Role of Integrin Alpha4 in Drug Resistance of Leukemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Anti-ITGA9 Monoclonal Antibody, Clone FQS0833 (DCABH-3776) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-ITGA9 monoclonal antibody, clone FQS0833 (DCABH-3776) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Rabbit monoclonal to Integrin alpha 9 Antigen Description Integrin alpha-9/beta-1 is a receptor for VCAM1, cytotactin and osteopontin. It recognizes the sequence A-E-I-D-G-I-E-L in cytotactin. Immunogen Synthetic peptide (the amino acid sequence is considered to be commercially sensitive) Isotype IgG Source/Host Rabbit Species Reactivity Mouse, Rat, Human Clone FQS0833 Purity Tissue culture supernatant Conjugate Unconjugated Applications WB, IHC-P Positive Control NIH3T3, A673, HepG2, and A549 cell lysates, Human lung and Human skin tissues Format Liquid Size 100 μl Buffer Preservative: 0.01% Sodium azide; Constituents: 50% Glycerol, 0.05% BSA Preservative 0.01% Sodium Azide Storage store at -20°C. Avoid freeze / thaw cycles. Ship Shipped at 4°C. GENE INFORMATION Gene Name ITGA9 integrin, alpha 9 [ Homo sapiens ] Official Symbol ITGA9 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Synonyms ITGA9; integrin, alpha 9; integrin alpha-9; ALPHA RLC; integrin; alpha 4 like; ITGA4L; RLC; integrin alpha-RLC; ALPHA-RLC; Entrez Gene ID 3680 Protein Refseq NP_002198 UniProt ID Q13797 Chromosome Location 3p21.3 Pathway Arrhythmogenic right ventricular cardiomyopathy (ARVC), organism-specific biosystem; Arrhythmogenic right ventricular cardiomyopathy (ARVC), conserved biosystem; Axon guidance, organism-specific biosystem; Cell adhesion molecules (CAMs), organism-specific biosystem; Cell adhesion molecules (CAMs), conserved biosystem; Developmental Biology, organism- specific biosystem; Dilated cardiomyopathy, organism-specific biosystem. -

Table 3: Average Gene Expression Profiles by Chromosome
Supplemental Data Table 1: Experimental Setup Correlation Array Reverse Fluor Array Extraction Coefficient Print Batch (Y/N) mean (range) DLD1-I.1 I A N DLD1-I.2 I B N 0.86 DLD1-I.3 I C N (0.79-0.90) DLD1-I.4 I C Y DLD1 DLD1-II.1 II D N DLD1-II.2 II E N 0.86 DLD1-II.3 II F N (0.74-0.94) DLD1-II.4 II F Y DLD1+3-II.1 II A N DLD1+3-II.2 II A N 0.85 DLD1 + 3 DLD1+3-II.3 II B N (0.64-0.95) DLD1+3-II.4 II B Y DLD1+7-I.1 I A N DLD1+7-I.2 I A N 0.79 DLD1 + 7 DLD1+7-I.3 I B N (0.68-0.90) DLD1+7-I.4 I B Y DLD1+13-I.1 I A N DLD1+13-I.2 I A N 0.88 DLD1 + 13 DLD1+13-I.3 I B N (0.84-0.91) DLD1+13-I.4 I B Y hTERT-HME-I.1 I A N hTERT-HME-I.2 I B N 0.85 hTERT-HME hTERT-HME-I.3 I C N (0.80-0.92) hTERT-HME-I.4 I C Y hTERT-HME+3-I.1 I A N hTERT-HME+3-I.2 I B N 0.84 hTERT-HME + 3 hTERT-HME+3-I.3 I C N (0.74-0.90) hTERT-HME+3-I.4 I C Y Supplemental Data Table 2: Average gene expression profiles by chromosome arm DLD1 hTERT-HME Ratio.7 Ratio.1 Ratio.3 Ratio.3 Chrom. -

Integrin Alpha 9 Antibody Product Data Sheet Tested Species Reactivity Details Human (Hu) Catalog Number: PA5-27771
Lot Number: QE2031191G Integrin alpha 9 Antibody Product Data Sheet Tested Species Reactivity Details Human (Hu) Catalog Number: PA5-27771 Size: 100 µL Tested Applications Dilution * Class: Polyclonal Western Blot (WB) 1:500-1:3000 Type: Antibody Immunohistochemistry (Paraffin) 1:100-1:1000 Clone: (IHC (P)) Host / Isotype: Rabbit / IgG * Suggested working dilutions are given as a guide only. It is recommended that the user titrates the product for use in their own experiment using appropriate negative and positive controls. Recombinant fragment corresponding to a region within Immunogen: amino acids 1 and 255 of Human Integrin alpha 9 Form Information Form: Liquid Concentration: 1mg/ml Purification: Antigen affinity chromatography PBS, pH 7, with 1% BSA, 20% Storage Buffer: glycerol Preservative: 0.01% thimerosal Storage Conditions: -20° C, Avoid Freeze/Thaw Cycles Product Specific Information General Information PA5-27771 targets Integrin alpha 9 in IHC (P) and WB applications and This gene encodes an alpha integrin. Integrins are heterodimeric integral shows reactivity with Human samples. membrane glycoproteins composed of an alpha chain and a beta chain that mediate cell-cell and cell-matrix adhesion. The protein encoded by this gene, The PA5-27771 immunogen is recombinant fragment corresponding to a when bound to the beta 1 chain, forms an integrin that is a receptor for region within amino acids 1 and 255 of Human Integrin alpha 9. VCAM1, cytotactin and osteopontin. Expression of this gene has been found For Research Use Only. Not for use in diagnostic procedures. Not for to be upregulated in small cell lung cancers. resale without express authorization. -
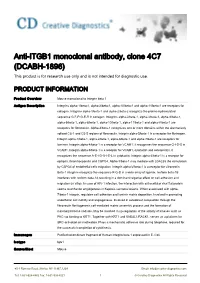
Anti-ITGB1 Monoclonal Antibody, Clone 4C7 (DCABH-1896) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-ITGB1 monoclonal antibody, clone 4C7 (DCABH-1896) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Mouse monoclonal to Integrin beta 1 Antigen Description Integrins alpha-1/beta-1, alpha-2/beta-1, alpha-10/beta-1 and alpha-11/beta-1 are receptors for collagen. Integrins alpha-1/beta-1 and alpha-2/beta-2 recognize the proline-hydroxylated sequence G-F-P-G-E-R in collagen. Integrins alpha-2/beta-1, alpha-3/beta-1, alpha-4/beta-1, alpha-5/beta-1, alpha-8/beta-1, alpha-10/beta-1, alpha-11/beta-1 and alpha-V/beta-1 are receptors for fibronectin. Alpha-4/beta-1 recognizes one or more domains within the alternatively spliced CS-1 and CS-5 regions of fibronectin. Integrin alpha-5/beta-1 is a receptor for fibrinogen. Integrin alpha-1/beta-1, alpha-2/beta-1, alpha-6/beta-1 and alpha-7/beta-1 are receptors for lamimin. Integrin alpha-4/beta-1 is a receptor for VCAM1. It recognizes the sequence Q-I-D-S in VCAM1. Integrin alpha-9/beta-1 is a receptor for VCAM1, cytotactin and osteopontin. It recognizes the sequence A-E-I-D-G-I-E-L in cytotactin. Integrin alpha-3/beta-1 is a receptor for epiligrin, thrombospondin and CSPG4. Alpha-3/beta-1 may mediate with LGALS3 the stimulation by CSPG4 of endothelial cells migration. Integrin alpha-V/beta-1 is a receptor for vitronectin. Beta-1 integrins recognize the sequence R-G-D in a wide array of ligands. -

Integrin and Gene Network Analysis Reveals That ITGA5 and ITGB1 Are Prognostic in Non-Small-Cell Lung Cancer
Journal name: OncoTargets and Therapy Article Designation: Original Research Year: 2016 Volume: 9 OncoTargets and Therapy Dovepress Running head verso: Zheng et al Running head recto: ITGA5 and ITGB1 are prognostic in NSCLC open access to scientific and medical research DOI: http://dx.doi.org/10.2147/OTT.S91796 Open Access Full Text Article ORIGINAL RESEARCH Integrin and gene network analysis reveals that ITGA5 and ITGB1 are prognostic in non-small-cell lung cancer Weiqi Zheng Background: Integrin expression has been identified as a prognostic factor in non-small-cell Caihui Jiang lung cancer (NSCLC). This study was aimed at determining the predictive ability of integrins Ruifeng Li and associated genes identified within the molecular network. Patients and methods: A total of 959 patients with NSCLC from The Cancer Genome Atlas Department of Radiation Oncology, Guangqian Hospital, Quanzhou, Fujian, cohorts were enrolled in this study. The expression profile of integrins and related genes were People’s Republic of China obtained from The Cancer Genome Atlas RNAseq database. Clinicopathological characteristics, including age, sex, smoking history, stage, histological subtype, neoadjuvant therapy, radiation therapy, and overall survival (OS), were collected. Cox proportional hazards regression models as well as Kaplan–Meier curves were used to assess the relative factors. Results: In the univariate Cox regression model, ITGA1, ITGA5, ITGA6, ITGB1, ITGB4, and ITGA11 were predictive of NSCLC prognosis. After adjusting for clinical factors, ITGA5 (odds ratio =1.17, 95% confidence interval: 1.05–1.31) andITGB1 (odds ratio =1.31, 95% confidence interval: 1.10–1.55) remained statistically significant. In the gene cluster network analysis, PLAUR, ILK, SPP1, PXN, and CD9, all associated with ITGA5 and ITGB1, were identified as independent predictive factors of OS in NSCLC. -

Both Full-Length and Protease-Cleaved Products of Osteopontin Are Elevated in Infectious Diseases
biomedicines Review Both Full-Length and Protease-Cleaved Products of Osteopontin Are Elevated in Infectious Diseases Toshio Hattori 1,* , Hiroko Iwasaki-Hozumi 1 , Gaowa Bai 1 , Haorile Chagan-Yasutan 1,2, Ashwnini Shete 3 , Elizabeth Freda Telan 4, Atsushi Takahashi 1, Yugo Ashino 5 and Takashi Matsuba 6 1 Research Institute of Health and Welfare, Kibi International University, Takahashi 716-8508, Japan; [email protected] (H.I.-H.); [email protected] (G.B.); [email protected] (H.C.-Y.); [email protected] (A.T.) 2 Mongolian Psychosomatic Medicine Department, International Mongolian Medicine Hospital of Inner Mongolia, Hohhot 010065, China 3 ICMR-National AIDS Research Institute, 73 G-Block, MIDC, Bhosari, Pune 411026, India; [email protected] 4 STD AIDS Cooperative Central Laboratory, San Lazaro Hospital, Manila 1003, Philippines; [email protected] 5 Department of Respiratory Medicine, Sendai City Hospital, Sendai 982-8502, Japan; [email protected] 6 Department of Animal Pharmaceutical Science, School of Pharmaceutical Science, Kyusyu University of Health and Welfare, Nobeoka 882-8508, Japan; [email protected] * Correspondence: [email protected]; Tel./Fax: +81-866-22-9469 Citation: Hattori, T.; Abstract: Circulating full-length osteopontin (FL-OPN) is elevated in plasma from patients with Iwasaki-Hozumi, H.; Bai, G.; various infectious diseases, such as adult T-cell leukemia, Mycobacterium tuberculosis (TB), hepatitis Chagan-Yasutan, H.; Shete, A.; Telan, virus infection, leptospirosis, acquired immune deficiency syndrome (AIDS), AIDS/TB, and coron- E.F.; Takahashi, A.; Ashino, Y.; avirus disease 2019 (COVID-19). Proteolysis of OPN by thrombin, matrix metalloproteases, caspase Matsuba, T. -

A Novel Α9 Integrin Ligand, XCL1/Lymphotactin, Is Involved in the Development of Murine Models of Autoimmune Diseases
A Novel α9 Integrin Ligand, XCL1/Lymphotactin, Is Involved in the Development of Murine Models of Autoimmune Diseases This information is current as of September 25, 2021. Naoki Matsumoto, Shigeyuki Kon, Takuya Nakatsuru, Tomoe Miyashita, Kyosuke Inui, Kodai Saitoh, Yuichi Kitai, Ryuta Muromoto, Jun-ichi Kashiwakura, Toshimitsu Uede and Tadashi Matsuda J Immunol 2017; 199:82-90; Prepublished online 26 May Downloaded from 2017; doi: 10.4049/jimmunol.1601329 http://www.jimmunol.org/content/199/1/82 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2017/05/26/jimmunol.160132 Material 9.DCSupplemental References This article cites 40 articles, 20 of which you can access for free at: http://www.jimmunol.org/content/199/1/82.full#ref-list-1 by guest on September 25, 2021 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2017 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology A Novel a9 Integrin Ligand, XCL1/Lymphotactin, Is Involved in the Development of Murine Models of Autoimmune Diseases Naoki Matsumoto,*,1 Shigeyuki Kon,*,†,1 Takuya Nakatsuru,* Tomoe Miyashita,* Kyosuke Inui,* Kodai Saitoh,* Yuichi Kitai,* Ryuta Muromoto,* Jun-ichi Kashiwakura,* Toshimitsu Uede,‡ and Tadashi Matsuda* The integrin a9b1 is a key receptor involved in the development of autoimmune diseases. -
![Integrin Alpha 9 (ITGA9) Mouse Monoclonal Antibody [Clone ID: Y9A2] Product Data](https://docslib.b-cdn.net/cover/8271/integrin-alpha-9-itga9-mouse-monoclonal-antibody-clone-id-y9a2-product-data-4478271.webp)
Integrin Alpha 9 (ITGA9) Mouse Monoclonal Antibody [Clone ID: Y9A2] Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for SM1281PT Integrin alpha 9 (ITGA9) Mouse Monoclonal Antibody [Clone ID: Y9A2] Product data: Product Type: Primary Antibodies Clone Name: Y9A2 Applications: FC, IP Recommended Dilution: Immunoprecipitation. Flow Cytometry. Reactivity: Guinea Pig, Human, Porcine Host: Mouse Isotype: IgG1 Clonality: Monoclonal Immunogen: Alpha-9 Integrin transfected lambda cells. Spleen cells from immunised BALB/c mice were fused with cells of the mouse SP2/0 myeloma cell line. Specificity: This antibody recognises the Human Alpha-9 Integrin. Clone Y9A2 inhibits adhesion of Alpha-9 expressing cells to N-terminal osteopontin. Formulation: PBS containing 0.09% Sodium Azide as preservative. State: Purified State: Liquid purified IgG fraction from Tissue Culture Supernatant Concentration: lot specific Purification: Affinity Chromatography on Protein G Conjugation: Unconjugated Storage: Store undiluted at 2-8°C for one month or (in aliquots) at -20°C for longer. Avoid repeated freezing and thawing. Stability: Shelf life: one year from despatch. Database Link: Entrez Gene 3680 Human Q13797 Background: Alpha9 integrin is a 140kD glycoprotein expressed as a heterodimer in association with the beta1 integrin. The alpha9 integrin is expressed by epithelial cells, including airway epithelial cells. This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 Integrin alpha 9 (ITGA9) Mouse Monoclonal Antibody [Clone ID: Y9A2] – SM1281PT Synonyms: Integrin alpha-RLC This product is to be used for laboratory only. -
![Anti-CD29 / Integrin Beta 1 Antibody [12G10] (ARG22982)](https://docslib.b-cdn.net/cover/0865/anti-cd29-integrin-beta-1-antibody-12g10-arg22982-4620865.webp)
Anti-CD29 / Integrin Beta 1 Antibody [12G10] (ARG22982)
Product datasheet [email protected] ARG22982 Package: 100 μg anti-CD29 / Integrin beta 1 antibody [12G10] Store at: -20°C Summary Product Description Mouse Monoclonal antibody [12G10] recognizes CD29 / Integrin beta 1 Mouse anti Human CD29 monoclonal antibody, clone 12G10 recognizes human CD29 also known as beta1 integrin or VLA-4 subunit alpha. CD29 is a ~130 kDa under reducing, ~115 kDa under non- reducing conditions single pass type I transmembrane glycoprotein. CD29 acts as the common beta subunit of the heterodimeric very late antigens 1-6, complexing with CD49a-f respectively where it forms part of the receptors for laminin , collagen and fibronectin. the VLA heterodimers ediate cell-cell and cell-matrix interactions.Mouse anti human CD29, clone 12G10 binding to cells adhering via VLA-4 results in actin cytoskeletal disruption and subsequent inhibition of attachment and spreading whilst 12G10 binding to cells adhering via VLA-5 results in enhancement of both these processes (Humphries et al. 2005). Clone 12G10 enhances alpha 5 beta 1-fibronectin interactions and binds to a region of CD25 containing the binding epitopes of several other anti CD29 antibody clones. However, unlike these, binding of 12G10 is enhanced in the presence of ligands such as fibronectin fragments (Mould et al. 1995). Binding of antibody clone 12G10 to the integrin β1 subunit is affected by divalent cations and the binding epitiope appears to be located around residues 207-218 in the b1 subunit putative A- domain (Mould et al. 1998) Tested Reactivity Hu Species Does Not React With Ms, Rat Tested Application ELISA, EM, FACS, ICC/IF, IHC-Fr, IP, WB Specificity The clone 12G10 binds to the CD29 / Integrin beta 1 βI domain then activates and stabilize the open headpiece conformation (active CD29 / Integrin beta 1). -

The 9 1 Integrin Enhances Cell Migration by Polyamine-Mediated
The ␣91 integrin enhances cell migration by polyamine-mediated modulation of an inward-rectifier potassium channel Gregory W. deHart*, Taihao Jin†, Diane E. McCloskey‡, Anthony E. Pegg‡, and Dean Sheppard*§ *Lung Biology Center, Department of Medicine, and †Howard Hughes Medical Institute, Department of Physiology, University of California, San Francisco, CA 94143; and ‡Department of Cellular and Molecular Physiology, Pennsylvania State University College of Medicine, Hershey, PA 17033 Edited by Lily Y. Jan, University of California School of Medicine, San Francisco, CA, and approved March 11, 2008 (received for review August 27, 2007) The ␣91 integrin accelerates cell migration through binding of dependent enhancement of cell migration (5). To systematically eval- spermidine/spermine acetyltransferase (SSAT) to the ␣9 cytoplasmic uate the role of SSAT catalytic activity, we studied six catalytically domain. We now show that SSAT enhances ␣9-mediated migration inactive mutants of SSAT (20, 21) with mutations scattered throughout specifically through catabolism of spermidine and/or spermine. Be- the protein. Each of these bound to the ␣9 cytoplasmic domain (Fig. cause spermine and spermidine are effective blockers of K؉ ion efflux 1a), but expression of any of three point mutants or three C-terminal -through inward-rectifier K؉ (Kir) channels, we examined the involve- truncation mutants caused comparable and significant dominant ment of Kir channels in this pathway. The Kir channel inhibitor, negative inhibition of migration on the ␣9-specific ligand, TNfn3RAA barium, or knockdown of a single subunit, Kir4.2, specifically inhib- (Fig. 1b) (5). A catalytically inactive mutant (K87A) did not affect ited ␣9-dependent cell migration. -

Rapid Isolation of Glomeruli Coupled with Gene Expression Profiling Identifies Downstream Targets in Pod1 Knockout Mice
Rapid Isolation of Glomeruli Coupled with Gene Expression Profiling Identifies Downstream Targets in Pod1 Knockout Mice Shiying Cui,* Chengjin Li,* Masatsugu Ema,† Jordan Weinstein,‡ and Susan E. Quaggin*‡ *The Samuel Lunenfeld Research Institute, University of Toronto, Toronto, Ontario, Canada; †Department of Anatomy and Embryology, Institute of Basic Medical Sciences, Division of Developmental Technology, Laboratory Animal Resource Center, University of Tsukuba, Tsukuba, Ibaraki, Japan; and ‡Division of Nephrology, St. Michael’s Hospital, University of Toronto, Toronto, Ontario, Canada Mouse mutations have provided tremendous insights into the molecular basis of renal and glomerular development. However, genes often play important roles during multiple stages of nephrogenesis, making it difficult to determine the role of a gene in a specific cell lineage such as the podocyte. Conditional gene targeting and chimeric analysis are two possible approaches to dissect the function of genes in specific cell populations. However, these are labor-intensive and costly and require the generation, validation, and analysis of additional transgenic lines. For overcoming these shortcomings and, specifically, for studying the role of gene function in developing glomeruli, a technique to isolate and purify glomeruli from murine embryos was developed. Combined with gene expression profiling, this method was used to identify differentially expressed genes in glomeruli from Pod1 knockout (KO) mice that die in the perinatal period with multiple renal defects. Glomeruli from early developing stages (late S-shape/early capillary loop) onward can be isolated successfully from wild-type and KO kidneys at 18.5 d postcoitus, and RNA can readily be obtained and used for genome-wide microarray analysis. With this approach, 3986 genes that are differently expressed between glomeruli from Pod1 KO and wild-type mice were identified, including a four-fold reduction of ␣ 8 integrin mRNA in glomeruli from Pod1 KO mice that was confirmed by immunostaining.