Ultrasound-Guided Femoral Nerve Block Guideline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Femoral Nerve Block Characteristics Using Ropivacaine 0.2% Alone, with Epinephrine, Or with Lidocaine and Epinephrine
SCIENTIFIC ARTICLES THE FEMORAL NERVE BLOCK CHARACTERISTICS USING ROPIVACAINE 0.2% ALONE, WITH EPINEPHRINE, OR WITH LIDOCAINE AND EPINEPHRINE A.M. TAHA1,2 AND A.M. ABD-ELmaKSOUD31* Keywords: anesthetic techniques, regional, femoral; anaesthetics local, ropivacaine; equipment, ultrasound machines. Abstract Background: The objective of this study was to evaluate the femoral nerve block characteristics (onset, success rate and duration) using ropivacaine 0.2% alone; with epinephrine, or with lidocaine and epinephrine compared with that using ropivacaine 0.5%. Methods: Ninety six patients were included in this prospective controlled double blind study and were randomly allocated into four equal groups (n=24). All the patients received ultrasound guided femoral nerve block using 15 ml of either ropivacaine 0.5% (group 1), ropivacaine 0.2% (group 2), ropivacaine 0.2% with epinephrine (group 3) and ropivacaine 0.2% with lidocaine and epinephrine (group 4). The block onset, success rate and duration were recorded. Results: The motor onset was significantly delayed in group 2 (compared with the other three groups) and in group 3 (compared with group 4). However, the block success rate and duration were comparable in the four groups. Conclusion: In femoral nerve block, ropivacaine 0.2% may have a comparable success rate and duration to ropivacaine 0.5% but with a remarkably delayed motor onset that may be improved by adding epinephrine. Addition of lidocaine may further accelerate the motor onset. Introduction The femoral nerve block (FNB) is a commonly indicated block, and ropivacaine is a widely used long acting local anesthetic (LA)1,2. Peripheral nerve blocks can provide excellent anesthesia and postoperative analgesia 3,4. -

Ultrasound Guided Femoral Nerve Block
Ultrasound Guided Femoral Nerve Block Michael Blaivas, MD, FACEP, FAIUM Clinical Professor of Medicine University of South Carolina School of Medicine AIUM, Third Vice President President, Society for Ultrasound Medical Education Past President, WINFOCUS Editor, Critical Ultrasound Journal Sub-specialty Editor, Journal of Ultrasound in Medicine Emergency Medicine Atlanta, Georgia [email protected] Disclosures • No relevant disclosures to lecture Objectives • Discuss anatomy of femoral nerve • Discuss uses of femoral nerve block classically and 3-in-1 variant • Discuss technique of femoral nerve blockade under ultrasound • Discuss pitfalls and potential errors Femoral Nerve Block Advantages • Many uses of regional nerve blocks • Avoid narcotics and their complications • Allow for longer term pain control • Can be used in patients unfit for sedation – Poor lung health – Hypotensive – Narcotic dependence or sensitivity Femoral Nerve Blocks • Wide variety of potential indications for a femoral nerve block – Hip fracture – Knee dislocation – Femoral fracture – Laceration repair – Burn – Etc. Nerve Blocks in Community vs. Academic Setting • Weekend stays • Night time admissions • Time to get consult and clear • Referral and admission patters • All of these factors can lead to patients spending considerable time prior to OR • Procedural sedation vs. block Femoral Nerve Blocks • Several basic principles with US also • Specialized needles +/- • No nerve stimulator • Can see nerve directly and inject directly around target nerve or nerves • Only -
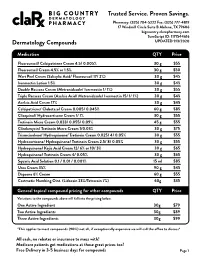
Pricing Sheet
Trusted Service. Proven Savings. Pharmacy: (325) 704-5222 Fax: (325) 777-4819 17 Windmill Circle Suite B Abilene, TX 79606 bigcountry.clarxpharmacy.com SureScript ID: 1171544616 Dermatology Compounds UPDATED 9/3/2020 Medication QTY Price Fluorouracil/ Calcipotriene Cream 4.5/ 0.005% 30 g $55 Fluorouracil Cream 4.5% or 1.5% 30 g $50 Wart Peel Cream (Salicylic Acid/ Fluorouracil 17/ 2%) 30 g $45 Ivermectin Lotion 1.5% 30 g $45 Double Rosacea Cream (Metronidazole/ Ivermectin 1/ 1%) 30 g $55 Triple Rosacea Cream (Azelaic Acid/ Metronidazole/ Ivermectin 15/ 1/ 1%) 30 g $45 Azelaic Acid Cream 17% 30 g $45 Calcipotriene/ Clobetasol Cream 0.005/ 0.045% 60 g $85 Clioquinol/ Hydrocortisone Cream 1/ 1% 30 g $55 Tretinoin Micro Cream 0.033/ 0.055/ 0.09% 45 g $55 Clindamycin/ Tretinoin Micro Cream 1/0.03% 30 g $75 Triamcinolone/ Hydroquinone/ Tretinoin Cream 0.025/ 4/ 0.05% 30 g $55 Hydrocortisone/ Hydroquinone/ Tretinoin Cream 2.5/ 8/ 0.05% 30 g $55 Hydroquinone/ Kojic Acid Cream 12/ 6% or 10/ 3% 30 g $65 Hydroquinone/ Tretinoin Cream 4/ 0.05% 30 g $65 Squaric Acid Solution 0.1 / 0.01 / 0.001% 15 ml $85 Urea Cream 35% 90 g $45 Dapsone 6% Cream 60 g $55 Costmetic Numbing Oint. (Lidocain 23%/Tetracain 7%) 60g $35 General topical compound pricing for other compounds QTY Price Variations to the compounds above will fall into the pricing below. One Active Ingredient 30g $79 Two Active Ingredients 30g $89 Three Active Ingredients 30g $99 *This applies to most compounds (90%) not all, if exceptionally expensive we will call the office to discuss* All cash, no rebates or insurance to mess with! Medicare patients get medications at these great prices too! Free Delivery in 3-5 business days for compounds Page 1 Trusted Service. -

Cream LOTRISONE® Lotion (Clotrimazole and Betamethasone Dipropionate)
LOTRISONE® Cream LOTRISONE® Lotion (clotrimazole and betamethasone dipropionate) FOR TOPICAL USE ONLY. NOT FOR OPHTHALMIC, ORAL, OR INTRAVAGINAL USE. NOT RECOMMENDED FOR PATIENTS UNDER THE AGE OF 17 YEARS AND NOT RECOMMENDED FOR DIAPER DERMATITIS. DESCRIPTION LOTRISONE® Cream and Lotion contain combinations of clotrimazole, a synthetic antifungal agent, and betamethasone dipropionate, a synthetic corticosteroid, for dermatologic use. Chemically, clotrimazole is 1–(o-chloro-α,α-diphenylbenzyl) imidazole, with the empirical formula C22H17CIN2, a molecular weight of 344.84, and the following structural formula: Clotrimazole is an odorless, white crystalline powder, insoluble in water and soluble in ethanol. Betamethasone dipropionate has the chemical name 9-fluoro-11β,17,21- trihydroxy-16β-methylpregna-1,4-diene-3,20-dione 17,21-dipropionate, with the empirical formula C28H37FO7, a molecular weight of 504.59, and the following structural formula: 1 LRN# 000370-LOS-MTL-USPI-1 Betamethasone dipropionate is a white to creamy white, odorless crystalline powder, insoluble in water. Each gram of LOTRISONE Cream contains 10 mg clotrimazole and 0.643 mg betamethasone dipropionate (equivalent to 0.5 mg betamethasone), in a hydrophilic cream consisting of purified water, mineral oil, white petrolatum, cetyl alcohol plus stearyl alcohol, ceteareth-30, propylene glycol, sodium phosphate monobasic monohydrate, and phosphoric acid; benzyl alcohol as preservative. LOTRISONE Cream may contain sodium hydroxide. LOTRISONE Cream is smooth, uniform, and white to off-white in color. Each gram of LOTRISONE Lotion contains 10 mg clotrimazole and 0.643 mg betamethasone dipropionate (equivalent to 0.5 mg betamethasone), in a hydrophilic base of purified water, mineral oil, white petrolatum, cetyl alcohol plus stearyl alcohol, ceteareth-30, propylene glycol, sodium phosphate monobasic monohydrate, and phosphoric acid; benzyl alcohol as a preservative. -
The International Student Journal of Nurse Anesthesia
Volume 15 Issue 1 Spring 2016 The International Student Journal of Nurse Anesthesia TOPICS IN THIS ISSUE Ondansetron to prevent SAB-induced Hypotension Hyperthermic Intraperitoneal Chemotherapy Carnitine Palmitoyltransferase Deficiency Adductor Canal vs. Femoral Nerve Block Ketamine Induction for Awake Intubation Airway Management for Tracheostomy TIVA for Gastroenterology Procedures Hematoma Following Thyroidectomy Tranexamic Acid in Trauma Tracheoesophageal Fistula Reintubation in the PACU Venous Air Embolism Emergence Delirium Preventing OR Fires INTERNATIONAL STUDENT JOURNAL OF NURSE ANESTHESIA Vol. 15 No. 1 Spring 2016 Editor Vicki C. Coopmans, CRNA, PhD Associate Editor Julie A. Pearson, CRNA, PhD Editorial Board Laura Ardizzone, CRNA, DNP Memorial Sloan Kettering Cancer Center; NY, NY MAJ Sarah Bellenger, CRNA, MSN, AN Darnall Army Medical Center; Fort Hood, TX Laura S. Bonanno, CRNA, DNP Louisiana State University Health Sciences Center Carrie C. Bowman Dalley, CRNA, MS Georgetown University Marianne Cosgrove, CRNA, DNAP Yale-New Haven Hospital School of Nurse Anesthesia LTC Denise Cotton, CRNA, DNAP, AN Winn Army Community Hospital; Fort Stewart, GA Janet A. Dewan, CRNA, PhD Northeastern University Kären K. Embrey CRNA, EdD University of Southern California Millikin University and Rhonda Gee, CRNA, DNSc Decatur Memorial Hospital Marjorie A. Geisz-Everson CRNA, PhD University of Southern Mississippi Johnnie Holmes, CRNA, PhD Naval Hospital Camp Lejeune Anne Marie Hranchook, CRNA, DNP Oakland University-Beaumont Donna Jasinski, -

Femoral and Sciatic Nerve Blocks for Total Knee Replacement in an Obese Patient with a Previous History of Failed Endotracheal Intubation −A Case Report−
Anesth Pain Med 2011; 6: 270~274 ■Case Report■ Femoral and sciatic nerve blocks for total knee replacement in an obese patient with a previous history of failed endotracheal intubation −A case report− Department of Anesthesiology and Pain Medicine, School of Medicine, Catholic University of Daegu, Daegu, Korea Jong Hae Kim, Woon Seok Roh, Jin Yong Jung, Seok Young Song, Jung Eun Kim, and Baek Jin Kim Peripheral nerve block has frequently been used as an alternative are situations in which spinal or epidural anesthesia cannot be to epidural analgesia for postoperative pain control in patients conducted, such as coagulation disturbances, sepsis, local undergoing total knee replacement. However, there are few reports infection, immune deficiency, severe spinal deformity, severe demonstrating that the combination of femoral and sciatic nerve blocks (FSNBs) can provide adequate analgesia and muscle decompensated hypovolemia and shock. Moreover, factors relaxation during total knee replacement. We experienced a case associated with technically difficult neuraxial blocks influence of successful FSNBs for a total knee replacement in a 66 year-old the anesthesiologist’s decision to perform the procedure [1]. In female patient who had a previous cancelled surgery due to a failed tracheal intubation followed by a difficult mask ventilation for 50 these cases, peripheral nerve block can provide a good solution minutes, 3 days before these blocks. FSNBs were performed with for operations on a lower extremity. The combination of 50 ml of 1.5% mepivacaine because she had conditions precluding femoral and sciatic nerve blocks (FSNBs) has frequently been neuraxial blocks including a long distance from the skin to the used for postoperative pain control after total knee replacement epidural space related to a high body mass index and nonpalpable lumbar spinous processes. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -

Salicylic Acid
Treatment Guide to Common Skin Conditions Prepared by Loren Regier, BSP, BA, Sharon Downey -www.RxFiles.ca Revised: Jan 2004 Dermatitis, Atopic Dry Skin Psoriasis Step 1 - General Treatment Measures Step 1 - General Treatment Measures Step 1 • Avoid contact with irritants or trigger factors • Use cool air humidifiers • Non-pharmacologic measures (general health issues) • Avoid wool or nylon clothing. • Lower house temperature (minimize perspiration) • Moisturizers (will not clear skin, but will ↓ itching) • Wash clothing in soap vs detergent; double rinse/vinegar • Limit use of soap to axillae, feet, and groin • Avoid frequent or prolonged bathing; twice weekly • Topical Steroids Step 2 recommended but daily bathing permitted with • Coal Tar • Colloidal oatmeal bath products adequate skin hydration therapy (apply moisturizer • Anthralin • Lanolin-free water miscible bath oil immediately afterwards) • Vitamin D3 • Intensive skin hydration therapy • Limit use of soap to axillae, feet, and groin • Topical Retinoid Therapy • “Soapless” cleansers for sensitive skin • Apply lubricating emollients such as petrolatum to • Sunshine Step 3 damp skin (e.g. after bathing) • Oral antihistamines (1st generation)for sedation & relief of • Salicylic acid itching give at bedtime +/- a daytime regimen as required Step 2 • Bath additives (tar solns, oils, oatmeal, Epsom salts) • Topical hydrocortisone (0.5%) for inflammation • Colloidal oatmeal bath products Step 2 apply od-tid; ointments more effective than creams • Water miscible bath oil • Phototherapy (UVB) may use cream during day & ointment at night • Humectants: urea, lactic acid, phospholipid • Photochemotherapy (Psoralen + UVA) Step 4 Step 3 • Combination Therapies (from Step 1 & 2 treatments) • Prescription topical corticosteroids: use lowest potency • Oral antihistamines for sedation & relief of itching steroid that is effective and wean to twice weekly. -

(6337) Smartpharmacy.Com
Phone 1.877.811.MEDS (6337) Fax 800.910.7195 SmartPharmacy.com Your prescription has been faxed to SMART PHARMACY Fax: (800) 910-7195 Phone: (877) 811-MEDS (6337) ** SHIPPING IS ALWAYS FREE Your physician has prescribed a topical cream to treat your pain and inflammation. Please review the following information about your prescription. HOW DO I FILL MY PRESCRIPTION? HOW DO I APPLY THE CREAM? • In most cases, your physician’s office will fax your The proper application of the cream is imperative to achieve prescription directly to Smart Pharmacy. A Smart Pharmacy maximum results; therefore, be sure to follow directions on the Registered Pharmacy Technician will begin processing your prescription label. prescription and contact you by phone. • Your prescription will arrive in an easy-to-use pump applicator. • Please leave a good contact number for calling or texting in order to expedite your order. • Clean and dry the affected area prior to applying topical cream with each application. • With your approval, the prescription will be shipped directly to your home or business at no charge. • Use latex gloves or thoroughly wash hands before and after each application. Do not apply to open wounds. Do not touch eyes or WILL INSURANCE COVER MY SMART mouth before washing hands as you may cause burning and irritation. PHARMACY PRESCRIPTION? • Most commercial insurance plans cover topical preparations with a reasonable co-pay. • Apply a liberal amount to affected area and rub in well as directed by your physician, massaging the affected area for 1-2 minutes. • Smart Pharmacy will verify your coverage and discuss your co-pay obligation. -

Drugs That Are Not Covered
Drugs that are Not Covered* Current 10/1/21 In addition to this list, newly marketed prescription medications may not be covered until the Pharmacy & Therapeutics Committee has had an opportunity to review the medication, to determine whether the medication will be covered and if so, which tier will apply based on safety, efficacy and the availability of other products within that class of medications. The current list of newly marketed drugs can be found on our New to Market Drug list. Abilify tablets albuterol HFA inhalers (authorized Apexicon E cream Abilify MyCite tablets generics for ProAir, Proventil, Ventolin Apidra vials Absorica capsules HFA inhalers) Apidra SoloStar injection Absorica LD capsules Aldactone tablets Aplenzin tablets Abstral sublingual tablets Aldara cream Apriso capsules Acanya gel and pump gel Alkindi sprinkle capsules Arava tablets Accupril tablets Allegra Children’s Allergy ODT Arazlo lotion acetaminophen 320.5 mg/caffeine 30 Allegra ODT, suspension and tablets Arestin microspheres mg/dihydrocodeine 16 mg Alltizal tablets Aricept tablets capsulesAciphex tablets alogliptin (authorized generic for Aricept ODT Aciphex Sprinkle capsules Nesina) Arimidex tablets Acticlate tablets alogliptin/metformin tablets (authorized Arixtra injection Active-Prep kits generic for Kazano) ArmonAir Digihaler inhaler Activella tablets alogliptin/pioglitazone (authorized ArmonAir Respiclick inhaler Actonel tablets generic for Oseni) Aromasin tablets Actoplus Met tablets Alphagan P 0.1% eye drops Arthrotec 50 and 75 tablets Actos -

Important Pharmacy Information There Is No Copay When Your Primary Care Provider (PCP) Or Unitedhealthcare Community Plan Specialist Writes You a Covered Prescription
Important Pharmacy Information There is no copay when your Primary Care Provider (PCP) or UnitedHealthcare Community Plan Specialist writes you a covered prescription. But you can get many over-the-counter (OTC) medicines free when you have a prescription. You can get the medications listed on the following pages when they are medically necessary and you get a written prescription from your UnitedHealthcare Community Plan doctor and take it to a UnitedHealthcare Community Plan pharmacy. To get your medicine: • Take your prescription to a UnitedHealthcare Community Plan pharmacy. To find a pharmacy, call 1-800-903-5253 or go to UHCCommunityPlan.com. • For your safety, we urge you to select a single pharmacy from which to get your drugs. • Get to know the pharmacist and build a relationship. If the UnitedHealthcare Community Plan pharmacy says they cannot fill your covered prescription or you have to pay more than your copay: Do not leave the pharmacy. Do not pay for it yourself. Ask the pharmacy why they cannot fill your prescription. Response Your Solution Not Covered • Ask them to call OptumRx right away to find out which medicine is covered. • Ask them to call your doctor to see if you can get the covered medicine instead. Prior • Ask them to call your doctor for a prior authorization. Authorization • You can call your doctor and ask that a prior authorization be sent to: Needed UnitedHealthcare Pharmacy Prior Notification Service Fax 1-866-940-7328 Phone 1-800-310-6826 Refill Too Soon • Ask what day it can be filled. • Pick your prescription up the day it can be filled. -

Running Head: ANESTHETIC MANAGEMENT in ERAS PROTOCOLS 1
Running head: ANESTHETIC MANAGEMENT IN ERAS PROTOCOLS 1 ANESTHETIC MANAGEMENT IN ERAS PROTOCOLS FOR TOTAL KNEE AND TOTAL HIP ARTHROPLASTY: AN INTEGRATIVE REVIEW Laura Oseka, BSN, RN Bryan College of Health Sciences ANESTHETIC MANAGEMENT IN ERAS PROTOCOLS 2 Abstract Aims and objectives: The aim of this integrative review is to provide current, evidence-based anesthetic and analgesic recommendations for inclusion in an enhanced recovery after surgery (ERAS) protocol for patients undergoing total knee arthroplasty (TKA) or total hip arthroplasty (THA). Methods: Articles published between 2006 and December 2016 were critically appraised for validity, reliability, and rigor of study. Results: The administration of non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, gabapentinoids, and steroids result in shorter hospital length of stay (LOS) and decreased postoperative pain and opioid consumption. A spinal anesthetic block provides benefits over general anesthesia, such as decreased 30-day mortality rates, hospital LOS, blood loss, and complications in the hospital. The use of peripheral nerve blocks result in lower pain scores, decreased opioid consumption, fewer complications, and shorter hospital LOS. Conclusion: Perioperative anesthetic management in ERAS protocols for TKA and THA patients should include the administration of acetaminophen, NSAIDs, gabapentinoids, and steroids. Preferred intraoperative anesthetic management in ERAS protocols should consist of spinal anesthesia with light sedation. Postoperative pain should be