Local Anesthesia Techniques of the Digits, Hallux, by Khurram H
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Pricing Sheet
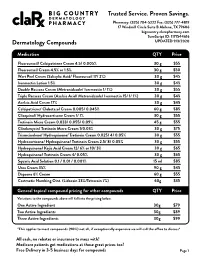
Trusted Service. Proven Savings. Pharmacy: (325) 704-5222 Fax: (325) 777-4819 17 Windmill Circle Suite B Abilene, TX 79606 bigcountry.clarxpharmacy.com SureScript ID: 1171544616 Dermatology Compounds UPDATED 9/3/2020 Medication QTY Price Fluorouracil/ Calcipotriene Cream 4.5/ 0.005% 30 g $55 Fluorouracil Cream 4.5% or 1.5% 30 g $50 Wart Peel Cream (Salicylic Acid/ Fluorouracil 17/ 2%) 30 g $45 Ivermectin Lotion 1.5% 30 g $45 Double Rosacea Cream (Metronidazole/ Ivermectin 1/ 1%) 30 g $55 Triple Rosacea Cream (Azelaic Acid/ Metronidazole/ Ivermectin 15/ 1/ 1%) 30 g $45 Azelaic Acid Cream 17% 30 g $45 Calcipotriene/ Clobetasol Cream 0.005/ 0.045% 60 g $85 Clioquinol/ Hydrocortisone Cream 1/ 1% 30 g $55 Tretinoin Micro Cream 0.033/ 0.055/ 0.09% 45 g $55 Clindamycin/ Tretinoin Micro Cream 1/0.03% 30 g $75 Triamcinolone/ Hydroquinone/ Tretinoin Cream 0.025/ 4/ 0.05% 30 g $55 Hydrocortisone/ Hydroquinone/ Tretinoin Cream 2.5/ 8/ 0.05% 30 g $55 Hydroquinone/ Kojic Acid Cream 12/ 6% or 10/ 3% 30 g $65 Hydroquinone/ Tretinoin Cream 4/ 0.05% 30 g $65 Squaric Acid Solution 0.1 / 0.01 / 0.001% 15 ml $85 Urea Cream 35% 90 g $45 Dapsone 6% Cream 60 g $55 Costmetic Numbing Oint. (Lidocain 23%/Tetracain 7%) 60g $35 General topical compound pricing for other compounds QTY Price Variations to the compounds above will fall into the pricing below. One Active Ingredient 30g $79 Two Active Ingredients 30g $89 Three Active Ingredients 30g $99 *This applies to most compounds (90%) not all, if exceptionally expensive we will call the office to discuss* All cash, no rebates or insurance to mess with! Medicare patients get medications at these great prices too! Free Delivery in 3-5 business days for compounds Page 1 Trusted Service. -

Cream LOTRISONE® Lotion (Clotrimazole and Betamethasone Dipropionate)
LOTRISONE® Cream LOTRISONE® Lotion (clotrimazole and betamethasone dipropionate) FOR TOPICAL USE ONLY. NOT FOR OPHTHALMIC, ORAL, OR INTRAVAGINAL USE. NOT RECOMMENDED FOR PATIENTS UNDER THE AGE OF 17 YEARS AND NOT RECOMMENDED FOR DIAPER DERMATITIS. DESCRIPTION LOTRISONE® Cream and Lotion contain combinations of clotrimazole, a synthetic antifungal agent, and betamethasone dipropionate, a synthetic corticosteroid, for dermatologic use. Chemically, clotrimazole is 1–(o-chloro-α,α-diphenylbenzyl) imidazole, with the empirical formula C22H17CIN2, a molecular weight of 344.84, and the following structural formula: Clotrimazole is an odorless, white crystalline powder, insoluble in water and soluble in ethanol. Betamethasone dipropionate has the chemical name 9-fluoro-11β,17,21- trihydroxy-16β-methylpregna-1,4-diene-3,20-dione 17,21-dipropionate, with the empirical formula C28H37FO7, a molecular weight of 504.59, and the following structural formula: 1 LRN# 000370-LOS-MTL-USPI-1 Betamethasone dipropionate is a white to creamy white, odorless crystalline powder, insoluble in water. Each gram of LOTRISONE Cream contains 10 mg clotrimazole and 0.643 mg betamethasone dipropionate (equivalent to 0.5 mg betamethasone), in a hydrophilic cream consisting of purified water, mineral oil, white petrolatum, cetyl alcohol plus stearyl alcohol, ceteareth-30, propylene glycol, sodium phosphate monobasic monohydrate, and phosphoric acid; benzyl alcohol as preservative. LOTRISONE Cream may contain sodium hydroxide. LOTRISONE Cream is smooth, uniform, and white to off-white in color. Each gram of LOTRISONE Lotion contains 10 mg clotrimazole and 0.643 mg betamethasone dipropionate (equivalent to 0.5 mg betamethasone), in a hydrophilic base of purified water, mineral oil, white petrolatum, cetyl alcohol plus stearyl alcohol, ceteareth-30, propylene glycol, sodium phosphate monobasic monohydrate, and phosphoric acid; benzyl alcohol as a preservative. -

Salicylic Acid
Treatment Guide to Common Skin Conditions Prepared by Loren Regier, BSP, BA, Sharon Downey -www.RxFiles.ca Revised: Jan 2004 Dermatitis, Atopic Dry Skin Psoriasis Step 1 - General Treatment Measures Step 1 - General Treatment Measures Step 1 • Avoid contact with irritants or trigger factors • Use cool air humidifiers • Non-pharmacologic measures (general health issues) • Avoid wool or nylon clothing. • Lower house temperature (minimize perspiration) • Moisturizers (will not clear skin, but will ↓ itching) • Wash clothing in soap vs detergent; double rinse/vinegar • Limit use of soap to axillae, feet, and groin • Avoid frequent or prolonged bathing; twice weekly • Topical Steroids Step 2 recommended but daily bathing permitted with • Coal Tar • Colloidal oatmeal bath products adequate skin hydration therapy (apply moisturizer • Anthralin • Lanolin-free water miscible bath oil immediately afterwards) • Vitamin D3 • Intensive skin hydration therapy • Limit use of soap to axillae, feet, and groin • Topical Retinoid Therapy • “Soapless” cleansers for sensitive skin • Apply lubricating emollients such as petrolatum to • Sunshine Step 3 damp skin (e.g. after bathing) • Oral antihistamines (1st generation)for sedation & relief of • Salicylic acid itching give at bedtime +/- a daytime regimen as required Step 2 • Bath additives (tar solns, oils, oatmeal, Epsom salts) • Topical hydrocortisone (0.5%) for inflammation • Colloidal oatmeal bath products Step 2 apply od-tid; ointments more effective than creams • Water miscible bath oil • Phototherapy (UVB) may use cream during day & ointment at night • Humectants: urea, lactic acid, phospholipid • Photochemotherapy (Psoralen + UVA) Step 4 Step 3 • Combination Therapies (from Step 1 & 2 treatments) • Prescription topical corticosteroids: use lowest potency • Oral antihistamines for sedation & relief of itching steroid that is effective and wean to twice weekly. -

(6337) Smartpharmacy.Com
Phone 1.877.811.MEDS (6337) Fax 800.910.7195 SmartPharmacy.com Your prescription has been faxed to SMART PHARMACY Fax: (800) 910-7195 Phone: (877) 811-MEDS (6337) ** SHIPPING IS ALWAYS FREE Your physician has prescribed a topical cream to treat your pain and inflammation. Please review the following information about your prescription. HOW DO I FILL MY PRESCRIPTION? HOW DO I APPLY THE CREAM? • In most cases, your physician’s office will fax your The proper application of the cream is imperative to achieve prescription directly to Smart Pharmacy. A Smart Pharmacy maximum results; therefore, be sure to follow directions on the Registered Pharmacy Technician will begin processing your prescription label. prescription and contact you by phone. • Your prescription will arrive in an easy-to-use pump applicator. • Please leave a good contact number for calling or texting in order to expedite your order. • Clean and dry the affected area prior to applying topical cream with each application. • With your approval, the prescription will be shipped directly to your home or business at no charge. • Use latex gloves or thoroughly wash hands before and after each application. Do not apply to open wounds. Do not touch eyes or WILL INSURANCE COVER MY SMART mouth before washing hands as you may cause burning and irritation. PHARMACY PRESCRIPTION? • Most commercial insurance plans cover topical preparations with a reasonable co-pay. • Apply a liberal amount to affected area and rub in well as directed by your physician, massaging the affected area for 1-2 minutes. • Smart Pharmacy will verify your coverage and discuss your co-pay obligation. -

Drugs That Are Not Covered
Drugs that are Not Covered* Current 10/1/21 In addition to this list, newly marketed prescription medications may not be covered until the Pharmacy & Therapeutics Committee has had an opportunity to review the medication, to determine whether the medication will be covered and if so, which tier will apply based on safety, efficacy and the availability of other products within that class of medications. The current list of newly marketed drugs can be found on our New to Market Drug list. Abilify tablets albuterol HFA inhalers (authorized Apexicon E cream Abilify MyCite tablets generics for ProAir, Proventil, Ventolin Apidra vials Absorica capsules HFA inhalers) Apidra SoloStar injection Absorica LD capsules Aldactone tablets Aplenzin tablets Abstral sublingual tablets Aldara cream Apriso capsules Acanya gel and pump gel Alkindi sprinkle capsules Arava tablets Accupril tablets Allegra Children’s Allergy ODT Arazlo lotion acetaminophen 320.5 mg/caffeine 30 Allegra ODT, suspension and tablets Arestin microspheres mg/dihydrocodeine 16 mg Alltizal tablets Aricept tablets capsulesAciphex tablets alogliptin (authorized generic for Aricept ODT Aciphex Sprinkle capsules Nesina) Arimidex tablets Acticlate tablets alogliptin/metformin tablets (authorized Arixtra injection Active-Prep kits generic for Kazano) ArmonAir Digihaler inhaler Activella tablets alogliptin/pioglitazone (authorized ArmonAir Respiclick inhaler Actonel tablets generic for Oseni) Aromasin tablets Actoplus Met tablets Alphagan P 0.1% eye drops Arthrotec 50 and 75 tablets Actos -

Important Pharmacy Information There Is No Copay When Your Primary Care Provider (PCP) Or Unitedhealthcare Community Plan Specialist Writes You a Covered Prescription
Important Pharmacy Information There is no copay when your Primary Care Provider (PCP) or UnitedHealthcare Community Plan Specialist writes you a covered prescription. But you can get many over-the-counter (OTC) medicines free when you have a prescription. You can get the medications listed on the following pages when they are medically necessary and you get a written prescription from your UnitedHealthcare Community Plan doctor and take it to a UnitedHealthcare Community Plan pharmacy. To get your medicine: • Take your prescription to a UnitedHealthcare Community Plan pharmacy. To find a pharmacy, call 1-800-903-5253 or go to UHCCommunityPlan.com. • For your safety, we urge you to select a single pharmacy from which to get your drugs. • Get to know the pharmacist and build a relationship. If the UnitedHealthcare Community Plan pharmacy says they cannot fill your covered prescription or you have to pay more than your copay: Do not leave the pharmacy. Do not pay for it yourself. Ask the pharmacy why they cannot fill your prescription. Response Your Solution Not Covered • Ask them to call OptumRx right away to find out which medicine is covered. • Ask them to call your doctor to see if you can get the covered medicine instead. Prior • Ask them to call your doctor for a prior authorization. Authorization • You can call your doctor and ask that a prior authorization be sent to: Needed UnitedHealthcare Pharmacy Prior Notification Service Fax 1-866-940-7328 Phone 1-800-310-6826 Refill Too Soon • Ask what day it can be filled. • Pick your prescription up the day it can be filled. -

Transdermal and Topical Drug Administration in the Treatment of Pain
molecules Review Transdermal and Topical Drug Administration in the Treatment of Pain Wojciech Leppert 1,*, Malgorzata Malec–Milewska 2, Renata Zajaczkowska 3,4 and Jerzy Wordliczek 3,4 1 Department of Palliative Medicine, Poznan University of Medical Sciences, Osiedle Rusa 55, 61–645 Poznan, Poland 2 Department of Anesthesiology and Intensive Care, Medical Centre of Postgraduate Education, 01-813 Warsaw, Poland; [email protected] 3 Department of Interdisciplinary Intensive Care, Jagiellonian University Medical College, 31-008 Krakow, Poland; [email protected] (R.Z.); [email protected] (J.W.) 4 Department of Anesthesiology and Intensive Therapy, University Hospital, 31-501 Krakow, Poland * Correspondence: [email protected]; Tel.: +48-61-8738-303 Academic Editor: Silvia Schenone Received: 30 January 2018; Accepted: 13 March 2018; Published: 17 March 2018 Abstract: The comprehensive treatment of pain is multidimodal, with pharmacotherapy playing a key role. An effective therapy for pain depends on the intensity and type of pain, the patients’ age, comorbidities, and appropriate choice of analgesic, its dose and route of administration. This review is aimed at presenting current knowledge on analgesics administered by transdermal and topical routes for physicians, nurses, pharmacists, and other health care professionals dealing with patients suffering from pain. Analgesics administered transdermally or topically act through different mechanisms. Opioids administered transdermally are absorbed into vessels located in subcutaneous tissue and, subsequently, are conveyed in the blood to opioid receptors localized in the central and peripheral nervous system. Non–steroidal anti–inflammatory drugs (NSAIDs) applied topically render analgesia mainly through a high concentration in the structures of the joint and a provision of local anti–inflammatory effects. -

PRODUCTS Physicians and Scientists Dedicated to Eczema Patients and Research
National Eczema Association The National Eczema Association (NEA) improves the health and quality of life for individuals with eczema through research, support, and education. NEA is governed by a Board of Directors and guided by a Scientific Advisory Committee comprised of PRODUCTS physicians and scientists dedicated to eczema patients and research. For a complimentary copy of the NEA quarterly magazine, The Advocate, and an eczema information package, please contact us. We are always here to help! National Eczema Association 4460 Redwood Highway, Suite 16D, San Rafael, CA 94903-1953 nationaleczema.org [email protected] TELEPHONE 415.499.3474 TOLL FREE 800.818.SKIN FAX 415.472.5345 JOIN NEA ON FACEBOOK: facebook.nationaleczema.org JOIN NEA’S ONLINE SUPPORT FORUM: National Eczema Association forum.nationaleczema.org Seal of Acceptance™ Program To help improve the quality of life for people with eczema and sensitive skin, the National Eczema As- sociation established the Seal of Acceptance program. If you or someone you care for suffers from eczema or sensitive skin, it can be difficult to know which products are appropriate to use. The NEA Seal of Acceptance™ helps you The National Eczema Association (NEA) improves the health choose products that are suitable for the care of eczema or sensitive skin. and quality of life for individuals with eczema through research, support, and education. NEA is entirely supported through individual and corporate contributions and is a 501(c)(3) tax-exempt organization. NEA is the only organization in the Acceptance of a specific product does not represent an endorsement of that product. Acceptance of a product United States advocating solely for eczema patients. -

The Effects of Polysorbate 80 on the Fat Emulsion in Ice Cream Mix: Evidence from Transmission Electron Microscopy Studies
Food Structure Volume 6 Number 2 Article 11 1987 The Effects of Polysorbate 80 on the Fat Emulsion in Ice Cream Mix: Evidence from Transmission Electron Microscopy Studies H. D. Goff M. Liboff W. K. Jordan J. E. Kinsella Follow this and additional works at: https://digitalcommons.usu.edu/foodmicrostructure Part of the Food Science Commons Recommended Citation Goff, H. D.; Liboff, M.; Jordan, W. K.; and Kinsella, J. E. (1987) "The Effects of Polysorbate 80 on the Fat Emulsion in Ice Cream Mix: Evidence from Transmission Electron Microscopy Studies," Food Structure: Vol. 6 : No. 2 , Article 11. Available at: https://digitalcommons.usu.edu/foodmicrostructure/vol6/iss2/11 This Article is brought to you for free and open access by the Western Dairy Center at DigitalCommons@USU. It has been accepted for inclusion in Food Structure by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. FOOD MICROSTRUCTURE, VoL 6 (1987), pp. 193- 198 0730-54 19/87$3 . 00+- . 00 Scanning Microscopy International , Chicago (AMF O'Hare). IL 60666 USA THE EFFECTS OF POLYSORBATE 80 ON THE FAT EMULSION IN ICE CREAM MIX EVIDENCE FROM TRANSMISSION ELECTRON MICROSCOPY STUDIES H. D. Goff", M. Uboff, W. K. Jordan, and J. E. Kinsella Institute of Food Science, Stocking Hall Cornell University, Ithaca, New York 14853 Introduction Emulsifiers are used in ice cream to produce a dry, smooth Emulsifiers, such as mono- and di -glycerides or textured product with desirable melting properties. They function polyoxyethylene sorbitan esters, are used in ice cream to improve by promoting a partial destabilization of the fat emulsion. -

Topical Medications
Delegation of Medication Administering Topical Administration to Unlicensed Medication Module/Skill Checklist Assistive Personnel (UAP) Objective At the completion of this module, the UAP should be able to administer topical medications. Topical medications come in many forms – ointments, lotions, pastes, creams, powders, sprays, and shampoos. NOTE: 1) The RN or LPN is permitted to delegate ONLY after application of all components of the NCBON Decision Tree for Delegation to UAP and after careful consideration that delegation is appropriate: a) for this client, b) with this acuity level, c) with this individual UAP’s knowledge and experience, and d) now (or in the time period being planned). 2) Successful completion of the “Infection Control” module by the UAP should be documented prior to instruction in medication administration by this or ANY route. D DEFINITIONS Ointments are semi-solid preparations of drugs in an oil base. Lotions are medications dissolved in a liquid. Pastes are a mixture of powders and ointment and are often very stiff and sticky. Creams are medications in a suspension of oil and water and are easily applied to the skin. Powders are very finely ground medications that are usually sprinkled onto the affected area. Sprays are medications in a solution that can be atomized into a mist for ease of application. Shampoos are medications in a soap solution made for application to the scalp and hair. Page 1 of 3 Origin: 6/5/2014 Delegation of Medication Administering Topical Administration to Unlicensed Medication Module/Skill Checklist Assistive Personnel (UAP) Procedure 1. Perform skills in General Medication Administration Checklist. -

Medicare Drug List
MEDICARE BRANDED MEDICATIONS (B) *Each medication on this list may be available to MEDICARE patient HOWEVER, each manufacturer has varying rules for access to their medications. (examples: income only, denials from Medicaid/LIS, $or% of income spent out of pocket for Rx, donut hole...) MEDPro,LLC will assist patients with the process. *available medications are subject to change *MEDPro,LLC service charges for (B) medications are $20 per month per medication *FPL% of family income varies by manufacturer and by medication The average is typically 300% FPL (reflected in the chart published on website). HOWEVER the Range is 100% FPL – 400% FPL. *contact MEDPro,LLC for medication specific questions and income specific questions @1-888-715-0556 ext 3 BRAND NAME generic name Acular LS Ophthalmic Solution 0.4% ketorolac tromethamine LS OPHTH soln (B) Acular Ophthalmic Solution 0.4% ketorolac tromethamine OPHTH soln (B) Acuvail Ophthalmic Solution 0.45% ketorolac tromethamine OPHTH solution (B) Aczone Gel 5% TOPICAL dapsone gel TOPICAL (B) Adalat CC Tablet nifedipine CC tablet (B) Advair Diskus Inhalation powder fluticasone/salmeterol diskus inhaler (B) Advair HFA Aerosol; Inhalation fluticasone/salmeterol aerosol HFA inhaler (B) Alcaine Ophthalmic Drops 0.5% proparacainehcl OPHTH drops (B) Alomide Ophthalmic Drops 0.1% lodoxamide tromethamine OPHTH drops (B) Alphagan P Ophthalmic Solution 0.1% brimonidine tartrate OPHTH solution (B) Alrex Eye Suspension 0.2% loteprednol ophthalmic susp (B) Altabax Ointment retapamulin ointment (B) Amitiza Capsule -

Emulsions Systems for Skin Care: from Macro to Nano-Formulations Farid Menaa* Executive Director, Fluorotronics USA, Inc
ical C eut are ac & Menaa, J Pharma Care Health Sys 2014, 1:2 m H r e a a DOI: 10.4172/jpchs.1000e104 h l t P h f S o y Journal of l s a t n e r m u s o J ISSN: 2376-0419 Pharmaceutical Care & Health Systems EditorialResearch Article OpenOpen Access Access Emulsions Systems for Skin Care: From Macro to Nano-Formulations Farid Menaa* Executive Director, Fluorotronics USA, Inc. San Diego, CA, USA Aging of the skin, the largest human body´s organ, is a gradual Another type of emulsion, rarely used due to its complexity in process that involves both intrinsic molecules (e.g. reactive oxygen nature and instability issues, is known as multiple emulsions [18]. In species (ROS) [1] and environmental factors (e.g. ultraviolet radiation such system, water-in-oil-in-water (W/O/W) emulsion (i.e. W/O plus [2,3]. During this process, the skin appearance and functions are altered hydrophilic emulsifier) or oil-in-water-in-oil (O/W/O) emulsion (i.e. (e.g. stimulated release of collagenase, elastase and hyaluronidase from O/W plus hydrophobic emulsifier) can be produced [12,19]. the extracellular matrix (ECM)) [1]. The signs of skin aging are visible in the form of wrinkles, uneven pigment appearance and skin atrophy Additionally, we can distinguish three types of size-dependent [2]. An aged skin will decrease the social comfort and self-confidence [4]. Topical applications of cosmetics in the form of emulsions, often Water used in lotions and creams (e.g.