and colleagues report a new and intriguing innate immune function of surfactant: direct antimicrobial activity. Pulmonary surfactant and lung host defense Pulmonary surfactant is a lipoprotein complex that is synthesized and secreted by the alveolar type II epithelial cell and the airway Clara cell into the thin liquid layer that lines the epithelium (reviewed in ref. 2). Once in the extracellular space, surfactant carries out two distinct functions. First, it reduces surface tension at the air-liquid interface of the lung, a function that requires an appropriate mix of surfactant […] Find the latest version: https://jci.me/18650/pdf COMMENTARIES See the related article beginning on page 1589. -

The Pulmonary Surfactant System: Biochemical and Clinical Aspects L
Lung (1997) 175:1–39 © Springer-Verlag New York Inc. 1997 Review The Pulmonary Surfactant System: Biochemical and Clinical Aspects L. A. J. M. Creuwels, L. M. G. van Golde, and H. P. Haagsman Laboratory of Veterinary Biochemistry, Utrecht University, P.O. Box 80176, 3508 TD Utrecht, The Netherlands Abstract. This article starts with a brief account of the history of research on pulmonary surfactant. We will then discuss the morphological aspects and compo- sition of the pulmonary surfactant system. We describe the hydrophilic surfactant proteins A and D and the hydrophobic surfactant proteins B and C, with focus on the crucial roles of these proteins in the dynamics, metabolism, and functions of pulmonary surfactant. Next we discuss the major disorders of the surfactant system. The final part of the review will be focused on the potentials and complications of surfactant therapy in the treatment of some of these disorders. It is our belief that increased knowledge of the surfactant system and its functions will lead to a more optimal composition of the exogenous surfactants and, perhaps, widen their appli- cability to treatment of surfactant disorders other than neonatal respiratory distress syndrome. Key words: Surfactant protein—Pulmonary surfactant—Respiratory distress syn- drome. History Research on surfactant goes back to 1929 when von Neergaard published the first paper about the difference in pressure needed to inflate lungs with air or with liquid [333]. He found that the pressure necessary for filling the lungs with air was higher than when the lungs were filled with liquid. To explain this result he stated that the alveoli were stabilized by lowering the naturally high surface tension of the air/water interface.