A 10-Year Retrospective Review of Botulinum Toxin Injections and Surgical Management of Sialorrhea
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Management of Saliva and Drooling Excessive Saliva and Drooling Affects up to 50% of People with Parkinson’S (PD)
Management of Saliva and Drooling Excessive saliva and drooling affects up to 50% of people with Parkinson’s (PD). Drooling can be embarrassing and can limit social interactions for the person with PD. Saliva and Drooling Parkinson Information Parkinson It can also be an important symptom of swallowing difficulty, which can increase the risk of choking on saliva. People with Parkinson’s disease do not swallow automatically due to rigidity and impaired mobility of the muscles of the palate, throat and esophagus. Saliva pools in the mouth and can potentially become a hazard since swallowing into the lungs carries the risk of pneumonia. If you have poor posture, saliva collects in the front of the mouth, resulting in drooling. Cause and symptoms Decreased control of saliva is most often caused by changes in the ability to swallow, rather than from producing too much saliva. A common cause of drooling for people with PD is the weakening and/or loss of motor control of the muscles involved in swallowing. You may experience one or more of the following symptoms: • Decreased ability to keep your mouth closed at rest, known as the “open mouth posture” • Difficulty keeping lips closed • Lack of awareness of the saliva in your mouth • Wetness at the sides of your mouth • A wet sounding voice • Drooling with posture changes • Coughing and/or choking Evaluation and treatment Speak with your physician about all symptoms that may not be related to PD. If you are experiencing drooling or choking on your saliva, you may require a swallowing evaluation by a Speech Language Pathologist. -

16. Questions and Answers
16. Questions and Answers 1. Which of the following is not associated with esophageal webs? A. Plummer-Vinson syndrome B. Epidermolysis bullosa C. Lupus D. Psoriasis E. Stevens-Johnson syndrome 2. An 11 year old boy complains that occasionally a bite of hotdog “gives mild pressing pain in his chest” and that “it takes a while before he can take another bite.” If it happens again, he discards the hotdog but sometimes he can finish it. The most helpful diagnostic information would come from A. Family history of Schatzki rings B. Eosinophil counts C. UGI D. Time-phased MRI E. Technetium 99 salivagram 3. 12 year old boy previously healthy with one-month history of difficulty swallowing both solid and liquids. He sometimes complains food is getting stuck in his retrosternal area after swallowing. His weight decreased approximately 5% from last year. He denies vomiting, choking, gagging, drooling, pain during swallowing or retrosternal pain. His physical examination is normal. What would be the appropriate next investigation to perform in this patient? A. Upper Endoscopy B. Upper GI contrast study C. Esophageal manometry D. Modified Barium Swallow (MBS) E. Direct laryngoscopy 4. A 12 year old male presents to the ER after a recent episode of emesis. The parents are concerned because undigested food 3 days old was in his vomit. He admits to a sensation of food and liquids “sticking” in his chest for the past 4 months, as he points to the upper middle chest. Parents relate a 10 lb (4.5 Kg) weight loss over the past 3 months. -

Osteoid-Osteoma
Benign tumors of soft tissues and bones of head at children. Classification, etiology. Diagnostics, differential diagnostics, treatment and rehabilitation of children. Pediatric Surgical Dentistry Lector - Kolisnik I.A. 0504044002 (Viber, Telegram) Plan of lecture and their organizational structure. № The main stages of the Type of lecture. Means of time distribution lecture and activating students. Methodical their content support materials 1. Preparatory stage. look p 1 and 2 5 % definitionrelevance of the topic, learning objectives of the lecture and motivation 2. The main stage. Teaching lectureClinical lecture. 85 % material according to the plan: -90% 1. 1 Frequency of malignant processes of SHLD in children. 2. Phases of carcinogenesis 3. Signs of benign and malignant process. 4. Methods of diagnosis of SHLD tumors. 5. The structure of malignant pathology of the thyroid gland in children. 6. Clinical and morphological features of malignant tumors of the thyroid gland in children. Principles of treatment. 7. Basic principles of rehabilitation of children with oncological pathology. 8. Stages of formation of bone regenerate. 9. Clinical case. 1. The final stage Answers to possible 5 % 2. Lecture summary. questions. 3. General conclusions. Classification of benign neoplasm Type of tissue Type of neoplasm Pavement epithelium Squamous cell papilloma Secretory (glandular) epithelium Adenoma Connective Fibroma Adipose Lipoma Smooth muscle Leiomyoma Osseous Osteoma Cartilaginous Chondroma Lymphoid Lymphoma Transversal striated muscle Rhabdomioma -

Oral Pathology Unmasking Gastrointestinal Disease
Journal of Dental Health Oral Disorders & Therapy Review Article Open Access Oral pathology unmasking gastrointestinal disease Abstract Volume 5 Issue 5 - 2016 Different ggastrointestinal disorders, such as Gastroesophageal Reflux Disease (GERD), Celiac Disease (CD) and Crohn’s disease, may manifest with alterations of the oral cavity Fumagalli LA, Gatti H, Armano C, Caruggi S, but are often under and misdiagnosed both by physicians and dentists. GERD can cause Salvatore S dental erosions, which are the main oral manifestation of this disease, or other multiple Department of Pediatric, Università dell’Insubria, Italy affections involving both hard and soft tissues such as burning mouth, aphtous oral ulcers, Correspondence: Silvia Salvatore, Pediatric Department of erythema of soft palate and uvula, stomatitis, epithelial atrophy, increased fibroblast number Pediatric, Università dell’Insubria, Via F. Del Ponte 19, 21100 in chorion, xerostomia and drooling. CD may be responsible of recurrent aphthous stomatitis Varese, Italy, Tel 0039 0332 299247, Fax 0039 0332 235904, (RAS), dental enamel defects, delayed eruption of teeth, atrophic glossitis and angular Email chelitis. Crohn’s disease can occur with several oral manifestations like indurated tag-like lesions, clobbestoning, mucogingivitis or, less specifically, with RAS, angular cheilitis, Received: October 30, 2016 | Published: December 12, 2016 reduced salivation, halitosis, dental caries and periodontal involvement, candidiasis, odynophagia, minor salivary gland enlargement, perioral -

Neurology and the Gastrointestinal System
J Neurol Neurosurg Psychiatry 1998;65:291–300 291 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.65.3.291 on 1 September 1998. Downloaded from NEUROLOGY AND MEDICINE Neurology and the gastrointestinal system G D Perkin, I Murray-Lyon The interrelation of neurology and the gas- that the two techniques are complementary, trointestinal system includes defects of gut acetylcholinesterase staining being particularly innervation, primary disorders of the nervous helpful when the biopsy material does not system (or muscle) which lead to gastrointesti- include submucosa, or in older infants or chil- nal symptoms—for example, dysphagia—and, dren in whom the population of distal submu- finally, certain gut disorders which include cosal ganglion cells may be less dense.6 neurological features in their clinical range. The first of this trio will be discussed only Gastrointestinal disorders due to briefly in this review, the second and third in neurological disease more detail. DYSPHAGIA A neurogenic mechanism for dysphagia, which Defects of innervation may have either sensory or motor components, ACHALASIA or both, can result from a disorder at the oral, Achalasia is characterised by an absence of pharyngeal, or oesophageal phase of swallow- peristalsis in the oesophageal body accompa- ing. In most patients, the neurological disorder nied by a failure of relaxation of the lower is evident, but in others, dysphagia is the oesophageal sphincter.1 Although the condi- presenting feature. Besides the dysphagia, tion can be secondary to other disease other symptoms suggesting a neurogenic copyright. processes—for example, Chagas’ disease—in mechanism include drooling of saliva, nasal Europeans it is usually a primary disorder. -

Oral Complications at the End of Life
CE HOURS Continuing Education1.5 Oral Complications at the End of Life Although dysphagia and stomatitis can have devastating effects on the quality of a patient’s life, there are many ways to manage them. By Constance Dahlin, MSN, APRN, BC, PCM en Eldredge, a 76-year-old retired truck driver, has end-stage heart disease and dementia. In the last year, his health has worsened considerably. He is bedbound, extremely weak, and occasionally short of breath. He has a poor appetite and is losing weight. After an evaluation including a com- plete blood count and computed tomographic scans of the chest and abdomen revealed colon cancer, he received chemotherapy, which ended Ktwo months ago. Mr. Eldredge is being cared for at home by his 75-year- old wife, Jean, and two of their adult children. He complains of dry mouth and says that foods “don’t taste right.” During meals he often coughs and sputters and says his mouth hurts when he eats and that food gets caught in his throat. His wife reports that he often must be coaxed to eat more. Swallowing difficulties (dysphagia) and oral mucosal inflammation (stomatitis) are common in patients who have progressive terminal ill- ness. Perhaps because these conditions are common within the context of a patient’s deconditioning near the end of life, many providers consider them relatively trivial and they’re therefore underreported, underesti- mated, and frequently overlooked for more prominent symptoms such as pain or shortness of breath.1-4 But swallowing difficulties and oral mucosal inflammation can have tremendous adverse consequences for patients and families and should not be dismissed. -

Salivary Gland Disorders and Tumours
Salivary gland disorders and tumours Sumamry This lesson is one we all tend to avoid because most of them sound the same! Hopefully this lesson will help you with clarification. Introduction to Salivary gland disorders and tumours: List of Salivary gland disorders and tumours Viral sialadenitis (mumps) Bacterial sialadenitis Sialosis (sialadenosis) Sialolithiasis Mucocele Acute Necotising Sialometaplasia Tumours: Pleomorphic adenoma Warthins Tumour Mucoepidermoid carcinoma Adenoid cystic carcinoma Acinic cell carcinoma Low-grade polymorphic adenoma Sjogren's syndrome Xerostomia Sialorrhea ReviseDental.com Key words: Sialosis non-pathogenic, non-neoplastic increase in salivary gland size Sialodenitis ductal infection Sialolithiasis duct obstruction Sialectasis cystic widening of the duct Sialorrhea excessive salivation/drooling (1) Acute Viral Sialadenitis Aetiology and epidemiology Common in the childhood disease Mumps caused by the RNA virus Parmyxovirus Typically affects the parotid gland Spread by droplet spread or direct contact 2-3 week incubation period precedes the clinical symptoms Can cause extrasalivary manifestations such as Orchitis Oophoritis Pancreatitis Clinical features Painful Typically bilateral enlargement of parotid glands Skin over the glands is not affected which distinguishes from bacterial sialodenitis Malaise, fever and headaches Histopathology Accumulation of neutrophils and fluid in the lumen of the ductal structures Diagnosis Made on clinical presentation Management FluidsReviseDental.com and medication for -

ODONTOGENTIC INFECTIONS Infection Spread Determinants
ODONTOGENTIC INFECTIONS The Host The Organism The Environment In a state of homeostasis, there is Peter A. Vellis, D.D.S. a balance between the three. PROGRESSION OF ODONTOGENIC Infection Spread Determinants INFECTIONS • Location, location , location 1. Source 2. Bone density 3. Muscle attachment 4. Fascial planes “The Path of Least Resistance” Odontogentic Infections Progression of Odontogenic Infections • Common occurrences • Periapical due primarily to caries • Periodontal and periodontal • Soft tissue involvement disease. – Determined by perforation of the cortical bone in relation to the muscle attachments • Odontogentic infections • Cellulitis‐ acute, painful, diffuse borders can extend to potential • fascial spaces. Abscess‐ chronic, localized pain, fluctuant, well circumscribed. INFECTIONS Severity of the Infection Classic signs and symptoms: • Dolor- Pain Complete Tumor- Swelling History Calor- Warmth – Chief Complaint Rubor- Redness – Onset Loss of function – Duration Trismus – Symptoms Difficulty in breathing, swallowing, chewing Severity of the Infection Physical Examination • Vital Signs • How the patient – Temperature‐ feels‐ Malaise systemic involvement >101 F • Previous treatment – Blood Pressure‐ mild • Self treatment elevation • Past Medical – Pulse‐ >100 History – Increased Respiratory • Review of Systems Rate‐ normal 14‐16 – Lymphadenopathy Fascial Planes/Spaces Fascial Planes/Spaces • Potential spaces for • Primary spaces infectious spread – Canine between loose – Buccal connective tissue – Submandibular – Submental -

Treatments for Ankyloglossia and Ankyloglossia with Concomitant Lip-Tie Comparative Effectiveness Review Number 149
Comparative Effectiveness Review Number 149 Treatments for Ankyloglossia and Ankyloglossia With Concomitant Lip-Tie Comparative Effectiveness Review Number 149 Treatments for Ankyloglossia and Ankyloglossia With Concomitant Lip-Tie Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 290-2012-00009-I Prepared by: Vanderbilt Evidence-based Practice Center Nashville, TN Investigators: David O. Francis, M.D., M.S. Sivakumar Chinnadurai, M.D., M.P.H. Anna Morad, M.D. Richard A. Epstein, Ph.D., M.P.H. Sahar Kohanim, M.D. Shanthi Krishnaswami, M.B.B.S., M.P.H. Nila A. Sathe, M.A., M.L.I.S. Melissa L. McPheeters, Ph.D., M.P.H. AHRQ Publication No. 15-EHC011-EF May 2015 This report is based on research conducted by the Vanderbilt Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 290-2012-00009-I). The findings and conclusions in this document are those of the authors, who are responsible for its contents; the findings and conclusions do not necessarily represent the views of AHRQ. Therefore, no statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help health care decisionmakers—patients and clinicians, health system leaders, and policymakers, among others—make well-informed decisions and thereby improve the quality of health care services. This report is not intended to be a substitute for the application of clinical judgment. -

CDHO Factsheet Oral Cancer
Disease/Medical Condition ORAL CANCER Date of Publication: August 7, 2014 (also known as “oral cavity cancer”) Is the initiation of non-invasive dental hygiene procedures* contra-indicated? Possibly (dental hygiene procedures should not be scheduled while the patient/client is experiencing oral ulcerations and pain, has an acute oral infection, has an absolute neutrophil count ≤ 1.0 X 109/L, or has a platelet count ≤ 50 X 109/L) Is medical consult advised? ..................................... Possibly (e.g., if suspicious lesion is detected; if intraoral infection and/or immunosuppression is suspected, particularly if the patient/client is undergoing radiation therapy and/or chemotherapy) Is the initiation of invasive dental hygiene procedures contra-indicated?** Possibly (contra-indicated for persons undergoing radiotherapy and/or chemotherapy for oral cancer); furthermore, dental hygiene procedures should not be scheduled while the patient/client is experiencing oral ulcerations and pain, has an acute oral infection, has an absolute neutrophil count ≤ 1000/mm3, or has a platelet count ≤ 50,000/mm3) Is medical consult advised? ...................................... See above. Is medical clearance required? .................................. Yes, if the patient/client is about to undergo or is undergoing active chemotherapy or radiation therapy for oral cancer. – Yes, if the patient/client is scheduled for major oral surgery for oral cancer. Is antibiotic prophylaxis required? ............................. No, not typically (although cancer or treatment-induced immunosuppression may warrant consideration of antibiotic prophylaxis). Is postponing treatment advised? .............................. Possibly (depends on whether cancer and its treatment may interfere with invasive procedures and whether there is immunosuppression associated with cancer treatment).1 Oral management implications Dental hygienists play an important role in early detection of oral cancer, leading to timely medical/dental referral and potential biopsy, endoscopy, and imaging. -
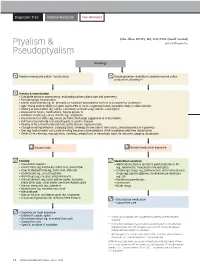
Ptyalism & Pseudoptyalism
Diagnostic Tree Internal Medicine Peer Reviewed Julie Allen, BVMS, MS, DACVIM (Small Animal) Ptyalism & Antech Diagnostics Pseudoptyalism Drooling* Ptyalism (excessive saliva** production) Pseudoptyalism (inability to swallow normal saliva production; drooling**) History & examination • Complete physical examination, evaluating salivary gland size and symmetry • Full neurologic examination • Breed: Giant breeds (eg, St. Bernard) or Yorkshire and Maltese terriers (increased PSS incidence) • Age: Young animals likely to ingest toxins/FBs or have congenital issues; neoplasia likely in older animals • History of vaccination (eg, rabies, calicivirus) or trauma (eg, electric cord injury) • Exposure to toxins, medications, topical products • Duration: Acute (eg, FB) vs chronic (eg, neoplasm) • Discoloration of saliva (eg, blood, purulent discharge) suggestive of oral problem • Halitosis may indicate oral, esophageal, or gastric disease • Pawing at face/mouth may indicate orofacial pain, hypocalcemia • Change in eating behavior: Dropping food, chewing on one side of the mouth, pseudoanorexia or hyporexia • Diet (eg, high-protein) can cause drooling because of precipitation of HE in patients with liver dysfunction • Other GI (ie, retching, regurgitation, vomiting, weight loss) or neurologic signs (ie, seizures, gagging, dysphagia) Known toxin Known medication exposure Toxicity Medication reaction • Household cleaners • Medications/topical products given topically or PO • Plants/trees (eg, Kentucky coffee tree, poinsettia) (eg, selamectin, moxidectin–imidacloprid) -

SIALORRHEA: CHALLENGES and MANAGEMENT Mahima Sehgal1, Dr
ISSN- 2394-5125 VOL 7, ISSUE 19, 2020 SIALORRHEA: CHALLENGES AND MANAGEMENT Mahima Sehgal1, Dr. Suwarna Dangore2, Radha Goverdhan3, Mahwish Nida4 1Intern, Sharad Pawar Dental College & Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (M), Wardha, Maharashtra. India 2Professor, Department of Oral Medicine and Radiology, Sharad Pawar Dental College & Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (M), Wardha, Maharashtra. India 3Intern, Sharad Pawar Dental College & Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (M), Wardha, Maharashtra. India 4Intern, Sharad Pawar Dental College & Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (M), Wardha, Maharashtra. India E-mail : [email protected] Received: 14 April 2020 Revised and Accepted: 8 August 2020 ABSTRACT : In a conscious person, saliva is continuously produced. Saliva not only helps in digestion of food, maintain oral hygiene but also helps in regulating water balance of body. Excessive production of saliva or sialorrhea is a medical and psychosocial problem. It may be due to various dysfunction like sensory, neuromuscular, hypersecretion or even anatomic (motor). Mentally retarded children and those with cerebral palsy are more prone to it. This may lead to social embarrassment, low self-esteem and social alienation in the affected person. Proper assessment and diagnosis is critical in finalizing the treatment plan. A careful diagnosis includes Physical examination, taking family history, observing the neurological co-ordination, searching for evidences of dental problem, any factor contributing to nasal obstruction, observing the severity of drooling. This review article outlines the physiology, etiology, psychosocial effect, evaluation and treatment strategies of sialorrhea.