The Stepwise Approach to the Treatment of Melasma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Melanocytes and Their Diseases
Downloaded from http://perspectivesinmedicine.cshlp.org/ on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Melanocytes and Their Diseases Yuji Yamaguchi1 and Vincent J. Hearing2 1Medical, AbbVie GK, Mita, Tokyo 108-6302, Japan 2Laboratory of Cell Biology, National Cancer Institute, National Institutes of Health, Bethesda, Maryland 20892 Correspondence: [email protected] Human melanocytes are distributed not only in the epidermis and in hair follicles but also in mucosa, cochlea (ear), iris (eye), and mesencephalon (brain) among other tissues. Melano- cytes, which are derived from the neural crest, are unique in that they produce eu-/pheo- melanin pigments in unique membrane-bound organelles termed melanosomes, which can be divided into four stages depending on their degree of maturation. Pigmentation production is determined by three distinct elements: enzymes involved in melanin synthesis, proteins required for melanosome structure, and proteins required for their trafficking and distribution. Many genes are involved in regulating pigmentation at various levels, and mutations in many of them cause pigmentary disorders, which can be classified into three types: hyperpigmen- tation (including melasma), hypopigmentation (including oculocutaneous albinism [OCA]), and mixed hyper-/hypopigmentation (including dyschromatosis symmetrica hereditaria). We briefly review vitiligo as a representative of an acquired hypopigmentation disorder. igments that determine human skin colors somes can be divided into four stages depend- Pinclude melanin, hemoglobin (red), hemo- ing on their degree of maturation. Early mela- siderin (brown), carotene (yellow), and bilin nosomes, especially stage I melanosomes, are (yellow). Among those, melanins play key roles similar to lysosomes whereas late melanosomes in determining human skin (and hair) pigmen- contain a structured matrix and highly dense tation. -

Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

Melasma (1 of 8)
Melasma (1 of 8) 1 Patient presents w/ symmetric hyperpigmented macules, which can be confl uent or punctate suggestive of melasma 2 DIAGNOSIS No ALTERNATIVE Does clinical presentation DIAGNOSIS confirm melasma? Yes A Non-pharmacological therapy • Patient education • Camoufl age make-up • Sunscreen B Pharmacological therapy Monotherapy • Hydroquinone or • Tretinoin TREATMENT Responding to No treatment? See next page Yes Continue treatment © MIMSas required Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B94 © MIMS 2019 Melasma (2 of 8) Patient unresponsive to initial therapy MELASMA A Non-pharmacological therapy • Patient education • Camoufl age make-up • Sunscreen B Pharmacological therapy Dual Combination erapy • Hydroquinone plus • Tretinoin or • Azelaic acid Responding to Yes Continue treatment treatment? as required No A Non-pharmacological therapy • Patient education • Camoufl age make-up • Sunscreen • Laser therapy • Dermabrasion B Pharmacological therapy Triple Combination erapy • Hydroquinone plus • Tretinoin plus • Topical steroid Chemical peels 1 MELASMA • Acquired hyperpigmentary skin disorder characterized by irregular light to dark brown macules occurring in the sun-exposed areas of the face, neck & arms - Occurs most commonly w/ pregnancy (chloasma) & w/ the use of contraceptive pills - Other factors implicated in the etiopathogenesis are photosensitizing medications, genetic factors, mild ovarian or thyroid dysfunction, & certain cosmetics • Most commonly aff ects Fitzpatrick skin phototypes III & IV • More common in women than in men • Rare before puberty & common in women during their reproductive years • Solar & ©ultraviolet exposure is the mostMIMS important factor in its development Not all products are available or approved for above use in all countries. -
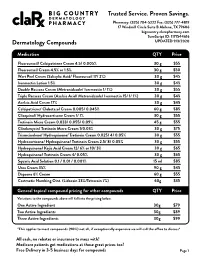
Pricing Sheet
Trusted Service. Proven Savings. Pharmacy: (325) 704-5222 Fax: (325) 777-4819 17 Windmill Circle Suite B Abilene, TX 79606 bigcountry.clarxpharmacy.com SureScript ID: 1171544616 Dermatology Compounds UPDATED 9/3/2020 Medication QTY Price Fluorouracil/ Calcipotriene Cream 4.5/ 0.005% 30 g $55 Fluorouracil Cream 4.5% or 1.5% 30 g $50 Wart Peel Cream (Salicylic Acid/ Fluorouracil 17/ 2%) 30 g $45 Ivermectin Lotion 1.5% 30 g $45 Double Rosacea Cream (Metronidazole/ Ivermectin 1/ 1%) 30 g $55 Triple Rosacea Cream (Azelaic Acid/ Metronidazole/ Ivermectin 15/ 1/ 1%) 30 g $45 Azelaic Acid Cream 17% 30 g $45 Calcipotriene/ Clobetasol Cream 0.005/ 0.045% 60 g $85 Clioquinol/ Hydrocortisone Cream 1/ 1% 30 g $55 Tretinoin Micro Cream 0.033/ 0.055/ 0.09% 45 g $55 Clindamycin/ Tretinoin Micro Cream 1/0.03% 30 g $75 Triamcinolone/ Hydroquinone/ Tretinoin Cream 0.025/ 4/ 0.05% 30 g $55 Hydrocortisone/ Hydroquinone/ Tretinoin Cream 2.5/ 8/ 0.05% 30 g $55 Hydroquinone/ Kojic Acid Cream 12/ 6% or 10/ 3% 30 g $65 Hydroquinone/ Tretinoin Cream 4/ 0.05% 30 g $65 Squaric Acid Solution 0.1 / 0.01 / 0.001% 15 ml $85 Urea Cream 35% 90 g $45 Dapsone 6% Cream 60 g $55 Costmetic Numbing Oint. (Lidocain 23%/Tetracain 7%) 60g $35 General topical compound pricing for other compounds QTY Price Variations to the compounds above will fall into the pricing below. One Active Ingredient 30g $79 Two Active Ingredients 30g $89 Three Active Ingredients 30g $99 *This applies to most compounds (90%) not all, if exceptionally expensive we will call the office to discuss* All cash, no rebates or insurance to mess with! Medicare patients get medications at these great prices too! Free Delivery in 3-5 business days for compounds Page 1 Trusted Service. -

Frequency of Different Types of Facial Melanoses Referring to the Department of Dermatology and Venereology, Nepal Medical Colle
Amatya et al. BMC Dermatology (2020) 20:4 https://doi.org/10.1186/s12895-020-00100-3 RESEARCH ARTICLE Open Access Frequency of different types of facial melanoses referring to the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital in 2019, and assessment of their effect on health-related quality of life Bibush Amatya* , Anil Kumar Jha and Shristi Shrestha Abstract Background: Abnormalities of facial pigmentation, or facial melanoses, are a common presenting complaint in Nepal and are the result of a diverse range of conditions. Objectives: The objective of this study was to determine the frequency, underlying cause and impact on quality of life of facial pigmentary disorders among patients visiting the Department of Dermatology and Venereology, Nepal Medical College and Teaching Hospital (NMCTH) over the course of one year. Methods: This was a cross-sectional study conducted at the Department of Dermatology and Venereology, NMCT H. We recruited patients with facial melanoses above 16 years of age who presented to the outpatient department. Clinical and demographic data were collected and all the enrolled participants completed the validated Nepali version of the Dermatology Life Quality Index (DLQI). Results: Between January 5, 2019 to January 4, 2020, a total of 485 patients were recruited in the study. The most common diagnoses were melasma (166 patients) and post acne hyperpigmentation (71 patients). Quality of life impairment was highest in patients having melasma with steroid induced rosacea-like dermatitis (DLQI = 13.54 ± 1.30), while it was lowest in participants with ephelides (2.45 ± 1.23). Conclusion: Facial melanoses are a common presenting complaint and lead to substantial impacts on quality of life. -

Clinicopathological Correlation of Acquired Hyperpigmentary Disorders
Symposium Clinicopathological correlation of acquired Dermatopathology hyperpigmentary disorders Anisha B. Patel, Raj Kubba1, Asha Kubba1 Department of Dermatology, ABSTRACT Oregon Health Sciences University, Portland, Oregon, Acquired pigmentary disorders are group of heterogenous entities that share single, most USA, 1Delhi Dermatology Group, Delhi Dermpath significant, clinical feature, that is, dyspigmentation. Asians and Indians, in particular, are mostly Laboratory, New Delhi, India affected. Although the classic morphologies and common treatment options of these conditions have been reviewed in the global dermatology literature, the value of histpathological evaluation Address for correspondence: has not been thoroughly explored. The importance of accurate diagnosis is emphasized here as Dr. Asha Kubba, the underlying diseases have varying etiologies that need to be addressed in order to effectively 10, Aradhana Enclave, treat the dyspigmentation. In this review, we describe and discuss the utility of histology in the R.K. Puram, Sector‑13, diagnostic work of hyperpigmentary disorders, and how, in many cases, it can lead to targeted New Delhi ‑ 110 066, India. E‑mail: and more effective therapy. We focus on the most common acquired pigmentary disorders [email protected] seen in Indian patients as well as a few uncommon diseases with distinctive histological traits. Facial melanoses, including mimickers of melasma, are thoroughly explored. These diseases include lichen planus pigmentosus, discoid lupus erythematosus, drug‑induced melanoses, hyperpigmentation due to exogenous substances, acanthosis nigricans, and macular amyloidosis. Key words: Facial melanoses, histology of hyperpigmentary disorders and melasma, pigmentary disorders INTRODUCTION focus on the most common acquired hyperpigmentary disorders seen in Indian patients as well as a few Acquired pigmentary disorders are found all over the uncommon diseases with distinctive histological traits. -

Dermatologic Manifestations of Hermansky-Pudlak Syndrome in Patients with and Without a 16–Base Pair Duplication in the HPS1 Gene
STUDY Dermatologic Manifestations of Hermansky-Pudlak Syndrome in Patients With and Without a 16–Base Pair Duplication in the HPS1 Gene Jorge Toro, MD; Maria Turner, MD; William A. Gahl, MD, PhD Background: Hermansky-Pudlak syndrome (HPS) con- without the duplication were non–Puerto Rican except sists of oculocutaneous albinism, a platelet storage pool de- 4 from central Puerto Rico. ficiency, and lysosomal accumulation of ceroid lipofuscin. Patients with HPS from northwest Puerto Rico are homozy- Results: Both patients homozygous for the 16-bp du- gous for a 16–base pair (bp) duplication in exon 15 of HPS1, plication and patients without the duplication dis- a gene on chromosome 10q23 known to cause the disorder. played skin color ranging from white to light brown. Pa- tients with the duplication, as well as those lacking the Objective: To determine the dermatologic findings of duplication, had hair color ranging from white to brown patients with HPS. and eye color ranging from blue to brown. New findings in both groups of patients with HPS were melanocytic Design: Survey of inpatients with HPS by physical ex- nevi with dysplastic features, acanthosis nigricans–like amination. lesions in the axilla and neck, and trichomegaly. Eighty percent of patients with the duplication exhibited fea- Setting: National Institutes of Health Clinical Center, tures of solar damage, including multiple freckles, stel- Bethesda, Md (a tertiary referral hospital). late lentigines, actinic keratoses, and, occasionally, basal cell or squamous cell carcinomas. Only 8% of patients Patients: Sixty-five patients aged 3 to 54 years were di- lacking the 16-bp duplication displayed these findings. -

Skin Care, Hair Care and Cosmetic Treatments in Pregnancy and Breastfeeding
Skin Care, Hair Care and Cosmetic Treatments in Pregnancy and Breastfeeding Information in this leaflet is general in nature and should not take the place of advice from your health care provider. With every pregnancy there is a 3 to 5% risk of having a baby with a birth defect. Issues for pregnancy Many pregnant women have skin and hair concerns just as they did before pregnancy. Sometimes conditions such as acne actually worsen during pregnancy because of hormonal changes and often women notice darkening of their skin (melasma). However, due to concern about potentially hazardous exposures to their unborn babies, pregnant women are often uncertain about which products are safe for them to use. Generally cosmetic treatments are discretionary (not medically necessary) and if safety is uncertain, women should consider whether the product or treatment is really required. There are several considerations when evaluating whether a specific skin or hair product is unsafe in pregnancy. Firstly, the active ingredient in the product needs to be considered unsafe. Secondly, it also has to be able to reach the unborn baby in its mother’s womb by inhalation or absorption through the mother’s skin (topical application). Although there is often limited information about the actual safety of specific ingredients in skin products during pregnancy, if it is known that skin absorption is minimal then the exposure to the unborn baby is generally insignificant and the product or treatment is regarded as safe. Below is a summary of current advice. Cosmetics, Moisturisers and other Skin Care Products Cosmetics and over the counter skin products generally contain ingredients that are unlikely to be harmful in pregnancy as they are used by applying to the skin (rather than swallowing a tablet). -

Cream LOTRISONE® Lotion (Clotrimazole and Betamethasone Dipropionate)
LOTRISONE® Cream LOTRISONE® Lotion (clotrimazole and betamethasone dipropionate) FOR TOPICAL USE ONLY. NOT FOR OPHTHALMIC, ORAL, OR INTRAVAGINAL USE. NOT RECOMMENDED FOR PATIENTS UNDER THE AGE OF 17 YEARS AND NOT RECOMMENDED FOR DIAPER DERMATITIS. DESCRIPTION LOTRISONE® Cream and Lotion contain combinations of clotrimazole, a synthetic antifungal agent, and betamethasone dipropionate, a synthetic corticosteroid, for dermatologic use. Chemically, clotrimazole is 1–(o-chloro-α,α-diphenylbenzyl) imidazole, with the empirical formula C22H17CIN2, a molecular weight of 344.84, and the following structural formula: Clotrimazole is an odorless, white crystalline powder, insoluble in water and soluble in ethanol. Betamethasone dipropionate has the chemical name 9-fluoro-11β,17,21- trihydroxy-16β-methylpregna-1,4-diene-3,20-dione 17,21-dipropionate, with the empirical formula C28H37FO7, a molecular weight of 504.59, and the following structural formula: 1 LRN# 000370-LOS-MTL-USPI-1 Betamethasone dipropionate is a white to creamy white, odorless crystalline powder, insoluble in water. Each gram of LOTRISONE Cream contains 10 mg clotrimazole and 0.643 mg betamethasone dipropionate (equivalent to 0.5 mg betamethasone), in a hydrophilic cream consisting of purified water, mineral oil, white petrolatum, cetyl alcohol plus stearyl alcohol, ceteareth-30, propylene glycol, sodium phosphate monobasic monohydrate, and phosphoric acid; benzyl alcohol as preservative. LOTRISONE Cream may contain sodium hydroxide. LOTRISONE Cream is smooth, uniform, and white to off-white in color. Each gram of LOTRISONE Lotion contains 10 mg clotrimazole and 0.643 mg betamethasone dipropionate (equivalent to 0.5 mg betamethasone), in a hydrophilic base of purified water, mineral oil, white petrolatum, cetyl alcohol plus stearyl alcohol, ceteareth-30, propylene glycol, sodium phosphate monobasic monohydrate, and phosphoric acid; benzyl alcohol as a preservative. -

A Genome-Wide Association Study Reveals a Locus for Bilateral Iridal Hypopigmentation in Holstein Friesian Cattle Anne K
Hollmann et al. BMC Genetics (2017) 18:30 DOI 10.1186/s12863-017-0496-4 RESEARCHARTICLE Open Access A genome-wide association study reveals a locus for bilateral iridal hypopigmentation in Holstein Friesian cattle Anne K. Hollmann1, Martina Bleyer2, Andrea Tipold3, Jasmin N. Neßler3, Wilhelm E. Wemheuer1, Ekkehard Schütz1 and Bertram Brenig1* Abstract Background: Eye pigmentation abnormalities in cattle are often related to albinism, Chediak-Higashi or Tietz like syndrome. However, mutations only affecting pigmentation of coat color and eye have also been described. Herein 18 Holstein Friesian cattle affected by bicolored and hypopigmented irises have been investigated. Results: Affected animals did not reveal any ophthalmological or neurological abnormalities besides the specific iris color differences. Coat color of affected cattle did not differ from controls. Histological examination revealed a reduction of melanin pigment in the iridal anterior border layer and stroma in cases as cause of iris hypopigmentation. To analyze the genetics of the iris pigmentation differences, a genome-wide association study was performed using Illumina BovineSNP50 BeadChip genotypes of the 18 cases and 172 randomly chosen control animals. A significant association on bovine chromosome 8 (BTA8) was identified at position 60,990,733 with a -log10(p) = 9.17. Analysis of genotypic and allelic dependences between cases of iridal hypopigmentation and an additional set of 316 randomly selected Holstein Friesian cattle controls showed that allele A at position 60,990,733 on BTA8 (P =4.0e–08, odds ratio = 6.3, 95% confidence interval 3.02–13.17) significantly increased the chance of iridal hypopigmentation. Conclusions: The clinical appearance of the iridal hypopigmentation differed from previously reported cases of pigmentation abnormalities in syndromes like Chediak-Higashi or Tietz and seems to be mainly of cosmetic character. -

Hydroxychloroquine-Associated Hyperpigmentation Mimicking Elder Abuse
Dermatol Ther (Heidelb) (2013) 3:203–210 DOI 10.1007/s13555-013-0032-z CASE REPORT Hydroxychloroquine-Associated Hyperpigmentation Mimicking Elder Abuse Philip R. Cohen To view enhanced content go to www.dermtherapy-open.com Received: June 17, 2013 / Published online: August 14, 2013 Ó The Author(s) 2013. This article is published with open access at Springerlink.com ABSTRACT cleared of suspected elder abuse. A skin biopsy of the patient’s dyschromia confirmed the Background: Hydroxychloroquine may result diagnosis of hydroxychloroquine-associated in cutaneous dyschromia. Older individuals hyperpigmentation. who are the victims of elder abuse can present Conclusion: Hyperpigmentation of skin, with bruising and resolving ecchymoses. mucosa, and nails can be observed in patients Purpose: The features of hydroxychloroquine- treated with antimalarials, including associated hyperpigmentation are described, hydroxychloroquine. Elder abuse is a significant the mucosal and skin manifestations of elder and underreported problem in seniors. abuse are reviewed, and the mucocutaneous Cutaneous findings can aid in the discovery of mimickers of elder abuse are summarized. physical abuse, sexual abuse, and self-neglect in Case Report: An elderly woman being treated elderly individuals. However, medication- with hydroxychloroquine for systemic lupus associated effects, systemic conditions, and erythematosus developed drug-associated black accidental external injuries can mimic elder and blue pigmentation of her skin. The abuse. Therefore, a complete medical history dyschromia was misinterpreted by her and appropriate laboratory evaluation, including clinician as elder abuse and Adult Protective skin biopsy, should be conducted when the Services was notified. The family was eventually diagnosis of elder abuse is suspected. Keywords: Abuse; Dyschromia; Elderly; P. -

Salicylic Acid
Treatment Guide to Common Skin Conditions Prepared by Loren Regier, BSP, BA, Sharon Downey -www.RxFiles.ca Revised: Jan 2004 Dermatitis, Atopic Dry Skin Psoriasis Step 1 - General Treatment Measures Step 1 - General Treatment Measures Step 1 • Avoid contact with irritants or trigger factors • Use cool air humidifiers • Non-pharmacologic measures (general health issues) • Avoid wool or nylon clothing. • Lower house temperature (minimize perspiration) • Moisturizers (will not clear skin, but will ↓ itching) • Wash clothing in soap vs detergent; double rinse/vinegar • Limit use of soap to axillae, feet, and groin • Avoid frequent or prolonged bathing; twice weekly • Topical Steroids Step 2 recommended but daily bathing permitted with • Coal Tar • Colloidal oatmeal bath products adequate skin hydration therapy (apply moisturizer • Anthralin • Lanolin-free water miscible bath oil immediately afterwards) • Vitamin D3 • Intensive skin hydration therapy • Limit use of soap to axillae, feet, and groin • Topical Retinoid Therapy • “Soapless” cleansers for sensitive skin • Apply lubricating emollients such as petrolatum to • Sunshine Step 3 damp skin (e.g. after bathing) • Oral antihistamines (1st generation)for sedation & relief of • Salicylic acid itching give at bedtime +/- a daytime regimen as required Step 2 • Bath additives (tar solns, oils, oatmeal, Epsom salts) • Topical hydrocortisone (0.5%) for inflammation • Colloidal oatmeal bath products Step 2 apply od-tid; ointments more effective than creams • Water miscible bath oil • Phototherapy (UVB) may use cream during day & ointment at night • Humectants: urea, lactic acid, phospholipid • Photochemotherapy (Psoralen + UVA) Step 4 Step 3 • Combination Therapies (from Step 1 & 2 treatments) • Prescription topical corticosteroids: use lowest potency • Oral antihistamines for sedation & relief of itching steroid that is effective and wean to twice weekly.