Application for Inclusion of Hydrocortisone Tablets in the WHO Model List of Essential Medicines for Children (July 2008)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

House of Delegates Handbook (I-18
Reference Committee on Amendments to Constitution and Bylaws BOT Report(s) 14 Protection of Physician Freedom of Speech CEJA Report(s) 01* Competence, Self-Assessment and Self-Awareness 02* Study Aid-in-Dying as End-of-Life Option / The Need to Distinguish "Physician-Assisted Suicide" and "Aid- in-Dying" 03* Amendment to E-2.2.1, "Pediatric Decision Making" 04* CEJA Role in Implementing H-140.837, "Anti-Harassment Policy" 05* Physicians' Freedom of Speech Resolution(s) 001 Support of a National Registry for Advance Directives 002* Protecting the Integrity of Public Health Data Collection 003* Mental Health Issues and Use of Psychotropic Drugs for Undocumented Immigrant Children * contained in the Handbook Addendum REPORT OF THE BOARD OF TRUSTEES B of T Report 14-I-18 Subject: Protection of Physician Freedom of Speech (Resolution 5-I-17) Presented by: Jack Resneck, Jr. MD, Chair Referred to: Reference Committee on Amendments to Constitution and Bylaws (Todd M. Hertzberg, MD, Chair) 1 INTRODUCTION 2 3 Resolution 5-I-17, introduced by the American Academy of Pain Medicine (AAPM), consisted of 4 the following proposals: 5 6 RESOLVED, That our American Medical Association strongly oppose litigation challenging 7 the exercise of a physician’s First Amendment right to express good faith opinions regarding 8 medical issues; and be it further 9 10 RESOLVED, That our AMA’s House of Delegates encourage the AMA Litigation Center to 11 provide such support to a constituent or component medical society whose members have been 12 sued for expressing good faith opinions regarding medical issues as the Litigation Center 13 deems appropriate in any specific case. -

Adrenal Disorders
Adrenal Disorders Dual-release Hydrocortisone in Addison’s Disease— A Review of the Literature Roberta Giordano, MD,1 Federica Guaraldi, MD,2 Rita Berardelli, MD,2 Ioannis Karamouzis, MD,2 Valentina D’Angelo, MD,2 Clizia Zichi, MD,2 Silvia Grottoli, MD,2 Ezio Ghigo, PhD2 and Emanuela Arvat, PhD3 1. Department of Clinical and Biological Sciences; 2. Division of Endocrinology, Diabetology and Metabolism, Department of Medical Sciences; 3. Division of Oncological Endocrinology, Department of Medical Sciences, University of Turin, Turin, Italy Abstract In patients with adrenal insufficiency, glucocorticoids (GCs) are insufficiently secreted and GC replacement is essential for health and, indeed, life. Despite GC-replacement therapy, patients with adrenal insufficiency have a greater cardiovascular risk than the general population, and suffer from impaired health-related quality of life. Although the aim of the replacement GC therapy is to reproduce as much as possible the physiologic pattern of cortisol secretion by the normal adrenal gland, the pharmacokinetics of available oral immediate-release hydrocortisone or cortisone make it impossible to fully mimic the cortisol rhythm. Therefore, there is an unmet clinical need for the development of novel pharmaceutical preparations of hydrocortisone, in order to guarantee a more physiologic serum cortisol concentration time-profile, and to improve the long-term outcome in patients under GC substitution therapy. Keywords Addison’s disease, glucocorticoids, hydrocortisone, Plenadren®, limits, advantages Disclosure: The authors have no conflicts of interest to declare. Received: June 28, 2013 Accepted: August 9, 2013 Citation: US Endocrinology 2013;9(2):177–80 DOI: 10.17925/USE.2013.09.02.177 Correspondence: Roberta Giordano, MD, Division of Endocrinology, Diabetology and Metabolism, Department of Medical Sciences, Azienda Ospedaliera Città della Salute e della Scienza di Torino, C so Dogliotti 14, 10126 Turin, Italy. -
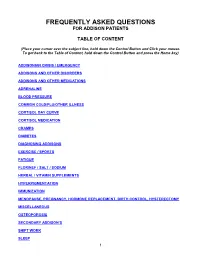
Frequently Asked Questions for Addison Patients
FREQUENTLY ASKED QUESTIONS FOR ADDISON PATIENTS TABLE OF CONTENT (Place your cursor over the subject line, hold down the Control Button and Click your mouse. To get back to the Table of Content, hold down the Control Button and press the Home key) ADDISONIAN CRISIS / EMERGENCY ADDISONS AND OTHER DISORDERS ADDISONS AND OTHER MEDICATIONS ADRENALINE BLOOD PRESSURE COMMON COLD/FLU/OTHER ILLNESS CORTISOL DAY CURVE CORTISOL MEDICATION CRAMPS DIABETES DIAGNOSING ADDISONS EXERCISE / SPORTS FATIGUE FLORINEF / SALT / SODIUM HERBAL / VITAMIN SUPPLEMENTS HYPERPIGMENTATION IMMUNIZATION MENOPAUSE, PREGNANCY, HORMONE REPLACEMENT, BIRTH CONTROL, HYSTERECTOMY MISCELLANEOUS OSTEOPOROSIS SECONDARY ADDISON’S SHIFT WORK SLEEP 1 STRESS DOSING SURGICAL, MEDICAL, DENTAL PROCEDURES THYROID TRAVEL WEIGHT GAIN 2 ADDISONIAN CRISIS / EMERGENCY How do you know when to call an ambulance? If you are careful, you should not have to call an ambulance. If someone with adrenal insufficiency has gastrointestinal problems and is unable to keep down their cortisol or other glucocorticoid for more than 24 hrs, they should be taken to an emergency department so they can be given intravenous solucortef and saline. It is not appropriate to wait until they are so ill that they cannot be taken to the hospital by a family member. If the individual is unable to retain anything by mouth and is very ill, or if they have had a sudden stress such as a fall or an infection, then it would be necessary for them to go by ambulance as soon as possible. It is important that you should have an emergency kit at home and that someone in the household knows how to use it. -

A New Pro-Natalist Tool: Parenthood As a Form of Public Employment
Trivent Publishing © The Authors, 2018 Available online at http://trivent-publishing.eu/ Series: Applied Ethics: From Bioethics to Environmental Ethics A New Pro-Natalist Tool: Parenthood as a Form of Public Employment János I. Tóth University of Szeged, Hungary Abstract: Low fertility rates currently represent a serious problem across Europe and East Asia. A possible solution to this crisis is the radical increase of fertility rates. I suggest that we distinguish between classical (3-child) pro-natalist and radical (5-child) pro-natalist policies, because their logic is different. Classical pro- natalism tries to harmonize childbearing and employment for the mother, while radical natalism considers bearing 5-6 children as work, as a kind of public employment. In this chapter, I elaborate on a possible radical pro-natalist institution: parenthood as a form of public employment. This institution, complete with classical pro-natalist measures, could best secure the fertility rate of 2.1 by 2030. Keywords: fertility rate; two forms of natalism; full-time parenthood; Eastern Europe. This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC-BY-NC-ND 4.0) license, which permits others to copy or share the article, provided original work is properly cited and that this is not done for commercial purposes. Users may not remix, transform, or build upon the material and may not distribute the modified material (http://creativecommons.org/licenses/by-nc/4.0/) 164 János I. Tóth A New Pro-Natalist Tool A New Pro-Natalist Tool: Parenthood as a Form of Public Employment János I. -

Steroid Use in Prednisone Allergy Abby Shuck, Pharmd Candidate
Steroid Use in Prednisone Allergy Abby Shuck, PharmD candidate 2015 University of Findlay If a patient has an allergy to prednisone and methylprednisolone, what (if any) other corticosteroid can the patient use to avoid an allergic reaction? Corticosteroids very rarely cause allergic reactions in patients that receive them. Since corticosteroids are typically used to treat severe allergic reactions and anaphylaxis, it seems unlikely that these drugs could actually induce an allergic reaction of their own. However, between 0.5-5% of people have reported any sort of reaction to a corticosteroid that they have received.1 Corticosteroids can cause anything from minor skin irritations to full blown anaphylactic shock. Worsening of allergic symptoms during corticosteroid treatment may not always mean that the patient has failed treatment, although it may appear to be so.2,3 There are essentially four classes of corticosteroids: Class A, hydrocortisone-type, Class B, triamcinolone acetonide type, Class C, betamethasone type, and Class D, hydrocortisone-17-butyrate and clobetasone-17-butyrate type. Major* corticosteroids in Class A include cortisone, hydrocortisone, methylprednisolone, prednisolone, and prednisone. Major* corticosteroids in Class B include budesonide, fluocinolone, and triamcinolone. Major* corticosteroids in Class C include beclomethasone and dexamethasone. Finally, major* corticosteroids in Class D include betamethasone, fluticasone, and mometasone.4,5 Class D was later subdivided into Class D1 and D2 depending on the presence or 5,6 absence of a C16 methyl substitution and/or halogenation on C9 of the steroid B-ring. It is often hard to determine what exactly a patient is allergic to if they experience a reaction to a corticosteroid. -

Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Cr
Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Crizotinib (PF-02341066) 1 4 55 Docetaxel 1 5 98 Anastrozole 1 6 25 Cladribine 1 7 23 Methotrexate 1 8 -187 Letrozole 1 9 65 Entecavir Hydrate 1 10 48 Roxadustat (FG-4592) 1 11 19 Imatinib Mesylate (STI571) 1 12 0 Sunitinib Malate 1 13 34 Vismodegib (GDC-0449) 1 14 64 Paclitaxel 1 15 89 Aprepitant 1 16 94 Decitabine 1 17 -79 Bendamustine HCl 1 18 19 Temozolomide 1 19 -111 Nepafenac 1 20 24 Nintedanib (BIBF 1120) 1 21 -43 Lapatinib (GW-572016) Ditosylate 1 22 88 Temsirolimus (CCI-779, NSC 683864) 1 23 96 Belinostat (PXD101) 1 24 46 Capecitabine 1 25 19 Bicalutamide 1 26 83 Dutasteride 1 27 68 Epirubicin HCl 1 28 -59 Tamoxifen 1 29 30 Rufinamide 1 30 96 Afatinib (BIBW2992) 1 31 -54 Lenalidomide (CC-5013) 1 32 19 Vorinostat (SAHA, MK0683) 1 33 38 Rucaparib (AG-014699,PF-01367338) phosphate1 34 14 Lenvatinib (E7080) 1 35 80 Fulvestrant 1 36 76 Melatonin 1 37 15 Etoposide 1 38 -69 Vincristine sulfate 1 39 61 Posaconazole 1 40 97 Bortezomib (PS-341) 1 41 71 Panobinostat (LBH589) 1 42 41 Entinostat (MS-275) 1 43 26 Cabozantinib (XL184, BMS-907351) 1 44 79 Valproic acid sodium salt (Sodium valproate) 1 45 7 Raltitrexed 1 46 39 Bisoprolol fumarate 1 47 -23 Raloxifene HCl 1 48 97 Agomelatine 1 49 35 Prasugrel 1 50 -24 Bosutinib (SKI-606) 1 51 85 Nilotinib (AMN-107) 1 52 99 Enzastaurin (LY317615) 1 53 -12 Everolimus (RAD001) 1 54 94 Regorafenib (BAY 73-4506) 1 55 24 Thalidomide 1 56 40 Tivozanib (AV-951) 1 57 86 Fludarabine -

Corticosteroids in Terminal Cancer-A Prospective Analysis of Current Practice
Postgraduate Medical Journal (November 1983) 59, 702-706 Postgrad Med J: first published as 10.1136/pgmj.59.697.702 on 1 November 1983. Downloaded from Corticosteroids in terminal cancer-a prospective analysis of current practice G. W. HANKS* T. TRUEMAN B.Sc., M.B., B.S., M.R.C.P.(U.K.) S.R.N. R. G. TWYCROSS M.A., D.M., F.R.C.P. Sir Michael Sobell House, The Churchill Hospital, Headington, Oxford OX3 7LJ Summary Introduction Over half of a group of 373 inpatients with advanced Corticosteroids have a major role to play in the malignant disease were treated with corticosteroids control of symptoms in patients with advanced for a variety of reasons. They received either pred- malignant disease. They may be employed in a non- nisolone or dexamethasone, or replacement therapy specific way to improve mood and appetite; or they with cortisone acetate. Forty percent of those receiv- may be indicated as specific adjunctive therapy in the ing corticosteroids benefited from them. A higher relief of symptoms related to a large tumour mass or response rate was seen when corticosteroids were to nerve compression. The management of a numberProtected by copyright. prescribed for nerve compression pain, for raised of other symptoms and syndromes may also be intracranial pressure, and when used in conjunction facilitated by treatment with corticosteroids (Table with chemotherapy. No significant difference in 1). efficacy was noted between the 2 drugs. The results, The use of corticosteroids in patients with ad- however, suggest that with a larger sample, dexame- vanced cancer is empirical, as it is in other non- thasone would have been shown to be significantly endocrine indications. -

Robust Extraction, Separation, and Quantitation of Structural Isomer Steroids from Human Plasma by SPE-UHPLC-MS/MS
TECHNICAL NOTE 21882 Robust extraction, separation, and quantitation of structural isomer steroids from human plasma by SPE-UHPLC-MS/MS Authors Application benefits Jon Bardsley1, Kean Woodmansey1, • Separation of structural isomers for accurate detection and Stacy Tremintin2 • Alternative selectivity to C18 phase with an increase in overall resolution of 1Thermo Fisher Scientific, Runcorn, structural isomers UK; 2Thermo Fisher Scientific, Sunnyvale, CA, USA • Stable retention time from extracted plasma • Accurate and precise analytical method across 1000-fold concentration Keywords range Steroid hormone, Vanquish Horizon UHPLC, TSQ Quantiva, Accucore Goal Biphenyl column, LC-MS/MS, SPE Achieve separation of 12 steroid hormones including structural isomers. Comparison to more popular C18 phase is assessed, as well as extraction from human plasma using polymeric solid phase extraction. Introduction Accurate measurement of steroids in plasma is an important requirement in clinical research laboratories. Triple quadrupole mass spectrometry (MS/MS) is now a standard platform in this area for detection due to speed and sensitivity, however this group of compounds contains many structural isomers that cannot be differentiated by MS/MS alone. This may lead to inaccurate analysis by over estimation of concentration levels. Separation prior to MS/MS detection must be achieved, typically by liquid chromatography (LC). An analytical method utilizing LC-MS/MS combined with solid phase extraction of plasma samples is used to remove many matrix interferences, -

Cortisone Acetate Tablets, Usp
CORTISONE ACETATE- cortisone acetate tablet Hikma Pharmaceuticals USA Inc. ---------- CORTISONE ACETATE TABLETS, USP Rev. 07/09 Rx Only DESCRIPTION: Glucocorticoids are adrenocortical steroids, both naturally occurring and synthetic, which are readily absorbed from the gastrointestinal tract. Cortisone acetate is a white or practically white, odorless, crystalline powder. It is stable in air. It is insoluble in water. The molecular weight is 402.49. It is designated chemically as 21-(acetyloxy)-17- hydroxypregn-4-ene-3,11,20-trione. The molecular formula is C23H30O6 and the structural formula is: Cortisone Acetate tablets contain 25 mg of cortisone acetate in each tablet. Inactive ingredients are Anhydrous Lactose, Colloidal Silicon Dioxide, Magnesium Stearate, Microcrystalline Cellulose, Sodium Lauryl Sulfate, and Sodium Starch Glycolate. CLINICAL PHARMACOLOGY: Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. They are also used for their potent anti-inflammatory effects in disorders of many organ systems. Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body's immune responses to diverse stimuli. INDICATIONS AND USAGE: 1. Endocrine Disorders Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the first choice; synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy mineralocorticoid supplementation -

Replacement Therapy for Adrenal Insufficiency
Group 4: Replacement therapy for adrenal insufficiency Frederic Castinetti, Laurence Guignat, Claire Bouvattier, Dinane Samara-Boustani, Yves Reznik To cite this version: Frederic Castinetti, Laurence Guignat, Claire Bouvattier, Dinane Samara-Boustani, Yves Reznik. Group 4: Replacement therapy for adrenal insufficiency . Annales d’Endocrinologie, Elsevier Masson, 2017, 78 (6), pp.525-534. 10.1016/j.ando.2017.10.007. hal-01724179 HAL Id: hal-01724179 https://hal-amu.archives-ouvertes.fr/hal-01724179 Submitted on 10 Apr 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Consensus Group 4: Replacement therapy for adrenal insufficiencyଝ Groupe 4 : traitement substitutif de l’insuffisance surrénale Frédéric Castinettia,∗, Laurence Guignatb, Claire Bouvattierc, Dinane Samara-Boustanid, Yves Reznike,f a UMR7286, CNRS, CRN2M, service d’endocrinologie, hôpital La Conception, Aix Marseille université, AP–HM, 13005 Marseille, France b Service d’endocrinologie et maladies métaboliques, hôpital Cochin, CHU Paris Centre, 75014 Paris, France c Service d’endocrinologie -

Medical Record Requirements for Pre-Service Reviews
Medical Record Requirements for Pre-Service Reviews This document lists medical record requirements for pre-service reviews. These requirements are developed using the clinical criteria in UnitedHealthcare medical policies in conjunction with the guidance provided by UnitedHealthcare physicians and pharmacists with experience in reviewing pre-service requests for coverage. These medical record requirements were developed in an effort to decrease the need for repeated requests for additional information and to improve turnaround time for coverage decisions. Please prepare the suggested materials in advance. We reserve the right to request more information, if necessary. Medical record requirements for case review(s) may vary among various UnitedHealthcare Commercial, UnitedHealthcare Community Plan and UnitedHealthcare Medicare Advantage benefit plans. Please review the requirements for notifications and prior authorization requests at UHCprovider.com/priorauth. These medical record requirements are provided for reference purposes only and may not include all services or codes. Listing of a service or code in this document does not imply that it is a covered or non-covered health service or code. Benefit coverage for health services is determined by the member specific benefit plan document and applicable laws. This document is the property of UnitedHealthcare and unauthorized copying, use or distribution of this information is strictly prohibited. It is regularly reviewed, updated and subject to change. Click a service category from the Table of Contents to jump to the applicable section of this document. Proprietary Information of UnitedHealthcare. Copyright 2020 United HealthCare Services, Inc. Page 1 of 141 Table of Contents Click a service category below to jump to the applicable section of this document. -

Contesting Gender in Popular Culture and Family Law: Middlesex and Other Transgender Tales
Indiana Law Journal Volume 80 Issue 2 Article 4 Spring 2005 Contesting Gender in Popular Culture and Family Law: Middlesex and Other Transgender Tales Susan Frelich Appleton Washington University in St. Louis, [email protected] Follow this and additional works at: https://www.repository.law.indiana.edu/ilj Part of the Family Law Commons, and the Sexuality and the Law Commons Recommended Citation Appleton, Susan Frelich (2005) "Contesting Gender in Popular Culture and Family Law: Middlesex and Other Transgender Tales," Indiana Law Journal: Vol. 80 : Iss. 2 , Article 4. Available at: https://www.repository.law.indiana.edu/ilj/vol80/iss2/4 This Essay is brought to you for free and open access by the Law School Journals at Digital Repository @ Maurer Law. It has been accepted for inclusion in Indiana Law Journal by an authorized editor of Digital Repository @ Maurer Law. For more information, please contact [email protected]. Contesting Gender in Popular Culture and Family Law: Middlesex and Other Transgender Tales SUSAN FRELICH APPLETON* I. CAL AND His COHORT They're everywhere: transsexuals, intersexed individuals, and others of uncertain gender classification. Transgender issues have come out of the closet as popular culture seems to have discovered a new favorite. Recently, several successful books and movies, not to mention frequent television coverage on both talk shows and science programs, have introduced the public to numerous ordinary people whose very existence challenges the notion that sex and gender provide life's fundamental organizing principles. In turn, the law's reliance on strict sex-based categories becomes increasingly fragile, indeed too fragile to withstand challenges to marriage laws requiring a male and a female.