Assessment of Contractility for Fontan Connections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Overexpression of Cx43 in Cells of the Myocardial Scar
www.nature.com/scientificreports OPEN Overexpression of Cx43 in cells of the myocardial scar: Correction of post-infarct arrhythmias through Received: 27 September 2017 Accepted: 6 April 2018 heterotypic cell-cell coupling Published: xx xx xxxx Wilhelm Roell1, Alexandra M. Klein1,2, Martin Breitbach2, Torsten S. Becker2, Ashish Parikh4, Jane Lee3, Katrin Zimmermann5, Shaun Reining3, Beth Gabris4, Annika Ottersbach1,2, Robert Doran3, Britta Engelbrecht1,2, Miriam Schifer1,2, Kenichi Kimura1,2, Patricia Freitag2, Esther Carls1,2, Caroline Geisen2, Georg D. Duerr1, Philipp Sasse2, Armin Welz1, Alexander Pfeifer5, Guy Salama4, Michael Kotlikof3 & Bernd K. Fleischmann2 Ventricular tachycardia (VT) is the most common and potentially lethal complication following myocardial infarction (MI). Biological correction of the conduction inhomogeneity that underlies re- entry could be a major advance in infarction therapy. As minimal increases in conduction of infarcted tissue markedly infuence VT susceptibility, we reasoned that enhanced propagation of the electrical signal between non-excitable cells within a resolving infarct might comprise a simple means to decrease post-infarction arrhythmia risk. We therefore tested lentivirus-mediated delivery of the gap-junction protein Connexin 43 (Cx43) into acute myocardial lesions. Cx43 was expressed in (myo)fbroblasts and CD45+ cells within the scar and provided prominent and long lasting arrhythmia protection in vivo. Optical mapping of Cx43 injected hearts revealed enhanced conduction velocity within the scar, indicating Cx43-mediated electrical coupling between myocytes and (myo)fbroblasts. Thus, Cx43 gene therapy, by direct in vivo transduction of non-cardiomyocytes, comprises a simple and clinically applicable biological therapy that markedly reduces post-infarction VT. Ventricular tachycardia (VT) is the most common and potentially lethal complication following myocardial infarction (MI)1. -

Early Diastolic Clicks After the Fontan Procedure for Double
304 Br Heart J 1990;63:304-7 Early diastolic clicks after the Fontan procedure for double inlet left ventricle: anatomical and physiological correlates Br Heart J: first published as 10.1136/hrt.63.5.304 on 1 May 1990. Downloaded from Andrew N Redlngton, Kit-Yee Chan, Julene S Carvalho, Elliot A Shinebourne Abstract inlet ventricle with two atrioventricular M mode echocardiograms and simultan- valves. All had previously undergone a Fontan eous phonocardiograms were recorded type procedure with direct atriopulmonary in four patients with early diastolic anastomosis. In two patients a valved clicks on auscultation. All had double homograft was interposed between the right inlet left ventricle and had undergone atrium and pulmonary artery. Each patient the Fontan procedure with closure of the had the right atrioventricular valve closed by right atrioventricular valve orifice by an either a single or double layer of Dacron cloth artifical patch. The phonocardiogram sewn into the floor of the right atrium. The confirmed a high frequency sound main pulmonary artery was tied off in all. occurring 60-90 ms after aortic valve Cross sectional, M mode, and pulsed wave closure and coinciding with the time of Doppler echocardiograms with simultaneous maximal excursion of the atrioven- electrocardiogram and phonocardiogram were tricular valve patch towards the ven- recorded on a Hewlett-Packard 77020A tricular mass. One patient had coexist- ultrasound system. The phonocardiogram was ing congenital complete heart block. recorded over the point on the chest where the The M mode echocardiogram showed diastolic click was best heart on auscultation, i'reversed") motion of the patch towards usually in the fourth left intercostal space the right atrium during atrial contrac- close to the sternum. -
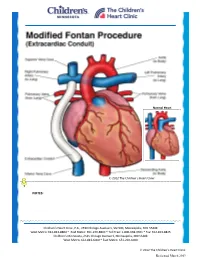
Modified Fontan Procedure: Extracardiac Conduit
Normal Heart © 2012 The Children’s Heart Clinic NOTES: Children’s Heart Clinic, P.A., 2530 Chicago Avenue S, Ste 500, Minneapolis, MN 55404 West Metro: 612-813-8800 * East Metro: 651-220-8800 * Toll Free: 1-800-938-0301 * Fax: 612-813-8825 Children’s Minnesota, 2525 Chicago Avenue S, Minneapolis, MN 55404 West Metro: 612-813-6000 * East Metro: 651-220-6000 © 2012 The Children’s Heart Clinic Reviewed March 2019 Modified Fontan Procedure: Extracardiac Conduit The Fontan procedure is usually the third procedure done in a series of surgeries to complete palliation of single ventricle patients. This procedure separates the “blue,” deoxygenated blood from the “red,” oxygenated blood circuit. Once the Fontan is done, deoxygenated blood drains passively to the pulmonary arteries, then to the lungs. Blood receives oxygen from the lungs and returns to the heart, where it is actively pumped out to the body. This procedure is usually done between 2-4 years of age. During surgery, the chest is opened through the previous incision, using a median sternotomy. The operation may or may not involve the use of cardiopulmonary bypass (heart-lung machine), depending on the surgical plan. A Gore-tex® tube graft (Gore) is cut to the appropriate length. An incision is made on the pulmonary artery near the area of the existing bidirectional Glenn shunt (cavopulmonary anastomosis) and the tube graft is sutured to the artery. Once that is complete, the inferior vena cava is divided from the atrium. The lower end of the Gore-tex® tube graft (Gore) is then sutured to the inferior vena cava. -

The Physiology of the Fontan Circulation ⁎ Andrew Redington
Progress in Pediatric Cardiology 22 (2006) 179–186 www.elsevier.com/locate/ppedcard The physiology of the Fontan circulation ⁎ Andrew Redington Division of Cardiology, The Department of Pediatrics, The Hospital for Sick Children, University of Toronto School of Medicine, Toronto, Ontario, Canada Available online 8 September 2006 Abstract The Fontan circulation, no matter which of its various iterations, is abnormal in virtually every aspect of its performance. Some of these abnormalities are primarily the result of the procedure itself, and others are secondary to the fundamental disturbances of circulatory performance imposed by the ‘single’ ventricle circulation. The physiology of ventricular, systemic arterial and venopulmonary function will be described in this review. © 2006 Elsevier Ireland Ltd. All rights reserved. Keywords: palliation; Fontan circulation; Cavopulmonary anastomosis; Antriopulmonary anastomosis 1. Introduction has the profound consequences for the systemic ventricle that will discussed below. At the same time as the bidirectional In this personal overview, I will discuss the physiology of the cavopulmonary anastomosis was becoming almost uniformly Fontan circulation. Bob Freedom's contribution to our under- adopted, there was abandonment of the ‘classical’ atriopulmon- standing of complex congenital heart disease has meant that ary anastomosis, in favour of the total cavopulmonary con- many more of these patients are surviving with this physiology nection (TCPC). The ‘lateral wall’ TCPC, popularised by Marc than could have been contemplated 30 years ago. Nonetheless, deLeval [1], was shown experimentally and clinically to be they represent a very difficult group of patients and we continue haemodynamically more efficient [1,2] and set the scene for the to learn more about this unique circulation. -

Evaluation of the Optimal Image Reconstruction Interval for Noninvasive Coronary 64-Slice Computed Tomography Venography
Open Journal of Radiology, 2013, 3, 66-72 http://dx.doi.org/10.4236/ojrad.2013.32010 Published Online June 2013 (http://www.scirp.org/journal/ojrad) Evaluation of the Optimal Image Reconstruction Interval for Noninvasive Coronary 64-Slice Computed Tomography Venography Yasutoshi Ohta1, Shinya Fujii1, Suguru Kakite1, Einosuke Mizuta2, Masayuki Hashimoto3, Toshio Kaminou1, Toshihide Ogawa1 1Division of Radiology, Department of Pathophysiological Therapeutic Science, Faculty of Medicine, Tottori University, Yonago City, Japan 2Division of Cardiology, Sanin Rosai Hospital, Yonago City, Japan 3Division of Radiology, Tottori Prefecture Kousei Hospital, Kurayoshi City, Japan Email: [email protected] Received March 22, 2013; revised April 22, 2013; accepted April 30, 2013 Copyright © 2013 Yasutoshi Ohta et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Objective: We investigated the appropriate reconstruction interval required to generate optimal quality images of the coronary veins and to evaluate the size of each vein at the systolic and diastolic phases using coronary computed tomo- graphy (CT) venography. Methods: Coronary CT venograms obtained from 30 patients using 64-slice CT were recon- structed at 0% to 90% of the cardiac cycle in 10% increments. Two radiologists assessed the image quality of the ante- rior interventricular vein (AIV), the great cardiac vein (GCV), the posterior vein of the left ventricle (PVLV), the poste- rior interventricular vein (PIV), the coronary sinus (CS) and the small cardiac vein (SCV). We determined the sizes of measurable CS (n = 16) and GCV (n = 12) at the end systolic and mid diastolic phases. -

Arterial Switch Operation Surgery Surgical Solutions to Complex Problems
Pediatric Cardiovascular Arterial Switch Operation Surgery Surgical Solutions to Complex Problems Tom R. Karl, MS, MD The arterial switch operation is appropriate treatment for most forms of transposition of Andrew Cochrane, FRACS the great arteries. In this review we analyze indications, techniques, and outcome for Christian P.R. Brizard, MD various subsets of patients with transposition of the great arteries, including those with an intact septum beyond 21 days of age, intramural coronary arteries, aortic arch ob- struction, the Taussig-Bing anomaly, discordant (corrected) transposition, transposition of the great arteries with left ventricular outflow tract obstruction, and univentricular hearts with transposition of the great arteries and subaortic stenosis. (Tex Heart Inst J 1997;24:322-33) T ransposition of the great arteries (TGA) is a prototypical lesion for pediat- ric cardiac surgeons, a lethal malformation that can often be converted (with a single operation) to a nearly normal heart. The arterial switch operation (ASO) has evolved to become the treatment of choice for most forms of TGA, and success with this operation has become a standard by which pediatric cardiac surgical units are judged. This is appropriate, because without expertise in neonatal anesthetic management, perfusion, intensive care, cardiology, and surgery, consistently good results are impossible to achieve. Surgical Anatomy of TGA In the broad sense, the term "TGA" describes any heart with a discordant ven- triculoatrial (VA) connection (aorta from right ventricle, pulmonary artery from left ventricle). The anatomic diagnosis is further defined by the intracardiac fea- tures. Most frequently, TGA is used to describe the solitus/concordant/discordant heart. -

Norwood/Batista Operation for a Newborn with Dilated Myopathy of the Left Ventricle
612 Brief communications The Journal of Thoracic and Cardiovascular Surgery September 2000 NORWOOD/BATISTA OPERATION FOR A NEWBORN WITH DILATED MYOPATHY OF THE LEFT VENTRICLE Richard D. Mainwaring, MD, Regina M. Healy, BS, John D. Murphy, MD, and William I. Norwood, MD, PhD, Wilmington, Del Partial left ventriculectomy for dilated cardiomyopathy was contractile function. The variable results that have been first reported by Batista and associates1 in 1996. The rationale reported in the adult literature may reflect patient selection for this procedure is the increase in left ventricular cavity size according to the reversibility or recoverability of the underly- in the absence of compensatory left ventricular wall thickness ing disease process. that is observed in dilated cardiomyopathy. This combination Despite the substantial worldwide experience with the of factors results in an increase in wall stress per unit muscle Batista procedure in adult patients, there is limited experience mass, as predicted by the LaPlace equation. As wall stress with this procedure in children. The current case report increases, mechanical load eventually becomes nonsustain- describes the treatment of a patient in whom the diagnosis of able and contributes to further dilation of the ventricle. Partial dilated cardiomyopathy was made in utero. left ventriculectomy has been advocated as a method of Clinical summary. A female infant was recognized in restoring the balance between cavity size and wall thickness. utero as having a dilated, poorly functioning left ventricle. Fundamental to this concept is the assumption that the left Labor was induced at 36 weeks’ gestation, and she was deliv- ventricular muscle is intrinsically normal or has recoverable ered by normal, spontaneous, vaginal delivery. -

The Clinical Spectrum of Fontan-Associated Liver Disease: Results from a Prospective Multimodality Screening Cohort
Edinburgh Research Explorer The clinical spectrum of Fontan-associated liver disease: results from a prospective multimodality screening cohort Citation for published version: Munsterman, ID, Duijnhouwer, AL, Kendall, TJ, Bronkhorst, CM, Ronot, M, van Wettere, M, van Dijk, APJ, Drenth, JPH & Tjwa, ETTL 2019, 'The clinical spectrum of Fontan-associated liver disease: results from a prospective multimodality screening cohort', European Heart Journal, vol. 40, no. 13, pp. 1057–1068. https://doi.org/10.1093/eurheartj/ehy620 Digital Object Identifier (DOI): 10.1093/eurheartj/ehy620 Link: Link to publication record in Edinburgh Research Explorer Document Version: Peer reviewed version Published In: European Heart Journal General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 25. Sep. 2021 Title: The clinical spectrum of Fontan-Associated Liver Disease: results from a prospective multimodality screening cohort. Authors: I.D. Munsterman1, A.L. Duijnhouwer2, T.J. Kendall3, C.M. Bronkhorst4, M. Ronot5, M. van Wettere5, A.P.J. van Dijk2, J.P.H. Drenth1, E.T.T.L. Tjwa1 On behalf of the Nijmegen Fontan Initiative (A.P.J. -

ICD-10 Coordination and Maintenance Committee Agenda
DEPARTMENT OF HEALTH & HUMAN SERVICES Centers for Medicare & Medicaid Services 7500 Security Boulevard Baltimore, Maryland 21244-1850 Agenda ICD-10 Coordination and Maintenance Committee Department of Health and Human Services Centers for Medicare & Medicaid Services CMS Auditorium 7500 Security Boulevard Baltimore, MD 21244-1850 ICD-10-PCS Topics March 7, 2017 Pat Brooks, CMS – Co -Chairperson Webcast and Dial-In Information The meeting will begin promptly at 9am ET and will be webcast. Toll-free dial-in access is available for participants who cannot join the webcast: Phone: 1-844-396-8222; Meeting ID: 909 233 082. We encourage you to join early, as the number of phone lines is limited. If participating via the webcast or dialing in you do NOT need to register on-line for the meeting. This meeting is being webcast via CMS at http://www.cms.gov/live/. By your attendance, you are giving consent to the use and distribution of your name, likeness and voice during the meeting. You are also giving consent to the use and distribution of any personally identifiable information that you or others may disclose about you during the meeting. Please do not disclose personal health information. Note: Proposals for diagnosis code topics are scheduled for March 8, 2017 and will be led by the Centers for Disease Control (CDC). Please visit CDCs website for the Diagnosis agenda located at the following address: http://www.cdc.gov/nchs/icd/icd9cm_maintenance.htm 1 Introductions and Overview Pat Brooks ICD-10-PCS Topics: 1. Cerebral Embolic Protection During Michelle Joshua Transcatheter Aortic Valve Replacement Alexandra Lansky, MD Pages 10-11 Professor of Medicine, Section of Cardiology Yale School of Medicine 2. -

Brief Communications
View metadata, citation and similar papers at core.ac.uk brought to you byCORE provided by Elsevier - Publisher Connector BRIEF COMMUNICATIONS CARDIOMYOPLASTY COMBINED WITH IMPLANTATION OF A CARDIOVERTER DEFIBRILLATOR Valeri S. Chekanov, MD, PhD, Sanjay Deshpande, MD, and Donald H. Schmidt, MD, Milwaukee, Wis. In the United States alone, approximately 2 to 3 million 58/25 mm Hg and mean 36 mm Hg), elevated pulmonary patients generally are affected by heart failure, and this capillary wedge pressure (an atrial wave of 28 mm Hg, number is likely to increase. 1 Survival of patients with ventricular wave of 42 mm Hg, and mean of 32 mm Hg), advanced ventricular dysfunction is limited not only by and reduced cardiac index (2.12 L/min/m2). Coronary progressive pump dysfunction but also by the risk of angiography showed severe three-vessel coronary artery sudden cardiac death. The 1-year mortality risk exceeds disease. The left ventricle was severely hypocontractile, 50% for patients with class IV symptoms. 2 Dynamic with an ejection fraction of 10%. cardiomyoplasty is emerging as a promising form of Latissimus dorsi cardiomyoplasty was chosen instead of surgical therapy for patients with advanced ventricular heart transplantation because the patient did not have dysfunction, but sudden cardiac death remains a major end-stage heart failure. Cardiomyoplasty was performed factor in decreased long-term survival among patients who through a medial sternotomy and a posterior wrap was have undergone cardiomyoplasty.3 Among the various performed. A Medtronic cardiostimulator (Medtronic, available therapeutic strategies for patients at high risk for Inc., Minneapolis, Minn.) was implanted with the myocar- sudden cardiac death, the implantable cardioverter defi- dial and skeletal electrodes placed in the conventional brillator (ICD) has been shown to be effective. -

Pressure-Volume Measurements By
PRESSURE-VOLUME MEASUREMENTS BY CONDUCTANCE CATHETER METHOD IN THORACIC SURGERY AND INTENSIVE CARE STUDIES CD Leycom Argonstraat 116 2718 SP Zoetermeer The Netherlands Tel: (31) 79 360 1780 Fax: (31) 79 362 1743 Email: [email protected] Website: www.cdleycom.com Version 0035.0 Ref.: CC-SURG.REV.V0035 1. CARDIOMYOPLASTY and AORTOMYOPLASTY In cardiomyoplasty dilated cardiomyopathy is treated by surgically wrapping the right latissimus muscle around the heart.The purpose of this is to stimulate the muscle, after having been conditioned for several months, in order to assist the ventricle in ejection during selected heart beats. The clinical success of this method is still debated. One of the important issues is how to evaluate the effects of the procedure in terms of improved pump function of the left ventricle. One of the most useful (or even the only) ways of assessing changed hemodynamics and contractile performance is the registration of left ventricular pressure- volume loops. Such loops may be constructed on a continuous basis during preload reduction (by transient vena cava occlusion) using the conductance catheter as has been done in several animal studies (1, 2, 3, 4). The general conclusion of these studies was that the proper stimulation protocol of the wrapped muscle effectuated an increase in contractility expressed by a leftward displacement and/or steeper slope of the end-systolic pressure-volume relation (ESPVR). A similar analysis, applied in human patients after undergoing cardiomyoplasty, has been published recently (5). Although no load reduction was performed in this multi- clinical study, it was shown convincingly that a stimulated heart beat when compared to unstimulated beats, resulted in an increased stroke volume mainly effectuated through a decrease in end-systolic volume, provided an optimal stimulation setting was utilized. -

Biointerventional Cardiovascular Therapy
European Heart Journal (2002) 23, 1753–1756 doi:10.1053/euhj.2002.3321, available online at http://www.idealibrary.com on Review Article Biointerventional cardiovascular therapy I. D. Cox, C. A. Thompson and S. N. Oesterle Cardiology Division, Massachusetts General Hospital, Boston, Massachusetts, U.S.A. Introduction However, viral vectors (such as adeno- and retroviruses) are generally considered to provide superior gene trans- Recent advances in gene and cell based therapies have fer efficiency in terms of both magnitude and duration of created exciting possibilities for therapeutic modification gene expression[4]. Non-selective delivery of adenoviral of local vascular and myocardial biology. The parallel vectors, either by intracoronary injection[5] or pressure- evolution of increasingly sophisticated catheter-based regulated retroinfusion via the coronary veins[6], can systems is currently expanding the frontiers of percu- result in diffuse distribution throughout the myocar- taneous intervention in cardiovascular disease[1,2] and dium. More selective gene transfer can be achieved by offers the possibility of delivering gene and cell based direct injection of genetic material into myocardium[7]. therapies by minimally invasive means. This conver- The latter approach achieves higher local tissue con- gence of biotechnology and advanced catheter based centration of therapeutic substrate and thereby seems systems can sensibly be referred to as bio-interventional likely to prove more efficient and less liable to produce cardiovascular therapy and rapid progress is currently undesirable effects in other vascular beds. In most cases, being made in a number of areas within this field. selective local injection of genetic substrate has been achieved through open surgical access to the myocar- dium.