Cardiovascular
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypertension – Adult – Clinical Practice Guideline
Hypertension – Adult – Clinical Practice Guideline Table of Contents EXECUTIVE SUMMARY ........................................................................................................... 3 SCOPE ...................................................................................................................................... 4 METHODOLOGY ...................................................................................................................... 5 INTRODUCTION ....................................................................................................................... 5 RECOMMENDATIONS .............................................................................................................. 5 Establish the Diagnosis ........................................................................................... 5 Patient Evaluation ................................................................................................... 7 Treatment Goals ..................................................................................................... 7 Lifestyle Modifications ............................................................................................. 8 Table 4 – Lifestyle Modifications ........................................................................ 9 Medication Treatment............................................................................................ 11 Figure 1 - Initiation and Titration of Antihypertensive Medication ..................... 13 Table 7 - Antihypertensive -

Myocarditis in Acute Infective Diseases a Review of 200 Cases by C
Arch Dis Child: first published as 10.1136/adc.19.100.178 on 1 December 1944. Downloaded from MYOCARDITIS IN ACUTE INFECTIVE DISEASES A REVIEW OF 200 CASES BY C. NEUBAUER, M.D. Resident Medical Officer, City Hospital for Infectious Diseases, Newcastle upon Tyne The acute infective diseases constitute the most voltage in all three limb leads together. This sign important cause of myocarditis, the commonest occurs especially in cases of severe myocarditis. heart disease in childhood. Increasing amount of Pathological anatomy. Whenever possible the evidence from electrocardiographic investigations heart of a fatal case was examined in the Patho- of the heart in acute infective diseases shows that logical Department (Prof. B. Shaw) ofKing's College, there can be a myocarditis when clinical signs and Newcastle upon Tyne. Two illustrative cases are symptoms are slight, doubtful or completely absent. given: These investigations further revealed that many 1. convalescent cases whose unsatisfactory condition Sheila F., ten years, died on the eleventh day of diphtheria. Immediately beneath the ven- was accounted for by post-infective or secondary tricular anaemia were endocardium and also in the inner third of actually suffering from myocarditis. the wall are some scattered small foci of lymphoid Therefore, since this involvement of the myocardium and histiocytic cells. These foci sometimes occur is so common an event and liable to be missed or in association with shrunken muscle fibres and what misdiagnosed, it seems justifiable to give an account appear to be small delicate recent scars. of 200 cases of myocarditis occuring in acute 2. Iris N., eight years old,'died on the fourth day infectious diseases. -
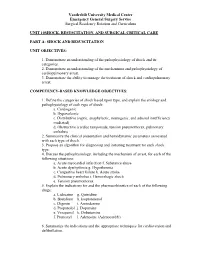
Unit 10 Shock,Resuscitation Part A
Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum UNIT 10SHOCK, RESUSCITATION, AND SURGICAL CRITICAL CARE PART A: SHOCK AND RESUSCITATION UNIT OBJECTIVES: 1. Demonstrate an understanding of the pathophysiology of shock and its categories. 2. Demonstrate an understanding of the mechanisms and pathophysiology of cardiopulmonary arrest. 3. Demonstrate the ability to manage the treatment of shock and cardiopulmonary arrest. COMPETENCY-BASED KNOWLEDGE OBJECTIVES: 1. Define the categories of shock based upon type, and explain the etiology and pathophysiology of each type of shock: a. Cardiogenic b. Hypovolemic c. Distributive (septic, anaphylactic, neurogenic, and adrenal insufficiency mediated) d. Obstructive (cardiac tamponade, tension pneumothorax, pulmonary embolus) 2. Summarize the clinical presentation and hemodynamic parameters associated with each type of shock. 3. Propose an algorithm for diagnosing and initiating treatment for each shock type. 4. Discuss the pathophysiology, including the mechanism of arrest, for each of the following situations: a. Acute myocardial infarction f. Substance abuse b. Acute dysrhythmia g. Hypothermia c. Congestive heart failure h. Acute stroke d. Pulmonary embolus i. Hemorrhagic shock e. Tension pneumothorax 5. Explain the indications for and the pharmacokinetics of each of the following drugs: a. Lidocaine g. Quinidine b. Bretylium h. Isoproterenol c. Digoxin i. Amiodarone d. Propanolol j. Dopamine e. Verapamil k. Dobutamine f. Pronestyl l. Adenosine (Adenocard®) 6. Summarize the indications and the appropriate techniques for cardioversion and defibrillation. Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum 7. Outline the signs and symptoms of acute airway obstruction and define the appropriate intervention in adult and pediatric patients. -

Approach to Shock.” These Podcasts Are Designed to Give Medical Students an Overview of Key Topics in Pediatrics
PedsCases Podcast Scripts This is a text version of a podcast from Pedscases.com on “Approach to Shock.” These podcasts are designed to give medical students an overview of key topics in pediatrics. The audio versions are accessible on iTunes or at www.pedcases.com/podcasts. Approach to Shock Developed by Dr. Dustin Jacobson and Dr Suzanne Beno for PedsCases.com. December 20, 2016 My name is Dustin Jacobson, a 3rd year pediatrics resident from the University of Toronto. This podcast was supervised by Dr. Suzanne Beno, a staff physician in the division of Pediatric Emergency Medicine at the University of Toronto. Today, we’ll discuss an approach to shock in children. First, we’ll define shock and understand it’s pathophysiology. Next, we’ll examine the subclassifications of shock. Last, we’ll review some basic and more advanced treatment for shock But first, let’s start with a case. Jonny is a 6-year-old male who presents with lethargy that is preceded by 2 days of a diarrheal illness. He has not urinated over the previous 24 hours. On assessment, he is tachycardic and hypotensive. He is febrile at 40 degrees Celsius, and is moaning on assessment, but spontaneously breathing. We’ll revisit this case including evaluation and management near the end of this podcast. The term “shock” is essentially a ‘catch-all’ phrase that refers to a state of inadequate oxygen or nutrient delivery for tissue metabolic demand. This broad definition incorporates many causes that eventually lead to this end-stage state. Basic oxygen delivery is determined by cardiac output and content of oxygen in the blood. -

Clinical Assessment in Acute Heart Failure
Hellenic J Cardiol 2015; 56: 285-301 Review Article Clinical Assessment in Acute Heart Failure 1 2 NIKOLAOS S. KAKOUROS , STAVROS N. KAKOUROS 1University of Massachusetts, MA, USA; 2Cardiac Department, “Amalia Fleming” General Hospital, Athens, Greece Key words: eart failure (HF) is defined as “a clear precipitant or trigger. It is very im Heart failure, complex clinical syn drome that portant to establish the precipitating diagnosis, physical examination, H can result from any structural or causes, which may have therapeutic and congestion. functional cardiac disorder that impairs the prognostic implications. Approximate ability of the ventricle to fill with, or eject ly 60% of patients with AHF have doc blood.” HF has an estimated overall prev umented CAD. Myocardial ischemia in alence of 2.6%. It is becoming more com the setting of acute coronary syndromes mon in adults older than 65 years, because is a precipitant or cause, particularly in of increased survival after acute myocar patients presenting with de novo AHF.4 dial infarction (AMI) and improved treat AHF is also often precipitated by medica ment of coronary artery disease (CAD), tion and dietary noncompliance, as well val vular heart disease and hypertension.1 as by many other conditions, which are Acute HF (AHF) is an increasingly com summarized in Table 1. Once the diagno mon cause of hospitalizations and mortality sis of AHF is confirmed, initial therapy in worldwide. In the majority of patients, AHF cludes removal of precipitants; if this can Manuscript received: can be attributed to worsening chronic HF, be carried out successfully, the patient’s August 25, 2014; and approximately 4050% of this group have subsequent course may be stable. -

Gallop Rhythm of the Heart.—Friedreich Muller (Miinch
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by ZENODO PROGRESS OP MEDICAL SCIENCE. MEDICINE. CNDER THE CHARGE OP WILLIAM OSLER, M.D, REGIUS PROFESSOR OF MEDICINE, OXFORD UNIVERSITT, ENGLAND, AND W. S THAYER, M.D., PROFESSOR OF CLINICAL MEDICINE, JOHNS HOPKINS UNIVERSITY, BALTIMORE, MARYLAND. Gallop Rhythm of the Heart.—Friedreich Muller (Miinch. med. JVoch., 1906, liii, 785). Gallop rhythm of the heart consists in the interposition of a third sound in the cardiac cycle. This sound occurs in diastole and is associated with a definite shock which is visible and easily palpable and makes a marked impression on the cardiograpbic record. In the cardiogram this impression may appear immediately before the systolic rise—the presystolic type, or in the first half of dias¬ tole, shortly after the second sound—the proto-diastolic type. Both of these waves are visible in the record of a normal apex-beat, although they are then very small elevations. They are pictured and studied by Marey in his classical work on the circulation and are particularly well illustrated in the tracings of Edgrem. It has been noted, too, that in cases of acute pericarditis in which there is certainly no change in the heart muscle, that the friction rub has a triple rhythm entirely analogous to the gallop rhvthm. The occurrence of the first or proto-diastolic wave corresponds with the period of greatest relaxation of the ventric¬ ular muscle and is synchronous with the negative wave or drop in the jugular pulse tracing; it marks the time when the blood begins to flow from the auricle into the ventricle. -

Complex Hypertension
COMPLEX HYPERTENSION Anita Ralstin, FNP-BC Next Step Health Consultant, LLC Incidence Of Hypertension ¨ About 70 million American adults have high blood pressure. About 33% of the population ¨ Only 52% have BP under control. ¨ Nearly a third of US adults have prehypertension. ¨ Hypertension costs $46 billion a year. (healthcare services, medications, missed work) From CDC Blood Pressure Facts 2015 What is Hypertension? ¨ JNC 7 (1997) definitions Stages Systolic Diastolic Prehypertension 102-129 OR 80-89 High BP Stage 1 140-159 OR 90-99 High BP Stage 2 160 or higher OR 100 or higher ¨ JNC 7 Goal BP = <140/90 ¨ JNC 8: did not define classification ¤ Patients 60 and +, start Rx when BP > 150/90* ¤ Patient < 60, start Rx when BP > 140/80 From National Heart, Lung Blood Institute SPRINT Study ¨ NIH supported study ¨ 9000+ subjects ¨ With at least one risk factor for CV disease ¨ Preliminary findings--- ¨ Adults 50 and older with HBP, targeting a SBP <120 reduced rates of CV events by 25%; reduced risk of death by 27% compared to a target of SBP 140. National Heart, Lung and Blood Institute Complex/Resistant Hypertension ¨ Resistant hypertension is defined as blood pressure that remains above goal despite concurrent use of three antihypertensive agents of different classes, one of which should be a diuretic. ¨ Patients whose blood pressure is controlled with four or more medications are considered to have resistant hypertension. Complex Hypertension ¨ BP above goal- 140/90 most patients. 130/80 diabetics or renal disease. ¨ Confirmed on at least two occasions with appropriate size cuff. ¨ Adherence to appropriate 3 drug regiment including a diuretic. -

Initial Approach to Hypertension in the Hemodynamics Unit: Review Article
REVIEW ARTICLE Initial approach to hypertension in the hemodynamics unit: review article Abordagem inicial da hipertensão arterial sistêmica em unidade de hemodinâmica: artigo de revisão Gustavo Teixeira Fulton Schimit1, José Manoel da Silva Silvestre2, Wander Eduardo Sardinha2, Eduardo Durante Ramires2, Domingos de Morais Filho2, Guilon Otávio Santos Tenório1, Fernando Barbosa Trevisan1 Abstract Correct identification and early management of hypertensive disorders should be a part of the therapeutic repertoire of every professional working in hemodynamics units. Based on recent publications, this study aims to propose a practical approach to the identification and early management of these disorders in this type of service. Keywords: hypertension; blood pressure; therapeutics; antihypertensive agents. Resumo O reconhecimento correto e manejo inicial das síndromes hipertensivas devem fazer parte do arsenal terapêutico de todo profissional que trabalhe em unidade de hemodinâmica. Este trabalho tem por objetivo, baseado em publicações recentes, propor uma abordagem prática para identificação e manejo inicial destes agravos nessa unidade. Palavras-chave: hipertensão; pressão arterial; terapêutica; anti-hipertensivos. 1Hospital Universitário Regional do Norte do Paraná, Londrina, PR, Brazil. 2Departamento de Clínica Cirúrgica, Universidade Estadual de Londrina – UEL, Londrina, PR, Brazil. Conflict of interest: No conflicts of interest declared concerning the publication of this article. Submitted on: 01.21.12. Accepted on: 03.25.13. The study was carried out at Hospital Universitário da Universidade Estadual de Londrina – UEL, Londrina, PR, Brazil. J Vasc Bras. 2013 Jun; 12(2):133-138 133 Hypertension in the hemodynamics unit INTRODUCTION been objectively adopted for the definition of normal Constant technical advances in the profession, blood pressure, and increases of 20/10 mm Hg above as well as in materials and new technologies, have this level double the risk of cardiovascular diseases11. -

Ministry of Health of Ukraine Kharkiv National Medical University
Ministry of Health of Ukraine Kharkiv National Medical University AUSCULTATION OF THE HEART. NORMAL HEART SOUNDS, REDUPLICATION OF THE SOUNDS, ADDITIONAL SOUNDS (TRIPLE RHYTHM, GALLOP RHYTHM), ORGANIC AND FUNCTIONAL HEART MURMURS Methodical instructions for students Рекомендовано Ученым советом ХНМУ Протокол №__от_______2017 г. Kharkiv KhNMU 2017 Auscultation of the heart. normal heart sounds, reduplication of the sounds, additional sounds (triple rhythm, gallop rhythm), organic and functional heart murmurs / Authors: Т.V. Ashcheulova, O.M. Kovalyova, O.V. Honchar. – Kharkiv: KhNMU, 2017. – 20 с. Authors: Т.V. Ashcheulova O.M. Kovalyova O.V. Honchar AUSCULTATION OF THE HEART To understand the underlying mechanisms contributing to the cardiac tones formation, it is necessary to remember the sequence of myocardial and valvular action during the cardiac cycle. During ventricular systole: 1. Asynchronous contraction, when separate areas of myocardial wall start to contract and intraventricular pressure rises. 2. Isometric contraction, when the main part of the ventricular myocardium contracts, atrioventricular valves close, and intraventricular pressure significantly increases. 3. The ejection phase, when the intraventricular pressure reaches the pressure in the main vessels, and the semilunar valves open. During diastole (ventricular relaxation): 1. Closure of semilunar valves. 2. Isometric relaxation – initial relaxation of ventricular myocardium, with atrioventricular and semilunar valves closed, until the pressure in the ventricles becomes lower than in the atria. 3. Phases of fast and slow ventricular filling - atrioventricular valves open and blood flows from the atria to the ventricles. 4. Atrial systole, after which cardiac cycle repeats again. The noise produced By a working heart is called heart sounds. In auscultation two sounds can be well heard in healthy subjects: the first sound (S1), which is produced during systole, and the second sound (S2), which occurs during diastole. -

3 Blood Pressure and Its Measurement
Chapter 3 / Blood Pressure and Its Measurement 49 3 Blood Pressure and Its Measurement CONTENTS PHYSIOLOGY OF BLOOD FLOW AND BLOOD PRESSURE PHYSIOLOGY OF BLOOD PRESSURE MEASUREMENT POINTS TO REMEMBER WHEN MEASURING BLOOD PRESSURE FACTORS THAT AFFECT BLOOD PRESSURE READINGS INTERPRETATION OF BLOOD PRESSURE MEASUREMENTS USE OF BLOOD PRESSURE MEASUREMENT IN SPECIAL CLINICAL SITUATIONS REFERENCES PHYSIOLOGY OF BLOOD FLOW AND BLOOD PRESSURE The purpose of the arterial system is to provide oxygenated blood to the tissues by converting the intermittent cardiac output into a continuous capillary flow and this is achieved by the structural organization of the arterial system. The blood flow in a vessel is basically determined by two factors: 1. The pressure difference between the two ends of the vessel, which provides the driving force for the flow 2. The impediment to flow, which is essentially the vascular resistance This can be expressed by the following formula: 6P Q = R where Q is the flow, 6P is the pressure difference, and R is the resistance. The pressure head in the aorta and the large arteries is provided by the pumping action of the left ventricle ejecting blood with each systole. The arterial pressure peaks in systole and tends to fall during diastole. Briefly, the peak systolic pressure achieved is determined by (see Chapter 2): 1. The momentum of ejection (the stroke volume, the velocity of ejection, which in turn are related to the contractility of the ventricle and the afterload) 2. The distensibility of the proximal arterial system 3. The timing and amplitude of the reflected pressure wave When the arterial system is stiff, as in the elderly, for the same amount of stroke output, the peak systolic pressure achieved will be higher. -

The Cardiovascular Examination
CHAPTER 1 The Cardiovascular Examination KEY POINTS • The cardiovascular examination lends itself to a systematic approach. • The examination should be thorough but should be directed by the history to areas likely to be relevant. • Certain cardiovascular signs are quite sensitive and specific. • When the examination is well performed, many unnecessary investigations can be avoided. CASE 1 SCENARIO: TARA WITH 3. Pick up the patient’s hand. Feel the radial pulse. DYSPNOEA Inspect the patient’s hands for clubbing. Demon- strate Schamroth’s sign (Fig. 1.1). If there is no 34-year-old Tara was referred to the hospital by her general clubbing, opposition of the index finger (nail to practitioner. She presented with increasing dyspnoea for the nail) demonstrates a diamond shape; in clubbing last 2 weeks. She has found it difficult to lie flat in bed and this space is lost. Also look for the peripheral has been waking up frequently feeling breathless. She also stigmata of infective endocarditis. Splinter haemor- has a dry cough and has felt extremely tired for weeks. She rhages are common (and are usually caused by also has high fever with a shake. She is an intravenous drug trauma), whereas Osler’s nodes and Janeway lesions user and her general practitioner (GP) found a loud murmur (Fig. 1.2) are rare. Look quickly, but carefully, at on auscultation. each nail bed, otherwise it is easy to miss key signs. Please examine the cardiovascular system. Note the presence of an intravenous cannula and, if an infusion is running, look at the bag to see The cardiovascular system should be examined in what it is. -

Quality Control of the Foot Revascularization Using Indocyanine Green Fluorescence Imaging
World J Surg (2017) 41:1919–1926 DOI 10.1007/s00268-017-3950-6 ORIGINAL SCIENTIFIC REPORT Quality Control of the Foot Revascularization Using Indocyanine Green Fluorescence Imaging 1 1 1 1 Nicla Settembre • Petteri Kauhanen • Anders Alba¨ck • Kristyna Spillerova • Maarit Venermo1 Published online: 6 March 2017 Ó Socie´te´ Internationale de Chirurgie 2017 Abstract Objectives Critical limb ischemia (CLI) is a clinical diagnosis, confirmed by objective tests, usually ankle-brachial index (ABI), toe pressure (TP) and TcPO2. Furthermore, the anatomical lesions in patients affected by CLI were visualized by ultrasound, angiography, CTA, or MRA. Indocyanine green fluorescence imaging (ICG-FI) is a diagnostic modality for assessing foot perfusion. We aimed to study the usefulness of ICG-FI in the quality control of revascularization. Materials and methods One hundred and four CLI limbs in 101 patients were studied with ICG-FI using SPY Elite before and after open or endovascular revascularization. ABI and TP were also measured. After ICG-FI, assessment of circulation was done using time–intensity curve derived from the two regions of interest the one being in the plantar side of the foot and the other in the dorsal side of the foot. Three parameters were derived from the curves: maximum intensity (the absolute value of the maximum intensity); intensity rate (the value from the time–intensity curve describing the increase in maximum intensity/s) and SPY10 (the intensity achieved during the first 10 s after the foot starts to gain intensity). Results Sixty-two limbs presented category 3 of Rutherford classification, 12 limbs category 4, and 30 limbs category 5.