Adrenal Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Frequently Asked Questions for Addison Patients
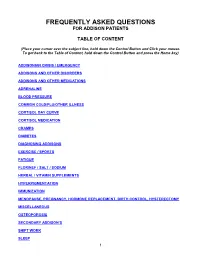
FREQUENTLY ASKED QUESTIONS FOR ADDISON PATIENTS TABLE OF CONTENT (Place your cursor over the subject line, hold down the Control Button and Click your mouse. To get back to the Table of Content, hold down the Control Button and press the Home key) ADDISONIAN CRISIS / EMERGENCY ADDISONS AND OTHER DISORDERS ADDISONS AND OTHER MEDICATIONS ADRENALINE BLOOD PRESSURE COMMON COLD/FLU/OTHER ILLNESS CORTISOL DAY CURVE CORTISOL MEDICATION CRAMPS DIABETES DIAGNOSING ADDISONS EXERCISE / SPORTS FATIGUE FLORINEF / SALT / SODIUM HERBAL / VITAMIN SUPPLEMENTS HYPERPIGMENTATION IMMUNIZATION MENOPAUSE, PREGNANCY, HORMONE REPLACEMENT, BIRTH CONTROL, HYSTERECTOMY MISCELLANEOUS OSTEOPOROSIS SECONDARY ADDISON’S SHIFT WORK SLEEP 1 STRESS DOSING SURGICAL, MEDICAL, DENTAL PROCEDURES THYROID TRAVEL WEIGHT GAIN 2 ADDISONIAN CRISIS / EMERGENCY How do you know when to call an ambulance? If you are careful, you should not have to call an ambulance. If someone with adrenal insufficiency has gastrointestinal problems and is unable to keep down their cortisol or other glucocorticoid for more than 24 hrs, they should be taken to an emergency department so they can be given intravenous solucortef and saline. It is not appropriate to wait until they are so ill that they cannot be taken to the hospital by a family member. If the individual is unable to retain anything by mouth and is very ill, or if they have had a sudden stress such as a fall or an infection, then it would be necessary for them to go by ambulance as soon as possible. It is important that you should have an emergency kit at home and that someone in the household knows how to use it. -

Steroid Use in Prednisone Allergy Abby Shuck, Pharmd Candidate
Steroid Use in Prednisone Allergy Abby Shuck, PharmD candidate 2015 University of Findlay If a patient has an allergy to prednisone and methylprednisolone, what (if any) other corticosteroid can the patient use to avoid an allergic reaction? Corticosteroids very rarely cause allergic reactions in patients that receive them. Since corticosteroids are typically used to treat severe allergic reactions and anaphylaxis, it seems unlikely that these drugs could actually induce an allergic reaction of their own. However, between 0.5-5% of people have reported any sort of reaction to a corticosteroid that they have received.1 Corticosteroids can cause anything from minor skin irritations to full blown anaphylactic shock. Worsening of allergic symptoms during corticosteroid treatment may not always mean that the patient has failed treatment, although it may appear to be so.2,3 There are essentially four classes of corticosteroids: Class A, hydrocortisone-type, Class B, triamcinolone acetonide type, Class C, betamethasone type, and Class D, hydrocortisone-17-butyrate and clobetasone-17-butyrate type. Major* corticosteroids in Class A include cortisone, hydrocortisone, methylprednisolone, prednisolone, and prednisone. Major* corticosteroids in Class B include budesonide, fluocinolone, and triamcinolone. Major* corticosteroids in Class C include beclomethasone and dexamethasone. Finally, major* corticosteroids in Class D include betamethasone, fluticasone, and mometasone.4,5 Class D was later subdivided into Class D1 and D2 depending on the presence or 5,6 absence of a C16 methyl substitution and/or halogenation on C9 of the steroid B-ring. It is often hard to determine what exactly a patient is allergic to if they experience a reaction to a corticosteroid. -

Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Cr
Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Crizotinib (PF-02341066) 1 4 55 Docetaxel 1 5 98 Anastrozole 1 6 25 Cladribine 1 7 23 Methotrexate 1 8 -187 Letrozole 1 9 65 Entecavir Hydrate 1 10 48 Roxadustat (FG-4592) 1 11 19 Imatinib Mesylate (STI571) 1 12 0 Sunitinib Malate 1 13 34 Vismodegib (GDC-0449) 1 14 64 Paclitaxel 1 15 89 Aprepitant 1 16 94 Decitabine 1 17 -79 Bendamustine HCl 1 18 19 Temozolomide 1 19 -111 Nepafenac 1 20 24 Nintedanib (BIBF 1120) 1 21 -43 Lapatinib (GW-572016) Ditosylate 1 22 88 Temsirolimus (CCI-779, NSC 683864) 1 23 96 Belinostat (PXD101) 1 24 46 Capecitabine 1 25 19 Bicalutamide 1 26 83 Dutasteride 1 27 68 Epirubicin HCl 1 28 -59 Tamoxifen 1 29 30 Rufinamide 1 30 96 Afatinib (BIBW2992) 1 31 -54 Lenalidomide (CC-5013) 1 32 19 Vorinostat (SAHA, MK0683) 1 33 38 Rucaparib (AG-014699,PF-01367338) phosphate1 34 14 Lenvatinib (E7080) 1 35 80 Fulvestrant 1 36 76 Melatonin 1 37 15 Etoposide 1 38 -69 Vincristine sulfate 1 39 61 Posaconazole 1 40 97 Bortezomib (PS-341) 1 41 71 Panobinostat (LBH589) 1 42 41 Entinostat (MS-275) 1 43 26 Cabozantinib (XL184, BMS-907351) 1 44 79 Valproic acid sodium salt (Sodium valproate) 1 45 7 Raltitrexed 1 46 39 Bisoprolol fumarate 1 47 -23 Raloxifene HCl 1 48 97 Agomelatine 1 49 35 Prasugrel 1 50 -24 Bosutinib (SKI-606) 1 51 85 Nilotinib (AMN-107) 1 52 99 Enzastaurin (LY317615) 1 53 -12 Everolimus (RAD001) 1 54 94 Regorafenib (BAY 73-4506) 1 55 24 Thalidomide 1 56 40 Tivozanib (AV-951) 1 57 86 Fludarabine -

Corticosteroids in Terminal Cancer-A Prospective Analysis of Current Practice
Postgraduate Medical Journal (November 1983) 59, 702-706 Postgrad Med J: first published as 10.1136/pgmj.59.697.702 on 1 November 1983. Downloaded from Corticosteroids in terminal cancer-a prospective analysis of current practice G. W. HANKS* T. TRUEMAN B.Sc., M.B., B.S., M.R.C.P.(U.K.) S.R.N. R. G. TWYCROSS M.A., D.M., F.R.C.P. Sir Michael Sobell House, The Churchill Hospital, Headington, Oxford OX3 7LJ Summary Introduction Over half of a group of 373 inpatients with advanced Corticosteroids have a major role to play in the malignant disease were treated with corticosteroids control of symptoms in patients with advanced for a variety of reasons. They received either pred- malignant disease. They may be employed in a non- nisolone or dexamethasone, or replacement therapy specific way to improve mood and appetite; or they with cortisone acetate. Forty percent of those receiv- may be indicated as specific adjunctive therapy in the ing corticosteroids benefited from them. A higher relief of symptoms related to a large tumour mass or response rate was seen when corticosteroids were to nerve compression. The management of a numberProtected by copyright. prescribed for nerve compression pain, for raised of other symptoms and syndromes may also be intracranial pressure, and when used in conjunction facilitated by treatment with corticosteroids (Table with chemotherapy. No significant difference in 1). efficacy was noted between the 2 drugs. The results, The use of corticosteroids in patients with ad- however, suggest that with a larger sample, dexame- vanced cancer is empirical, as it is in other non- thasone would have been shown to be significantly endocrine indications. -

Cortisone Acetate Tablets, Usp
CORTISONE ACETATE- cortisone acetate tablet Hikma Pharmaceuticals USA Inc. ---------- CORTISONE ACETATE TABLETS, USP Rev. 07/09 Rx Only DESCRIPTION: Glucocorticoids are adrenocortical steroids, both naturally occurring and synthetic, which are readily absorbed from the gastrointestinal tract. Cortisone acetate is a white or practically white, odorless, crystalline powder. It is stable in air. It is insoluble in water. The molecular weight is 402.49. It is designated chemically as 21-(acetyloxy)-17- hydroxypregn-4-ene-3,11,20-trione. The molecular formula is C23H30O6 and the structural formula is: Cortisone Acetate tablets contain 25 mg of cortisone acetate in each tablet. Inactive ingredients are Anhydrous Lactose, Colloidal Silicon Dioxide, Magnesium Stearate, Microcrystalline Cellulose, Sodium Lauryl Sulfate, and Sodium Starch Glycolate. CLINICAL PHARMACOLOGY: Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. They are also used for their potent anti-inflammatory effects in disorders of many organ systems. Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body's immune responses to diverse stimuli. INDICATIONS AND USAGE: 1. Endocrine Disorders Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the first choice; synthetic analogs may be used in conjunction with mineralocorticoids where applicable; in infancy mineralocorticoid supplementation -

Replacement Therapy for Adrenal Insufficiency
Group 4: Replacement therapy for adrenal insufficiency Frederic Castinetti, Laurence Guignat, Claire Bouvattier, Dinane Samara-Boustani, Yves Reznik To cite this version: Frederic Castinetti, Laurence Guignat, Claire Bouvattier, Dinane Samara-Boustani, Yves Reznik. Group 4: Replacement therapy for adrenal insufficiency . Annales d’Endocrinologie, Elsevier Masson, 2017, 78 (6), pp.525-534. 10.1016/j.ando.2017.10.007. hal-01724179 HAL Id: hal-01724179 https://hal-amu.archives-ouvertes.fr/hal-01724179 Submitted on 10 Apr 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Consensus Group 4: Replacement therapy for adrenal insufficiencyଝ Groupe 4 : traitement substitutif de l’insuffisance surrénale Frédéric Castinettia,∗, Laurence Guignatb, Claire Bouvattierc, Dinane Samara-Boustanid, Yves Reznike,f a UMR7286, CNRS, CRN2M, service d’endocrinologie, hôpital La Conception, Aix Marseille université, AP–HM, 13005 Marseille, France b Service d’endocrinologie et maladies métaboliques, hôpital Cochin, CHU Paris Centre, 75014 Paris, France c Service d’endocrinologie -

21 CFR Ch. I (4–1–01 Edition)
§ 524.86 21 CFR Ch. I (4–1–01 Edition) 524.1044b Gentamicin sulfate, 524.1600 Nystatin ophthalmic and topical betamethasone valerate otic solution. dosage forms. 524.1044c Gentamicin ophthalmic ointment. 524.1600a Nystatin, neomycin, thiostrepton, 524.1044d Gentamicin sulfate, and triamcinolone acetonide ointment. betamethasone valerate ointment. 524.1600b Nystatin, neomycin, thiostrepton, 524.1044e Gentamicin sulfate spray. and triamcinolone acetonide ophthalmic 524.1044f Gentamicin sulfate, ointment. betamethasone valerate topical spray. 524.1662 Oxytetracycline hydrochloride oph- 524.1044g Gentamicin sulfate, thalmic and topical dosage forms. betamethasone valerate, clotrimazole 524.1662a Oxytetracycline hydrochloride and ointment. hydrocortisone spray. 524.1044h Gentamicin sulfate, mometasone 524.1662b Oxytetracycline hydrochloride, furoate, clotrimazole otic suspension. polymyxin B sulfate ophthalmic oint- 524.1193 Ivermectin pour-on. ment. 524.1195 Ivermectin otic suspension. 524.1742 N-(Mercaptomethyl) phthalimide S- 524.1200 Kanamycin ophthalmic and topical (O,O-dimethyl phosphorodithioate) emul- dosage forms. sifiable liquid. 524.1200a Kanamycin ophthalmic ointment. 524.1880 Prednisolone-neomycin sulfate oph- 524.1200b Kanamycin ophthalmic aqueous thalmic ointment. solution. 524.1881 Prednisolone acetate ophthalmic 524.1204 Kanamycin sulfate, calcium and topical dosage forms. amphomycin, and hydrocortisone ace- 524.1881a [Reserved] tate. 524.1240 Levamisole. 524.1881b Prednisolone acetate-neomycin 524.1376 2-Mercaptobenzothiazole solution. sulfate sterile suspension. 524.1443 Miconazole nitrate cream; 524.1883 Prednisolone sodium phosphate-ne- miconazole nitrate lotion; miconazole ni- omycin sulfate ophthalmic ointment. trate spray. 524.1982 Proparacaine hydrochloride oph- 524.1446 Milbemycin oxime solution. thalmic solution. 524.1451 Moxidectin. 524.2098 Selamectin. 524.1465 Mupirocin ointment. 524.2101 Selenium disulfide suspension. 524.1484 Neomycin sulfate ophthalmic and 524.2140 Squalane, pyrethrins and piperonyl topical dosage forms. -

Pharmacologic Characteristics of Corticosteroids 대한신경집중치료학회
REVIEW J Neurocrit Care 2017;10(2):53-59 https://doi.org/10.18700/jnc.170035 eISSN 2508-1349 Pharmacologic Characteristics of Corticosteroids 대한신경집중치료학회 Sophie Samuel, PharmD1, Thuy Nguyen, PharmD1, H. Alex Choi, MD2 1Department of Pharmacy, Memorial Hermann Texas Medical Center, Houston, TX; 2Department of Neurosurgery and Neurology, The University of Texas Medical School at Houston, Houston, TX, USA Corticosteroids (CSs) are used frequently in the neurocritical care unit mainly for their anti- Received December 7, 2017 inflammatory and immunosuppressive effects. Despite their broad use, limited evidence Revised December 7, 2017 exists for their efficacy in diseases confronted in the neurocritical care setting. There are Accepted December 17, 2017 considerable safety concerns associated with administering these drugs and should be limited Corresponding Author: to specific conditions in which their benefits outweigh the risks. The application of CSs in H. Alex Choi, MD neurologic diseases, range from traumatic head and spinal cord injuries to central nervous Department of Pharmacy, Memorial system infections. Based on animal studies, it is speculated that the benefit of CSs therapy Hermann Texas Medical Center, 6411 in brain and spinal cord, include neuroprotection from free radicals, specifically when given Fannin Street, Houston, TX 77030, at a higher supraphysiologic doses. Regardless of these advantages and promising results in USA animal studies, clinical trials have failed to show a significant benefit of CSs administration Tel: +1-713-500-6128 on neurologic outcomes or mortality in patients with head and acute spinal injuries. This Fax: +1-713-500-0665 article reviews various chemical structures between natural and synthetic steroids, discuss its E-mail: [email protected] pharmacokinetic and pharmacodynamic profiles, and describe their use in clinical practice. -

Conversion of Cortisone to Cortisol and Prednisone to Prednisolone
22 April 1967 Histocompatibility Tests-Johnson and Russell MEBRITJSH 205 Bach, F., and Hirschhorn, K. (1964). Science, 143, 813. Harris, R., Clarke, C. A., Jones, A. L., Sheppard, P. M., Lehane, D., Bain, B., and Lowenstein, L. (1964). Ibid., 145, 1315. McCarthy, M., Lawler, S. D., and Shatwell, H. S. (1966). Brit. Vas, M. R., and Lowenstein, L. (1964). Blood, 23, 108. med. 7., 1, 509. Brent, L., and Medawar, P. B. (1963). Brit. med. 7., 2, 269. Hirschhorn, K. (1965). In Histocompatibility Testing, edited by P. S. - (1964). Nature (Lond.), 204, 90. Russell and H. J. Winn, Publication No. 1229, Nat. Acad. Sci., Bridges, J. M., Nelson, S. D., and McGeown, M. G. (1964). Lancet, 1, Washington, p. 177. 581. Huggins, C. E. (1964). Ann. Surg., 160, 643. Chen, P. S. (1958). Proc. Soc. exp. Biol. (N.Y.), 98, 546. Johnson, G. J., and Russell, P. S. (1965). Nature (Lond.), 208, 343. Gray, J. G., and Russell, P. S. (1963). Lancet, 2, 863. Moorhead, J. F., and Patel, A. R. (1964). Brit. med. 7., 2, 1111. - (1965). In Histocompatibility Testing, edited by P. S. Russell Russell, P. S. (1966). In Histocompatibility Testing 1965, edited by HE and H. J. Winn. Publication No. 1229, Nat. Acad. Sci., Washington, Balner, F. J. Cleton, and J. G. Eernissc, p. 233. Copenhagen. p. 105. Streilein, J. W. (1966). Ibid., p. 241. Conversion of Cortisone to Cortisol and Prednisone to Prednisolone J. S. JENKINS,* M.D., M.R.C.P.; P. A. SAMPSON,t M.B., CH.B. Brit. med. J., 1967, 2, 205-207 Though cortisone has been widely used since Hench et al. -

Recent Advances in the Analysis of Steroid Hormones and Related Drugs
ANALYTICAL SCIENCES MAY 2004, VOL. 20 767 2004 © The Japan Society for Analytical Chemistry Reviews Recent Advances in the Analysis of Steroid Hormones and Related Drugs Sándor GÖRÖG Gedeon Richter Ltd., P.O.B. 27, H-1475 Budapest, Hungary The development during the last 15 years and the state-of-the-art in the analysis of bulk steroid hormone drugs and hormone-like structures and pharmaceutical formulations made thereof are summarized. Other steroids (sterols, bile acids, cardiac glycosides, vitamins D) as well as biological-clinical aspects and pharmacokinetic and metabolic studies are excluded from this review. The state-of-the-art is summarized based on comparisons of monographs in the latest editions of the European Pharmacopoeia, United States Pharmacopoeia and the Japanese Pharmacopoeia. This is followed by sections dealing with new developments in the methodology for the fields of spectroscopic and spectrophotometric, chromatographic, electrophoretic and hyphenated techniques as well electroanalytical methods. The review is terminated by two problem-oriented sections: examples on impurity and degradation profiling as well as enantiomeric analysis. (Received January 14, 2004; Accepted February 2, 2004) 1 Introduction 767 4·3 Supercritical fluid chromatography (SFC) 2 Steroid Hormone Drugs in Pharmacopoeias 768 4·4 High-performance liquid chromatography 2·1 Assay of bulk drug materials (HPLC) and HPLC-MS 2·2 Related impurities test of bulk drug materials 5 Electrophoretic and Related Methods 776 2·3 Assay of steroid hormone formulations -

Prednisone in Rheumatoid Arthritis: Metabolic and Clinical Effects
Ann Rheum Dis: first published as 10.1136/ard.17.2.145 on 1 June 1958. Downloaded from Ann. rheum. Dis. (1958), 17, 145. PREDNISONE IN RHEUMATOID ARTHRITIS: METABOLIC AND CLINICAL EFFECTS BY L. EMMERSON WARD, HOWARD F. POLLEY, MARSCHELLE H. POWER, HAROLD L. MASON, CHARLES H. SLOCUMB, AND PHILIP S. HENCH Mayo Clinic and Mayo Foundation,* Rochester, Minn. The initial reports (Hench, Kendall, Slocumb, and strated that chemists could alter the steroid molecule Polley, 1949; Sprague, Power, Mason, Albert, so as to prepare synthetic compounds with even Mathieson, Hench, Kendall, Slocumb, and Polley, more selective effects. This paved the way for the 1950; Hench and others, 1950) of the antirheumatic dissociation of one effect from another, so that one potency of cortisone emphasized the fact that or more of these effects could be enhanced rela- excessive doses produced not only desirable but also tively. certain undesirable effects. At that time (1949), we The chemical structure of prednisone (delta expressed our hope and belief that analogues 1-cortisone) and prednisolone (delta I-hydro- superior to cortisone would be discovered. Since cortisone) differs from that of cortisone and hydro- then, at least seven more cortisone-like steroids have cortisone, respectively, only in the possession of a copyright. been found useful clinically; these include hydro- double bond (hence the designation "delta") between cortisone, 9-alpha-fluorohydrocortisone (Fludro- the first and second carbon atoms in ring A of the cortisone), prednisone, prednisolone, a compound molecule (Fig. 1, overleaf). It is this slight change whose structure is 9-alpha-fluoro, delta 1-hydro- that invests these synthetic cortisone-like steroids cortisone, and the two most recent additions, with an increased antirheumatic potency and a de- namely triamcinolone and 6-methyl, delta I-hydro- creased effect on the metabolism ofelectrolytes when cortisone. -

PDL)/Non-Preferred Drug List (NPDL
Louisiana Medicaid Preferred Drug List (PDL)/Non-Preferred Drug List (NPDL) • The PDL is a list of over 100 therapeutic classes reviewed by the Pharmaceutical & Therapeutics (P&T) committee. In addition, there are medications and/or classes of medications that are not reviewed by the committee. Unless there is a clinical pre-authorization requirement for the entire class (as noted on the last page of the PDL) these medications will continue to be covered without prior authorization. Examples: spironolactone, hydrochlorothiazide, amoxicillin suspension • To locate any medication on this list, you may use the keyboard shortcut CTRL + F to search. • There is a mandatory generic substitution unless the brand is preferred, and the generic is non-preferred. When the brand is preferred and the generic is non-preferred, no special notations are required by the prescriber and the pharmacist enters “9” in the DAW field 408-D8. • When the brand is non-preferred and the prescriber has determined it to be medically necessary, “Brand medically necessary” or “Brand necessary” must be written on the prescription in the prescriber’s handwriting or via an electronic prescription and the pharmacist enters “1” in the DAW field 408-D8. For more information, please CLICK THIS LINK to the provider manual. • New medications that enter the marketplace in classes reviewed by P&T committee will be considered non-preferred requiring prior authorization until the next P&T committee meeting. Please refer to the following criteria: New Drugs Introduced into the Market / Non-Preferred • Medications listed as non-preferred are available through the prior authorization process.