Curriculum of Mbbs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pak Qatar Panel Hospital List
Pak Qatar Panel Hospital List KARACHI S.No Hospital Name Hospital Address Phone No 1 Advanced Eye Clinic 17 C / 1 Block 6 Pechs Karachi 021-4540999 2 Aga Khan Clifton Medical Center Near Indus Valley School,Sharea Sadee,Clifton Block 2,Street - 11.Karachi 3 Aga Khan Hospital And Medical College Aga Khan University Hospital Stadium Road.Karachi 021-34862478 Foundation (Main) 4 Aga Khan Hospital And Medical College The Aga Hospital For Women Garden,515 Gold Street,Garden 021 34862478 Foundation (Garden) East,Karachi 5 Aga Khan Hospital And Medical College The Aga Khan Hospital For Women,Karimabad,Aisha Manzal,D- 021-36317805 Foundation (Karim) 6,Block 7 Fb Area Karachi 6 Aga Khan Hospital And Medical College The Aga Khan Hospital For Women And 021-32524618 Foundation (Khar) Children,Kharadar,Atmaram Pritamdas Road,Kharadar Karachi. 7 Al Mumtaz Medical Complex 25/423 Darakhshan Society (Kala Board Bus Stop) Malir Karachi 021-45110199 8 Asghar Hospital Sd-23,Block-B,North Nazimabad Karachi 030023456907 9 Ashfaq Memorial Hospital Sb 9, 13 D Main University Road Gulshan Iqbal Karachi 021 34822261 10 Atia General Hospital 48 Malir Township Kalaboard Karachi 021 4501700 11 Boulevard Hospital 140-17 East Street Off Main Korangi Road, Karachi 021-35311691 12 Burhani Hospital Tayyabjee Road Garikhata Karachi 021 2212572 13 Chiniot General Hospital 1/3, Sector 41-B Korangi Township Karachi 021-5063443 14 Clifton Kidney And General Hospital F-17/2,Rojan Street,Block 5,Behind Bar B Q Tonight Clifton, Karachi 021-3837965 15 Creek General Hospital Ibrahim -

11Th and Final Report 7-6-2017.Xlsx
List of Young Scientists (under 40 years of age) Directory of the Productive Scientists of Pakistan 2016 Name/ Designation/ Department/ S.No Sci ID -index ARO Total Organization Score Score Score Score Score Score Score Score Score Score Score (ARO) Books Edited Factor h Published/ Total PhDs Applicant's Applicant's Res. Grants Publications Total Impact 5% 5% 0f Scaled 5% 0f Scaled 5% 0f Scaled 5% 0f Scaled Total Applied Total Patents Total Awards Total Awards Patents score Impact Factor 10% 0f Scaled Total External 30% 0f Scaled 15% 0f Scaled 15% 0f Scaled 10% 0f Scaled Grand Score Total Citations Total Score for Total Score for Total Score for Citations Score Score for Books PhD Supervision Research Grants Research Output F. Health Sciences Shoaib Ahmad Malik (Dr.) Assistant Professor 1 2875 0 0 0.000 0 0 0.00 0 0 0.00 0 0 21 172.3 14.848 0.47 1253 118.001 0.34 15 3.63 0 0 0.00 0 0 0.00 Sargodha Medical College, 0.00 4.44 University of Sargodha, Sargodha Muhammad Arif Lodhi (Dr.) Assistant Professor 2 170 0 0 0.000 0 0 0.00 0 0 0.00 3 7.5 53 63.007 8.792 0.28 514 65.71 0.19 12 2.90 0 0 0.00 0 0 0.00 Department of Biochemistry, 0.07 3.44 Abdul Wali Khan University, Mardan Shah Jahan (Dr.) Assistant Professor 3 119 0 0 0.000 0 0 0.00 0 0 0.00 2 5 22 54.965 9.633 0.31 237 40.1059 0.12 10 2.42 0 0 0.00 0 0 0.00 Department of Immunology, 0.05 2.90 University of Health Sciences, Lahore Sobia Manzoor (Dr.) Assistant Professor 4 Department of Healthcare Biotechnology, 28561 0 0 0.000 0 0 0.00 2 10 0.12 0 0 0.00 28 52.556 8.329 0.26 172 24.808 -

Prevalence and Severity of Depressive Illness Among Youth Coming to Psychiatry Out-Patient Department of District Headquarter Hospital (DHQ), Sargodha
322 Journal of Rawalpindi Medical College (JRMC); 2020; 24(4): 322-327 Original Article Prevalence and severity of Depressive illness among youth coming to Psychiatry Out-patient department of District Headquarter Hospital (DHQ), Sargodha Rida Dawood1, Aftab Nazir2, Muhammad Shahid Javed3, Kashif Rauf4, Zunera Tanveer5, Shoaib Ahmad Malik6 1 Women Medical Officer, Children Hospital & 4 Demonstrator, Department of Biochemistry, Institute of Child Health, Faisalabad. Rawalpindi Medical University, Rawalpindi. 2 Assistant Professor, Department of Community 5 Lecturer, Department of Physiology, Medicine, Independent Medical College, Faisalabad. Bolan University of Medical and Health Sciences, Quetta. 3 Professor, Department of Physiology, 6 Assistant Professor, Department of Biochemistry, Sargodha Medical College, Sargodha. Sargodha Medical College, Sargodha. Author’s Contribution Corresponding Author Article Processing 6 Conception of study Dr. Shoaib Ahmad Malik, Received: 20/03/2020 1,3,6 Experimentation/Study conduction Assistant Professor, Accepted: 20/10/2020 1,2,4,5 Analysis/Interpretation/Discussion Department of Biochemistry, 1,2,6 Manuscript Writing Sargodha Medical College, 3 Facilitation and Material analysis Sargodha Email: [email protected] Cite this Article: Dawood, R., Nazir, A., Javed, M.S., Conflict of Interest: Nil Access Online: Rauf, K., Tanveer, Z., Malik, S.A. Prevalence and Funding Source: Nil severity of Depressive illness among youth coming to Psychiatry Out-patient department of District Headquarter Hospital (DHQ), Sargodha. Journal of Rawalpindi Medical College. 30 Dec. 2020; 24(4): 322- 327. DOI: https://doi.org/10.37939/jrmc.v24i4.1353 Abstract Introduction: Prevalence and severity of depressive illness among the youth are on the rise. Objective: To examine the prevalence and severity of depressive illness among youth coming to the psychiatry outpatient department of District Headquarters Hospital, Sargodha. -

Download FATA Colleges Choices Form
Pre Merit List Merit No. Declaration of Preferences PMC MDCAT Roll No. MBBS/BDS(FATA/MAD SEATS) for Agency/FR. Public Sector Medical Dental Colleges/Institutions Session 2020-21 VERY IMPORTANT: 1.Write your preferences in the order you would like to be considered for admission against the name of College/Institution. 2.Preference once given shall be final and cannot be changed subsequently. Think carefully before writing. 3.Cutting / erasing / over writing is not allowed. 4.The applicant shall never be considered for a college which he/she has not written down in this list of choices. The University shall not assign a college by itself if the alternate choices are not indicated. 5.Khyber Girls Medical College, Peshawar and Fatima Jinnah Medical College, Lahore are for female students only. Male students cannot opt for this college. 6.Candidate who do not submit choices by the deadline i.e. till 02:00 pm on 17/02/2021, the placement committee shall consider his/her choices recorded previously on the already submitted online application form. Name of the Institution/College Choice No. (In Figure and Words) Signatures of the Applicant ADS=Ayub Dental Section, Abbotabad AMC=Ayub Medical College, Abbotabad BKMC=Bacha Khan Medical College, Mardan BKDS=Bacha Khan Dental Secion, Mardan. BMC=Bannu Medical College, Bannu. GKMC = Gajju Khan Medical College Swabi KGMC = Khyber Girls Medical College (For Girls only) GMC = Gomal Medical College KCD = Khyber College of Dentistry KIMS = KMU Institute of Medical Sciences, Kohat KIDS = KMU Institute of Dental Sciences, Kohat KMC = Khyber Medical College Peshawar 1 of 2 Pre Merit List Merit No. -

Health Bulletin July.Pdf
July, 2014 - Volume: 2, Issue: 7 IN THIS BULLETIN HIGHLIGHTS: Polio spread feared over mass displacement 02 English News 2-7 Dengue: Mosquito larva still exists in Pindi 02 Lack of coordination hampering vaccination of NWA children 02 Polio Cases Recorded 8 Delayed security nods affect polio drives in city 02 Combating dengue: Fumigation carried out in rural areas 03 Health Profile: 9-11 U.A.E. polio campaign vaccinates 2.5 million children in 21 areas in Pakistan 03 District Multan Children suffer as Pakistan battles measles epidemic 03 Health dept starts registering IDPs to halt polio spread 04 CDA readies for dengue fever season 05 Maps 12,14,16 Ulema declare polio immunization Islamic 05 Polio virus detected in Quetta linked to Sukkur 05 Articles 13,15 Deaths from vaccine: Health minister suspends 17 officials for negligence 05 Polio vaccinators return to Bara, Pakistan, after five years 06 Urdu News 17-21 Sewage samples polio positive 06 Six children die at a private hospital 06 06 Health Directory 22-35 Another health scare: Two children infected with Rubella virus in Jalozai Camp Norwegian funding for polio eradication increased 07 MULTAN HEALTH FACILITIES ADULT HEALTH AND CARE - PUNJAB MAPS PATIENTS TREATED IN MULTAN DIVISION MULTAN HEALTH FACILITIES 71°26'40"E 71°27'30"E 71°28'20"E 71°29'10"E 71°30'0"E 71°30'50"E BUZDAR CLINIC TAYYABA BISMILLAH JILANI Rd CLINIC AMNA FAMILY il BLOOD CLINIC HOSPITAL Ja d M BANK R FATEH MEDICAL MEDICAL NISHTER DENTAL Legend l D DENTAL & ORAL SURGEON a & DENTAL STORE MEDICAL COLLEGE A RABBANI n COMMUNITY AND HOSPITAL a CLINIC R HOSPITALT C HEALTH GULZAR HOSPITAL u "' Basic Health Unit d g CENTER NAFEES MEDICARE AL MINHAJ FAMILY MULTAN BURN UNIT PSYCHIATRIC h UL QURAN la MATERNITY HOME CLINIC ZAFAR q op Blood Bank N BLOOD BANK r ishta NIAZ CLINIC R i r a Rd X-RAY SIYAL CLINIC d d d SHAHAB k a Saddiqia n R LABORATORY FAROOQ k ÷Ó o Children Hospital d DECENT NISHTAR a . -

Dr. Rafeeq Alam Khan
Rafeeq Alam Khan Curriculum Vitae Meritorious Professor PRESENT STATUS Meritorious Professor Department of Pharmacology Faculty of Pharmacy University of Karachi, Karachi Pakistan Editor in Chief Journal of Basic and Applied Sciences & Journal of Pharmacy and Nutrition Sciences PERSONAL INFORMATION Father's Name Iqbal Alam Khan Date of Birth 09.09.1959 N.I.C. 42101-1807518-9 Marital Status Married Nationality Pakistani E-mail addresses [email protected] , [email protected] Journals website www.lifescienceglobal.com Office Address Department of Pharmacology, Faculty of Pharmacy, University of Karachi, Karachi- 75270 Pakistan Residence B-39, Block-B, Sector 18-A, Gulzar-e-Hijri, Karachi University Employees Co-operative Housing Society, KDA Scheme # 33, Karachi, Pakistan Office Phone +921- 99261300-06 /2361 Cell Number +92-321-8258742 REGISTRATION Registered Pharmacist from Pakistan Pharmacy council Reg. No. 639 dated September 12, 1984. Page 1 of 25 Rafeeq Alam Khan Curriculum Vitae Meritorious Professor EDUCATION Degree Year Specialization/GPA Institute PhD 1996 Pharmacology University of Karachi M. Pharmacy (Gold Medalist) 1986 Pharmacology University of Karachi B. Pharmacy 1983 3.05 University of Karachi REVIEW STATEMENT Twenty nine years of professional, teaching, research and administrative experience had resulted in the creation of a talented team of Pharmacologist not only serving the parent Department, but also enjoying leading positions at various academic institutions throughout Pakistan as well as outside Pakistan. 49 students have been awarded PhD, M. Phil and M. Pharm. degrees under my guidance. I am the editor in chief of two reputable journals. Journal of Basic and Applied Sciences since January 2005, and Journal of Pharmacy and Nutrition Sciences since June 2011, both are now open access journals published by life science global. -

Breast Abcess and Tuberculosis and Its Diagnostic Challenges: a Two-Year Prospective Study in Karachi, Pakistan
Open Access Original Article DOI: 10.7759/cureus.5909 Breast Abcess and Tuberculosis and its Diagnostic Challenges: A Two-Year Prospective Study in Karachi, Pakistan Batool Zehra Asjad 1 , Mir Arsalan Ali 2 , Bushra K. Naeem 3 , Mehmood Khan 1 , Urooj Ahmed Abbasi 4 , Zakia Nehal 5 , Sara Siddiqui 5 1. Surgery, Hamdard University Hospital, Karachi, PAK 2. Surgery, Ziauddin University, Karachi, PAK 3. General Surgery, Jinnah Post Graduate Medical College, Karachi, PAK 4. Surgery, Jinnah Postgraduate Medical Center, Karachi, PAK 5. Surgery, Jinnah Postgraduate Medical Centre, Karachi, PAK Corresponding author: Batool Zehra Asjad, [email protected] Abstract Breast tuberculosis (TB) is rare among extrapulmonary tuberculosis cases, and the diagnosis is usually preceded by a high index of suspicion and findings of granulomatous lesions. We conducted this study to evaluate different clinical presentations of breast TB, including its diagnosis and association with lactation. We also examined the association of breast TB with TB elsewhere in the body and contact history. This prospective, descriptive study was conducted at a tertiary care hospital in Karachi, Pakistan from March 2017 to March 2019. The study population consisted of 100 women of age ranging from 30 to 39 years after 10 patients were lost to follow-up. After providing informed written consent and a histopathology or culture report, participants completed a proforma. We used IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY) to analyze the data, which were kept confidential. Twenty-four patients had diabetes, while 36 patients had no comorbidities. The most consistent symptoms were breast pain (98%), breast lump (89%), fever (83%), and discharge (45%). -

Iqbal Ahmad M
Professor Dr. Iqbal Ahmad M. Sc. (Kar.), Ph. D. (London), D. Sc. Royal Society Fellow Tamgha-e-Imtiaz Department of Pharmaceutical Chemistry Baqai Institute of Pharmaceutical Sciences Baqai Medical University, Karachi ORCID # 0000-0001-8817-3595 POSTAL ADDRESS 51, Deh Tor, Toll Plaza, Super Highway Gadap Road, Karachi-74600. Telephone Off: +92-21-34410293-98 Res: +92-21-34660002 Fax: +92-21-34410439 E-mail: [email protected] [email protected] ACADEMIC QUALIFICATIONS B. Sc. Karachi University 1960 M. Sc. Chemistry Karachi University 1962 Ph. D. Pharmaceutical Chemistry London University 1968 Thesis “A Study of Degradation of Riboflavin and Related Compounds” Postgraduate Diploma Statistics Karachi University 1975 D. Sc. Pharmaceutical Chemistry Karachi University 2014 1 PROFESSIONAL QUALIFICATIONS Registered Pharmacist (Category A) Pharmacy Council of Sind 1976 RESEARCH INTERESTS Drug Analysis, Drug Stability, Preformulation and Formulation Development, Vitamin Interactions in Solution Media, Photochemistry of Medicinal Compounds, Laser Flash Photolysis Studies of Biochemical and Pharmaceutical Systems, Pharmaceutical and Herbal Drug Development. EXPERIENCE POSTDOCTORAL RESEARCH 1. Royal Society Fellow, Department of Biology, Imperial College, London, September 1989–December 1990. Worked with Professor Lord G. Porter, O.M., P.R.S., Nobel Laureate on “Laser Flash Photolysis Studies of Redox Reactions of Photosystem II D1/D2 Cytochrome b 559 Reaction Centres of Higher Plants”. 2. Research Associate, Department of Biochemistry, University of Arizona, Tucson, Arizona 85721, U.S.A., July 1980 - September 1981. Worked with Professor G. Tollin, Regents’ Professor of Biochemistry and Chemistry on “Laser Flash Photolysis Studies of Flavoproteins and Cytochromes”. 3. Postdoctoral Fellow, Research Division, North E. Wales Institute of Higher Education, Connah’s Quay, Clwyd CH5 4BR, U.K., September 1978–June 1980. -
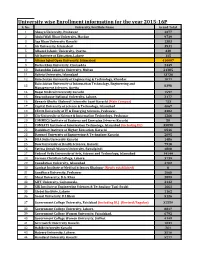
University Wise Enrollment Information for the Year 2015-16P S
University wise Enrollment information for the year 2015-16P S. No. University/Institute Name Grand Total 1 Abasyn University, Peshawar 4377 2 Abdul Wali Khan University, Mardan 9739 3 Aga Khan University Karachi 1383 4 Air University, Islamabad 3531 5 Alhamd Islamic University, Quetta. 338 6 Ali Institute of Education, Lahore 115 8 Allama Iqbal Open University, Islamabad 416607 9 Bacha Khan University, Charsadda 2449 10 Bahauddin Zakariya University, Multan 21385 11 Bahria University, Islamabad 13736 12 Balochistan University of Engineering & Technology, Khuzdar 1071 Balochistan University of Information Technology, Engineering and 13 8398 Management Sciences, Quetta 14 Baqai Medical University Karachi 1597 15 Beaconhouse National University, Lahore. 2177 16 Benazir Bhutto Shaheed University Lyari Karachi (Main Campus) 753 17 Capital University of Science & Technology, Islamabad 4067 18 CECOS University of IT & Emerging Sciences, Peshawar. 3382 19 City University of Science & Information Technology, Peshawar 1266 20 COMMECS Institute of Business and Emerging Sciences Karachi 50 21 COMSATS Institute of Information Technology, Islamabad (including DL) 35890 22 Dadabhoy Institute of Higher Education, Karachi 6546 23 Dawood University of Engineering & Technology Karachi 2095 24 DHA Suffa University Karachi 1486 25 Dow University of Health Sciences, Karachi 7918 26 Fatima Jinnah Women University, Rawalpindi 4808 27 Federal Urdu University of Arts, Science and Technology, Islamabad 14144 28 Forman Christian College, Lahore. 3739 29 Foundation University, Islamabad 4702 30 Gambat Institute of Medical Sciences Khairpur (Newly established) 0 31 Gandhara University, Peshawar 1068 32 Ghazi University, D.G. Khan 2899 33 GIFT University, Gujranwala. 2132 34 GIK Institute of Engineering Sciences & Technology Topi-Swabi 1661 35 Global Institute, Lahore 1162 36 Gomal University, D.I.Khan 5126 37 Government College University, Faislabad (including DL) (Revised/Regular) 32559 38 Government College University, Lahore. -

Sports Directory for Public and Private Universities Public Sector Universities Federal
Sports Directory for Public and Private Universities Public Sector Universities Federal: 1. Allama Iqbal Open University, Islamabad Name of Sports Officer: there is no sports officer in said university as per information received from university. Designation: Office Phone No: Celll No: E-mail: Mailing Address: 2. Bahria University, Islamabad Name of Sports Officer: Malik Bashir Ahmad Designation: Dy. Director Sports Office Phone No: 051-9261279 Cell No: 0331-2221333 E-mail: [email protected] Mailing Address: Bahria University, Naval Complex, E-8, Shangrila Road, Islamabad Name of Sports Officer: Mirza Tasleem Designation: Sports Officer Office Phone No: 051-9261279 Cell No: E-mail: [email protected] Mailing Address: as above 3. International Islamic University, Islamabad Name of Sports Officer: Muhammad Khalid Chaudhry Designation: Sports Officer Office Phone No: 051-9019656 Cell No: 0333-5120533 E-mail: [email protected] Mailing Address: Sports Officer, IIUI, H-12, Islamabad 4. National University of Modern Languages (NUML), Islamabad Name of Sports Officer: No Sports Officer Designation: Office Phone No: 051-9257646 Cell No: E-mail: Mailing Address: Sector H-9, Islamabad Name of Sports Officer: Saeed Ahmed Designation: Demonstrator Office Phone No: 051-9257646 Cell No: 0335-5794434 E-mail: [email protected] Mailing Address: as above 5. Quaid-e-Azam University, Islamabad Name of Sports Officer: M. Safdar Ali Designation: Dy. Director Sports Office Phone No: 051-90642173 Cell No: 0333-6359863 E-mail: [email protected] Mailing Address: Quaid-e-Azam University, Islamabad 6. National University of Sciences and Technology, Islamabad Name of Sports Officer: Mrs. -

Depression Among Medical Students of a Public Sector Medical
Annals of Clinical Obstetrics and Gynecology ISSN: 2694-491X Research Article Depression among Medical Students of a Public Sector Medical University in Pakistan Taimoor Akram Khan1, Hamna Arif2, Saba Sabahat3, Gohar Khan4 and Amjad Khan5* 1Department of Community Medicine, King Edward Medical University, Lahore, Pakistan 2Department of Gynaecology and Obstretics, Lady Aitchison Hospital, Lahore, Pakistan 3Tehsil Head Quarter Hospital, Pakistan 4Department of Medicine, Jinnah Hospital Lahore, Pakistan 5Department of Community Medicine, King Edward Medical University, Lahore, Pakistan Abstract Medical students have several risk factors for depression like lack of sleep, heavy work burden and loads of competition that puts them under enormous pressure. Objective: The objective of this study was to study the burden and severity of depression in medical students and the factors that contribute towards it. Methods: This comparative cross-sectional study was conducted at a public sector medical university in Pakistan in February 2018. Study subjects were selected using stratified random sampling. Burn’s depression checklist, an internationally validated tool for depression, was used for identification of depression and assessment of severity of symptoms. Results: Out of 300 medical students who were included in the study, 124 (41.3%) were males and 176 (58.7%) were females. 61 (20.3%) subjects were from 1st year MBBS, 61 (20.3%) from 2nd year, 65 (21.6%) from 3rd year, 61 (20.3%) from 4th year, and 52 (17.3%) from final year. The ages of subjects were between 17 Years to 26 years with mean age of 22. Out of 300 medical students, 12 students (4%) did not have depression at all, 20 students (6.7%) did not have depression but were unhappy, 102 students (34%) had mild depression whereas 117 students (39%) had moderate depression, 39 students (13%) had severe depression whereas extreme depression was seen in 10 students (3.3%). -

Pak Qatar Panel Hospital List
Pak Qatar Panel Hospital List JAUHARABAD S.No Hospital Name Hospital Address Phone No 1 Al Noor Hospital Jauharabad Civil Line, Jauharabad 0300 3968083 2 Amanat Eye Hospital Lahore Main Boulevard,Near First Women Bank,78-B,E-/1,Gulberg 03355011162 Iii.Lahore ISLAMABAD S.No Hospital Name Hospital Address Phone No 3 Riphah International Hospital Islamabad Express High Way Opposite Dha Gate-7,Islamabad - KARACHI S.No Hospital Name Hospital Address Phone No 4 Advanced Eye Clinic 17 C / 1 Block 6 Pechs Karachi 021-4540999 5 Aga Khan Hospital And Medical College Aga Khan University Hospital Stadium Road.Karachi 021-34862478 Foundation (Main) 6 Aga Khan Hospital And Medical College The Aga Hospital For Women Garden,515 Gold Street,Garden 021 34862478 Foundation (Garden) East,Karachi 7 Aga Khan Hospital And Medical College The Aga Khan Hospital For Women,Karimabad,Aisha Manzal,D- 021-36317805 Foundation (Karim) 6,Block 7 Fb Area Karachi 8 Aga Khan Hospital And Medical College The Aga Khan Hospital For Women And 021-32524618 Foundation (Khar) Children,Kharadar,Atmaram Pritamdas Road,Kharadar Karachi. 9 Al Mumtaz Medical Complex 25/423 Darakhshan Society (Kala Board Bus Stop) Malir Karachi 021-45110199 10 Asghar Hospital Sd-23,Block-B,North Nazimabad Karachi 030023456907 11 Ashfaq Memorial Hospital Sb 9, 13 D Main University Road Gulshan Iqbal Karachi 021 34822261 12 Atia General Hospital 48 Malir Township Kalaboard Karachi 021 4501700 13 Boulevard Hospital 140-17 East Street Off Main Korangi Road, Karachi 021-35311691 14 Burhani Hospital Tayyabjee