Safe Motherhood Applied Research and Training (SMART) Report 1: Project Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Muzaffargarh
! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! !! ! ! ! ! ! Overview - Muzaffargarh ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! Bhattiwala Kherawala !Molewala Siwagwala ! Mari PuadhiMari Poadhi LelahLeiah ! ! Chanawala ! ! ! ! ! ! ! Ladhranwala Kherawala! ! ! ! Lerah Tindawala Ahmad Chirawala Bhukwala Jhang Tehsil ! ! ! ! ! ! ! Lalwala ! Pehar MorjhangiMarjhangi Anwarwal!a Khairewala ! ! ! ! ! ! ! ! ! Wali Dadwala MuhammadwalaJindawala Faqirewala ! ! ! ! ! ! ! ! ! MalkaniRetra !Shah Alamwala ! Bhindwalwala ! ! ! ! ! Patti Khar ! ! ! Dargaiwala Shah Alamwala ! ! ! ! ! ! Sultanwala ! ! Zubairwa(24e6)la Vasawa Khiarewala ! ! ! ! ! ! ! Jhok Bodo Mochiwala PakkaMochiwala KumharKumbar ! ! ! ! ! ! Qaziwala ! Haji MuhammadKhanwala Basti Dagi ! ! ! ! ! Lalwala Vasawa ! ! ! Mirani ! ! Munnawala! ! ! Mughlanwala ! Le! gend ! Sohnawala ! ! ! ! ! Pir Shahwala! ! ! Langanwala ! ! ! ! Chaubara ! Rajawala B!asti Saqi ! ! ! ! ! ! ! ! ! BuranawalaBuranawala !Gullanwala ! ! ! ! ! Jahaniawala ! ! ! ! ! Pathanwala Rajawala Maqaliwala Sanpalwala Massu Khanwala ! ! ! ! ! ! Bhandniwal!a Josawala ! ! Basti NasirBabhan Jaman Shah !Tarkhanwala ! !Mohanawala ! ! ! ! ! ! ! ! ! ! Basti Naseer Tarkhanwala Mohanawala !Citiy / Town ! Sohbawala ! Basti Bhedanwala ! ! ! ! ! ! Sohaganwala Bhurliwala ! ! ! ! Thattha BulaniBolani Ladhana Kunnal Thal Pharlawala ! ! ! ! ! ! ! ! ! ! ! Ganjiwala Pinglarwala Sanpal Siddiq Bajwa ! ! ! ! ! Anhiwala Balochanwala ! Pahrewali ! ! Ahmadwala ! ! ! -

Rapid Assessment Report of Flood-Affected Communities in D.G. Khan District, Punjab, Pakistan
Rapid Assessment Report of Flood-Affected Communities in D.G. Khan District, Punjab, Pakistan A house amid flood water in UC Sheroo, Tehsil D.G.Khan Monitoring, Evaluation and Accountability Unit August 19, 2010 Acknowledgements We would like to acknowledge support and cooperation by our field staff members in D.G Khan district particularly Dr. Shafiq-ur-Rehman, Mr. Khurram Khosa and Mr. Sajid. Sincere thanks to our Team Leader, Allison Zelkowitz, who showed keen interest in this assessment and provided every possible support to finish this study in time. We thank our colleague Mr. Omar Aijzi and Mr. Musa Hunzai who provided their valuable inputs during the course of study. We appreciate hard work of our data enumerators who showed great commitment and dedication throughout this exercise. Finally we extend our deepest thanks to flood affected communities who provided us vital information to compile this report. Report by: Sajjad Akram Monitoring, Evaluation & Accountability Manager Muhammad Hassan Monitoring, Evaluation & Accountability Coordinator Save the Children, Malakand Response Program, Pakistan © Photo by Khurram Khusa, a house amid flood water in UC Sheroo, D. G. Khan District, Punjab Province Save the Children Federation Inc. 2010 2 List of Abbreviations and Acronyms BHU Basic Health Unit CD Civil Dispensary CH Civil Hospital D. G. Khan Dera Ghazi Khan DHQ District Headquarter Hospital HHs Households Km Kilometers MNCH Maternal, Neonatal, and Child Health NFIs Non Food Items NGO Non Government Organization SPSS Statistical Package -

Matric Annual 2019
BOARD OF INTERMEDIATE AND SECONDARY EDUCATION DERA GHAZI KHAN 1 SCHOOL WISE PASS PERCENTAGE EXCEPT RESULT LATER ON CASES SECONDARY SCHOOL CERTIFICATE (ANNUAL) EXAMINATION 2019 APPEARED PASSED PASSED% 323201 LOAH-O- QALAM GIRLS SECONDARY SCHOOL KOT ADU M.GARH SCIENCE 23 20 86.96 GENERAL 1 1 100.00 TOTAL 24 21 87.50 32110007 GOVT. GIRLS HIGH SCHOOL, CHOTI ZAREEN (DERA GHAZI KHAN) SCIENCE 176 147 83.52 GENERAL TOTAL 176 147 83.52 32110008 GOVT.GIRLS HIGHER SECONDARY SCHOOL, KOT CHHUTTA (DERA GHAZI KHAN) SCIENCE 217 178 82.03 GENERAL 38 24 63.16 TOTAL 255 202 79.22 32110046 GOVT. GIRLS HIGH SCHOOL, SARWAR WALI (DERA GHAZI KHAN) SCIENCE 81 63 77.78 GENERAL TOTAL 81 63 77.78 32110047 GOVT. GIRLS HIGH SCHOOL, SHADAN LUND (DERA GHAZI KHAN) SCIENCE 96 86 89.58 GENERAL TOTAL 96 86 89.58 32110048 GOVT.GIRLS HIGH SCHOOL, JHOKE UTTRA (DERA GHAZI KHAN) SCIENCE 68 67 98.53 GENERAL TOTAL 68 67 98.53 32110049 GOVT.GIRLS HIGHER SECONDARY SCHOOL, MANA AHMADANI (DERA GHAZI KHAN) SCIENCE 179 177 98.88 GENERAL TOTAL 179 177 98.88 32110050 GOVT. GIRLS HIGH SCHOOL NO.1, DERA GHAZI KHAN SCIENCE 362 320 88.40 GENERAL 140 103 73.57 TOTAL 502 423 84.26 32110051 GOVT.GIRLS HIGH SCHOOL, MULLA QUAID SHAH, DERA GHAZI KHAN SCIENCE 335 277 82.69 GENERAL 39 32 82.05 TOTAL 374 309 82.62 BOARD OF INTERMEDIATE AND SECONDARY EDUCATION DERA GHAZI KHAN 2 SCHOOL WISE PASS PERCENTAGE EXCEPT RESULT LATER ON CASES SECONDARY SCHOOL CERTIFICATE (ANNUAL) EXAMINATION 2019 APPEARED PASSED PASSED% 32110052 CENTER OF EXCELLENCE GOVT. -

(13) Govt. Girls Degree College
BOARD OF INTERMEDIATE & SECONDARY EDUCATION, D.G.KHAN. A1 COLLEGE/INSTITUTE WISE PASS PERCENTAGE INTERMEDIATE (PART-I FRESH) ANNUAL EXAMINATION 2019 NAME OF INSTITUTE FROM RNO TO RNO APPEARED PASSED PASSED % (13) GOVT. GIRLS DEGREE COLLEGE MODEL TOWN, DERA GHAZI KHAN PRE-MEDICAL 297 184 61.95 PRE-ENGINEERING 40 27 67.50 HUMANITIES AND OTHER 132 90 68.18 GENERAL SCIENCE 26 3 11.53 TOTAL: 495 304 61.41 (17) GOVT. GIRLS HIGHER SECONDARY SCHOOL MANA AHMADANI ( DERA GHAZI KHAN ) PRE-MEDICAL 60 43 71.66 PRE-ENGINEERING 18 10 55.55 HUMANITIES AND OTHER 63 47 74.60 GENERAL SCIENCE 7 1 14.28 TOTAL: 148 101 68.24 (49) GOVT. HIGHER SECONDARY SCHOOL MANA AHMADANI ( DERA GHAZI KHAN ) PRE-MEDICAL 69 55 79.71 PRE-ENGINEERING 49 43 87.75 HUMANITIES AND OTHER 69 57 82.60 GENERAL SCIENCE 20 4 20.00 TOTAL: 207 159 76.81 (107) GOVT. GIRLS COMMUNITY HIGHER SECONDARY SCHOOL KHAN GARH ( MUZAFFARGARH ) PRE-MEDICAL 93 62 66.66 PRE-ENGINEERING 16 12 75.00 HUMANITIES AND OTHER 21 13 61.90 GENERAL SCIENCE 18 8 44.44 TOTAL: 148 95 64.18 (111) GOVT.GIRLS COMMUNITY MODEL HIGHER SECONDARY SCHOOL MEHMOOD KOT ( MUZAFFARGARH ) PRE-MEDICAL 85 53 62.35 PRE-ENGINEERING 16 12 75.00 HUMANITIES AND OTHER 37 13 35.13 GENERAL SCIENCE 11 7 63.63 TOTAL: 149 85 57.04 (321101) GOVT. COLLEGE FOR WOMEN CHOTI ZAREEN ( DERA GHAZI KHAN ) PRE-MEDICAL 67 21 31.34 PRE-ENGINEERING 11 9 81.81 BOARD OF INTERMEDIATE & SECONDARY EDUCATION, D.G.KHAN. -

73732 Tendar 25-05-2017.Pdf
HI#-ieg-s.I*ii*tsiJEplT TENDER NOTICE its development projed pertaining District Couocil Dera Ghazi Khan lnteods to call sealed t€nders for D.G.Khan for the financial year 2016-17 . to lop zori-rt {rom coltractors who are enlisted in zla council per bid document by the Head Oerk (l&S 1. The bid documents will be issued on charges of Rs.5OO/- publication of tender notice till to Branch) on written r+quest of contractors from the date of 03-05- 2017 accompanyilrg the followine documents' 2016-2017 from zila council Dera i- Enlistment letler along with Govt Fee deposit slip for financialyear ii. Partnership dLed io case of limited company iii. No Litiga-tion certificate on letter head pad' - the shape of call deposlt from any 2. The sealed bid document alongwith 5/o earnest money in D'6'Khan from date of publication to date 1006 scheduled bank in Punjab in favour of chair;an District Council 2017 at 01:00Pm. at o1:Oo pm in the office of 3, All the received / Sealed bids will be opened on dated 12-0G2017 presence of available contractores or their ir,r,", ao"n",r o.n.*iJn iv arr" ,*a* opening comnittee in the authorized rePresentatives- to quote their rates in Nos as will as in ivords on above 4. lt i5 Eompulsiry on all participated contractors o; below the estimate oin percentage basis' ( amount adiusting 5% of earnest 5. Additional performance guarantee 10% of tender cost balance approved by the competent autiourity within 7 money) should be deposited by the bidder whose rates are wilt be forefeited by the Distrist Ci'uncil .lavs lf he does not dedosit the required amount, his 5% CDR deposited This action cannot be ;;; ;;; ;" ,,]irt r" ,"j""t"0 and process of re-tendering wi, be initiated. -

Pest Situation of Field Crops, Vegetables & Orchards For
PEST SITUATION OF FIELD CROPS, VEGETABLES & ORCHARDS FOR 2ND FORTNIGHT OF JUNE 2019 1 OF 20 Area AFFECTED LOCALITIES/ AREA IN ACRES Affected Area INSECT PEST/ DISTRICT CROPS No. of Spots Surveyed DISEASE No. of Spots (Acre) AREA IN No. of Spots AREA IN (Acre) ABOVE ETL LOCALITIES Above ETL BELOW ETL LOCALITIES ACRES Below ETL ACRES (Hot Spots) Qadir Pur Lar, Mangay Hatti, Sarwar Shah Kot, Balail, Sultan Pur, Jhoke Lashkar Pur, 2/T, Gajju Hatta, Mahra, Veins, Chahan MIranKhan, Vanoi, Jungle Ameer Multan Mango 81 976 707 Galls 30 261 Hussain, Khan Pur Qazian, Hilal Wijhay, Bhana, Jalal Pur Khakhi, Todar Pur, Ponta, Jahan Pur, Behli Sharif, Ghazi Pur, Jang Wala Mango Mango Fruit Borer Baghrain, Bhana 2 52 Mangay Hatti, Sher Shah, Sultan Pur, Veins, Chak RS, Chahan Miran Khan, Mango Fruit Fly 12 119 Vanoi, Jungle Ameer Hussain, Gawain, Khan Pur Qazian, Soman, Todar Pur 5 Faiz, Rukn Abad, Pahore, Jhoke Lashkar Pur, Leli Pur, Gajju Hatta, Mahra, Sikanderabad Gharbi, Chahan Miran Mango Scales Khan, Vanoi, Jungle Ameer Hussain, Khan 22 169 Pur Qazian, Baghrain, Jalal Pur Khakhi, Mirali Wahin, Todar Pur, Ponta, Hafiz Wala 5 Faiz, Qadir Pur Lar, Managay Hatti, Sher Shah, Mirzan Pur, Jhoke Lashkar Pur, Mahra, Vanoi, Jungle Ameer Mango Hopper Hussain, Khan Pur Qazian, Hilal Wijhay, 21 251 Baghrain, Bhana, Jalal Pur Khakhi, Mirali Wahin, Todar Pur, Jahan Pur, Ali Pur Sadat, Nachkain 5 Faiz, Qadir Pur Lar, Jampur, Sher Shah, Buch, Jhoke Lashkar Pur, Gajju Hatta, Mahra, Veins, Sikanderabad Gharbi, Chahan Miran Khan, Vanoi, Jungle Ameer Hussain, Gawain, -
Special Audit Reports - - 5 Performance Audit Reports - - 6 Other Reports (Relating to Uas) -
AUDIT REPORTS ON THE ACCOUNTS OF UNION ADMINISTRATIONS DISTRICT DERA GHAZI KHAN AUDIT YEARS 2009-2012 AUDITOR GENERAL OF PAKISTAN Table of Contents ABBREVIATIONS AND ACRONYMS .................................................... i Preface ....................................................................................... ii EXECUTIVE SUMMARY ........................................................................ iii SUMMARY, TABLES & CHARTS ........................................................ vii Table 1: Audit Work Statistics .................................................................. vii Table 2: Audit Observations Classified by Categories ............................. vii Table 3: Outcome Statistics ...................................................................... viii Table 4: Irregularities Pointed Out ............................................................. ix CHAPTER 1 ....................................................................................... 1 1.1 Union Administrations, District Dera Ghazi Khan .......................... 1 1.1.1 Introduction ....................................................................................... 1 1.1.2 Comments on Budget and Accounts (Variance Analysis) for the Financial Years 2008-11 . 1 1.1.3 Comments on Budget and Accounts (Variance Analysis) ................. 2 AUDIT PARAS ....................................................................................... 5 1.2 Non Production of Record .............................................................. -
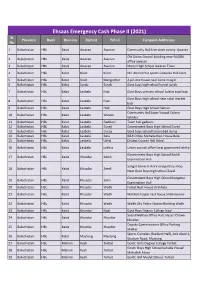
UPDATED CAMPSITES LIST for EECP PHASE-2.Xlsx
Ehsaas Emergency Cash Phase II (2021) Sr. Province Bank Division Distrcit Tehsil Campsite Addresses No. 1 Balochistan HBL Kalat Awaran Awaran Community Hall Live stock colony Awaran Old Union Council building near NADRA 2 Balochistan HBL Kalat Awaran Awaran office awaran 3 Balochistan HBL Kalat Awaran Awaran Model High School Awaran Town 4 Balochistan HBL Kalat Kalat Kalat Mir Ahmed Yar sports Complex Hall kalat 5 Balochistan HBL Kalat Kalat Mangochar A private house near Jame masjid 6 Balochistan HBL Kalat Surab Surab Govt boys high school hostel surab 7 Balochistan HBL Kalat Lasbela Hub Govt Boys primary school Adalat road hub Govt Boys high school near sabzi market 8 Balochistan HBL Kalat Lasbela Hub hub 9 Balochistan HBL Kalat Lasbela Hub Govt Boys High School Sakran Community Hall Jaam Yousuf Colony 10 Balochistan HBL Kalat Lasbela Winder Winder 11 Balochistan HBL Kalat Lasbela Gaddani Town hall gaddani 12 Balochistan HBL Kalat Lasbela Dureji Government Boys High School Dureji 13 Balochistan HBL Kalat Lasbela Dureji Govt boys school hasanabad dureji 14 Balochistan HBL Kalat Lasbela Bela B&R Office Mohalla Rest House Bela 15 Balochistan HBL Kalat Lasbela Uthal District Council Hall Uthal 16 Balochistan HBL Kalat Lasbela Lakhra Union council office local goverment lakhra Government Boys High School Karkh 17 Balochistan HBL Kalat Khuzdar Karkh Examination Hall Sangat General store and poltary shop 18 Balochistan HBL Kalat Khuzdar Zeedi Near Govt Boys high school Zeedi Government Boys High School Norgama 19 Balochistan HBL Kalat Khuzdar Zehri Examination Hall 20 Balochistan HBL Kalat Khuzdar Wadh Forest Rest House Drakhala 21 Balochistan HBL Kalat Khuzdar Wadh Mohbat Faqeer rest house Shahnoorani 22 Balochistan HBL Kalat Khuzdar Wadh Wadh City Police Station Building Wadh 23 Balochistan HBL Kalat Khuzdar Naal Govt Boys Degree College Naal Social Welfare Office Hall, Hazari Chowk 24 Balochistan HBL Kalat Khuzdar Khuzdar khuzdar. -

Ehsaas Emergency Cash Payments
Consolidated List of Campsites and Bank Branches for Ehsaas Emergency Cash Payments Campsites Ehsaas Emergency Cash List of campsites for biometrically enabled payments in all 4 provinces including GB, AJK and Islamabad AZAD JAMMU & KASHMIR SR# District Name Tehsil Campsite 1 Bagh Bagh Boys High School Bagh 2 Bagh Bagh Boys High School Bagh 3 Bagh Bagh Boys inter college Rera Dhulli Bagh 4 Bagh Harighal BISP Tehsil Office Harigal 5 Bagh Dhirkot Boys Degree College Dhirkot 6 Bagh Dhirkot Boys Degree College Dhirkot 7 Hattain Hattian Girls Degree Collage Hattain 8 Hattain Hattian Boys High School Chakothi 9 Hattain Chakar Boys Middle School Chakar 10 Hattain Leepa Girls Degree Collage Leepa (Nakot) 11 Haveli Kahuta Boys Degree Collage Kahutta 12 Haveli Kahuta Boys Degree Collage Kahutta 13 Haveli Khurshidabad Boys Inter Collage Khurshidabad 14 Kotli Kotli Govt. Boys Post Graduate College Kotli 15 Kotli Kotli Inter Science College Gulhar 16 Kotli Kotli Govt. Girls High School No. 02 Kotli 17 Kotli Kotli Boys Pilot High School Kotli 18 Kotli Kotli Govt. Boys Middle School Tatta Pani 19 Kotli Sehnsa Govt. Girls High School Sehnsa 20 Kotli Sehnsa Govt. Boys High School Sehnsa 21 Kotli Fatehpur Thakyala Govt. Boys Degree College Fatehpur Thakyala 22 Kotli Fatehpur Thakyala Local Govt. Office 23 Kotli Charhoi Govt. Boys High School Charhoi 24 Kotli Charhoi Govt. Boys Middle School Gulpur 25 Kotli Charhoi Govt. Boys Higher Secondary School Rajdhani 26 Kotli Charhoi Govt. Boys High School Naar 27 Kotli Khuiratta Govt. Boys High School Khuiratta 28 Kotli Khuiratta Govt. Girls High School Khuiratta 29 Bhimber Bhimber Govt. -

(13) Govt. Girls Degree College
BOARD OF INTERMEDIATE & SECONDARY EDUCATION, D.G.KHAN. COLLEGE/INSTITUTE WISE PASS PERCENTAGE A1 INTERMEDIATE (PART-II & COMBINED) ANNUAL EXAMINATION 2018 NAME OF INSTITUTE FROM RNO TO RNO APPEARED PASSED PASSED % (13) GOVT. GIRLS DEGREE COLLEGE MODEL TOWN, DERA GHAZI KHAN PRE-MEDICAL 245 156 63.67 PRE-ENGINEERING 37 28 75.67 HUMANITIES AND OTHER 124 75 60.48 GENERAL SCIENCE 19 8 42.10 TOTAL: 425 267 62.82 (17) GOVT. GIRLS HIGHER SECONDARY SCHOOL MANA AHMADANI ( DERA GHAZI KHAN ) PRE-MEDICAL 25 19 76.00 PRE-ENGINEERING 13 11 84.61 HUMANITIES AND OTHER 35 31 88.57 TOTAL: 73 61 83.56 (49) GOVT. HIGHER SECONDARY SCHOOL MANA AHMADANI ( DERA GHAZI KHAN ) PRE-MEDICAL 9 8 88.88 PRE-ENGINEERING 17 15 88.23 HUMANITIES AND OTHER 28 19 67.85 GENERAL SCIENCE 7 5 71.42 TOTAL: 61 47 77.04 (107) GOVT. GIRLS COMMUNITY HIGHER SECONDARY SCHOOL KHAN GARH ( MUZAFFARGARH ) PRE-MEDICAL 55 44 80.00 PRE-ENGINEERING 15 11 73.33 HUMANITIES AND OTHER 16 12 75.00 GENERAL SCIENCE 1 0 0.00 TOTAL: 87 67 77.01 (108) GOVT.GIRLS COMMUNITY HIGHER SECONDARY SCHOOL SINAWAN ( MUZAFFARGARH ) PRE-MEDICAL 128 106 82.81 PRE-ENGINEERING 19 9 47.36 HUMANITIES AND OTHER 11 5 45.45 GENERAL SCIENCE 4 1 25.00 TOTAL: 162 121 74.69 (111) GOVT.GIRLS COMMUNITY MODEL HIGHER SECONDARY SCHOOL MEHMOOD KOT ( MUZAFFARGARH ) PRE-MEDICAL 41 33 80.48 PRE-ENGINEERING 15 15 100.00 HUMANITIES AND OTHER 28 21 75.00 GENERAL SCIENCE 5 4 80.00 TOTAL: 89 73 82.02 BOARD OF INTERMEDIATE & SECONDARY EDUCATION, D.G.KHAN. -

To View NSP QAT Schedule
EMIS CODE New QAT Program Sr. No Shift Time SCHOOL NAME Address TEHSIL DISTRICT REGION QAT Day /SCHOOL CODE Date Name 12.30 pm NEW AGE PUBLIC UC Name Dhurnal, UC # 39, Moza FATEH 1 B ATK-FJG-NSP-VIII-3061 ATTOCK North 14 18.12.18 NSP to 2.30 pm SCHOOL Dhurnal, Chak / Basti Dhurnal Ada, JANG Tehsil Fateh Jung District Attock 12.30 pm Village Bai, PO Munnoo Nagar, Tehsil HASSANAB 2 B ATK-HDL-NSP-IV-210 Sun Rise High School ATTOCK North 11 14.12.18 NSP to 2.30 pm Hassan Abdal, District Attock DAL 12.30 pm Science Secondary Thatti Sado Shah, Po Akhlas, Tehsil PINDI 3 B ATK-PGB-NSP-IV-214 ATTOCK North 16 20.12.18 NSP to 2.30 pm School Pindi Gheb, District Attock GHEB 12.30 pm Al Aziz Educational Village Gangawali, Teshil Pindi Gheb, PINDI 4 B ATK-PGB-NSP-IV-216 ATTOCK North 17 09.01.19 NSP to 2.30 pm School System District Attock GHEB Basti Haider town(Pindi Gheb), Mouza 12.30 pm PINDI 5 B ATK-PGB-NSP-VII-2477 Hamza Public School Pindi Gheb, UC Name Chakki, UC # 53, ATTOCK North 17 09.01.19 NSP to 2.30 pm GHEB Tehsil Pindi Gheb, District Attock. Mohallah Jibby. Village Qiblabandi, PO 12.30 pm Tameer-e-Seerat Public 6 B ATK-HZO-NSP-IV-211 Kotkay, Via BaraZai, Tehsil Hazro, HAZRO ATTOCK North 12 15.12.18 NSP to 2.30 pm School District Attock 9.00 am to Stars Public Elementary 7 A ATK-ATK-NSP-IV-207 Dhoke Jawanda, Tehsil & District Attock ATTOCK ATTOCK North 12 15.12.18 NSP 11.00 School 12.30 pm Muslim Scholar Public Dhoke Qureshian, P/O Rangwad, tehsil 8 B ATK-JND-NSP-VI-656 JAND ATTOCK North 15 19.12.18 NSP to 2.30 pm School Jand 12.30 pm Farooqabad -

DERA-GHAZI-KHAN-Rend60.Pdf
Renewal List S/NO REN# / NAME FATHER'S PRESENT ADDRESS DATE OF ACADEMIC REN DATE NAME BIRTH QUALIFICATION 1 39939 ZAFAR PEER BUKHSH CHAK TOPI WALA MOUZA KHAKHI P/O SAMEDISTT. 7-10-1984 MATRIC 13/7/2014 HUSSAIN D.G. KHAN , DERA GHAZI KHAN, PUNJAB 2 37693 ABDUL RASHID ELAHI BAKHSH IDREES TOWN GADAI SHUMALI P/O SAMIN TEH & 1-10-1970 MATRIC 14/7/2014 DISTT. D.G. KHAN , DERA GHAZI KHAN, PUNJAB 3 21707 ABID HUSSAIN KHADIM CHOTI ZARIN BASTI MARI WALAP.O. HASSAN ABAD, 10/5/1978 MATRIC 14/07/2014 HUSSAIN DERA GHAZI KHAN, PUNJAB 4 32701 SAAD ULLAH MUHAMMAD H/NO. 92 BLOCK NO. 15 EID GAH ROAD D, G, KHAN , 26-12- MATRIC 15/07/2014 SAFDAR SAFDAR DERA GHAZI KHAN, PUNJAB 1975 5 47704 GHULAM ALLAH WASAYA VILL, BAQIR WALA P/O NUTKANI TEH, TAUNSA 7-7-1978 MATRIC 19/07/2014 MUSTAFA SHARIF DISTT,, DERA GHAZI KHAN, PUNJAB 6 31539 MUNIR AHMED MOLVI BASHIR MORAH P/O NANKANI TEH, TOUNSAH DISTT, D G 28-5-1973 MATRIC 04/09/2014 AHMED KHAN, DERA GHAZI KHAN, PUNJAB 7 22237 SALEEM MIRZA H.N.82BLOCK G, DERA GHAZI KHAN, PUNJAB 1/4/1974 MATRIC 20/09/2014 AKHTAR MUHAMMAD RAFIQ 8 37680 MUHAMMAD MUHAMMAD HOUSE NO. 92, BLOCK -9, , DERA GHAZI KHAN, 31-8-1968 MATRIC 23/9/2014 SALEEM SHARIF PUNJAB SHARIF 9 40134 MUHAMMAD MUHAMMAD H NO. 102 BLOCK F D G KHAN, DERA GHAZI KHAN, 24-2-1984 MATRIC 27/9/2014 ALI ANSARI RIAZ ANSARI PUNJAB 10 40135 MUHAMMAD MUHAMMAD BLOCK NO.