4-Hydroxynonenal, an Endogenous Aldehyde, Causes Pain and Neurogenic Inflammation Through Activation of the Irritant Receptor TRPA1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Allicin Protects Against Lipopolysaccharide-Induced Acute Lung Injury by Up-Regulation of Claudin-4
Zheng et al Tropical Journal of Pharmaceutical Research July 2014; 13 (7): 1063-1069 ISSN: 1596-5996 (print); 1596-9827 (electronic) © Pharmacotherapy Group, Faculty of Pharmacy, University of Benin, Benin City, 300001 Nigeria. All rights reserved. Available online at http://www.tjpr.org http://dx.doi.org/10.4314/tjpr.v13i7.8 Original Research Article Allicin Protects against Lipopolysaccharide-Induced Acute Lung Injury by Up-Regulation of Claudin-4 Yue-liang Zheng, Wen-wei Cai, Guang-zhao Yan, Yuan-zhan Xu and Mei-qi Zhang* Department of Emergency, Zhejiang Provincial People's Hospital, Hangzhou 310014, China *For correspondence: Email: [email protected]; Tel: +86-0571-85893631 Received: 8 January 2014 Revised accepted: 31 May 2014 Abstract Purpose: To investigate the effect of allicin, an active component of garlic, on lipopolysaccharide (LPS)- induced acute lung injury. Methods: Wistar rats were subjected to LPS intravenous injection with or without allicin treatment to induce acute lung injury (ALI) model. Also, A549 cells were stimulated with LPS in the presence and absence of allicin. HE staining was used to detect pathological changes in lung tissues. Enzyme-linked immunosorbent assay (ELISA) was performed to measure cytokine content. Cell viability was measured by CCK-8 and EdU incorporation assay. Genes expression was determined by real time polymerase chain reaction (PCR) and Western blot. Flow cytometry was applied to measure cell apoptosis. Results: In vivo data showed that pulmonary edema, inflammatory cytokines expression and pathological changes were significantly attenuated in LPS-induced ALI after treatment with allicin (p < 0.05) while in vitro results indicate that allicin administration significantly improved the A549 cell viability in a dose-dependent manner as measured by CCK-8 and EdU incorporation assay. -

World Journal of Pharmaceutical Research Anjna Et Al
World Journal of Pharmaceutical Research Anjna et al. World Journal of PharmaceuticalSJIF ImpactResearch Factor 8.074 Volume 8, Issue 10, 741-748. Research Article ISSN 2277– 7105 A PHYTOCHEMICAL STUDY OF ALLIUM SATIVUM – W.S.R TO ALLICIN CONTENT 1*Tak Anjna, 2Thakur Kumar Sudarshan and 3Das Kumar Arun 1Associate Professor, Prasuti Tantra Avum Stri Roga, Main Campus, Uttrakhanda Ayurveda University, Dehradun, Uttarakhanda. 2Lecturer, Ras Shashtra Avum Bhaishajya Kalpana, R.G.G.P.G. Ayurvedic College, Paprola, Himachal Pradesh. 3Principal, Professor & H.O.D, Ras Shashtra Avum Bhaishajya Kalpana, Govt. Ayurvedic College, Bolangir, Orisa. ABSTRACT Article Received on 15 July 2019, Allium sativum has attracted the interest of many researchers due to its Revised on 05 August 2019, wide range of therapeutic effects with minimal adverse reactions. Its Accepted on 25 August 2019, DOI: 10.20959/wjpr201910-15253 role in promoting the female reproductive health can be well understood from the fact Acharya Kashyap in his text has described a full chapter Lashuna Kalpadhyaya mentioning that the woman *Corresponding Author Tak Anjna consuming Lashuna will not suffer from diseases of kati, shroni Associate Professor, Prasuti (pelvis), gramyadharma janya rogas (sexually transmitted diseases) Tantra Avum Stri Roga, and infertility. Its effects are mainly attributed to its chemical Main Campus, Uttrakhanda constituents like Allicin, Ajoene and certain other sulphur compounds Ayurveda University, etc. In the present study, bulbs of Allium sativum were dried and in Dehradun, Uttarakhanda. controlled temperature and fine powder was made. It was filled in capsules and clinical trial was done in the patients of Hypomenorrhoea. In context of this, a phytochemical study of dried powder of Allium sativum was done and various chemical constituents of garlic have been investigated to support its pharmaco-therapeutic actions as per clinical study. -

Allicin Induces Apoptosis Through Activation of Both Intrinsic and Extrinsic Pathways in Glioma Cells
5976 MOLECULAR MEDICINE REPORTS 17: 5976-5981, 2018 Allicin induces apoptosis through activation of both intrinsic and extrinsic pathways in glioma cells CHENLONG LI1, HANGUANG JING2, GUANGTAO MA3 and PENG LIANG1 1Department of Neurosurgery, Harbin Medical University Cancer Hospital, Harbin, Heilongjiang 150086; 2Basic Theory of Chinese Medicine, Preclinical Medicine School, Beijing University of Chinese Medicine, Beijing 100029; 3Department of Neurosurgery, Daqing Oil Field General Hospital, Daqing, Heilongjiang 163000, P.R. China Received August 12, 2016; Accepted January 4, 2018 DOI: 10.3892/mmr.2018.8552 Abstract. Allicin is an extract purified fromAllium sativum apoptotic cascades. These results implicate Allicin as a (garlic), and previous research has indicated that Allicin novel antitumor agent in treating glioma. has an inhibitory effect on many kinds of tumor cells. The aim of the present study was to explore the anticancer Introduction activity of Allicin on human glioma cells and investigate the underlying mechanism. MTT and colony‑formation Glioblastoma (GBM) is the most aggressive subset of assays were performed to detect glioma cell prolifera- primary brain tumor in adults, and is responsible for ~50% tion, and explore the effect of Allicin at various doses and of all cranial tumors. GBMs are highly infiltrative which time‑points. The apoptosis of glioma cells was measured results in difficulty for them to be resected completely (1-3). by fluorescence microscopy with Hoechst 33258 staining, Comprehensive therapy including radiotherapy and chemo- and then flow cytometry was used to analyzed changes in therapy is the main approach used for treatment; however, glioma cell apoptosis. Reverse transcription‑quantitative the overall survival of glioma patients is only 12‑14 months polymerase chain reaction and western blot analysis were post‑diagnosis (4). -

Garlic and Onions: Their Cancer Prevention Properties Holly L
Published OnlineFirst January 13, 2015; DOI: 10.1158/1940-6207.CAPR-14-0172 Review Cancer Prevention Research Garlic and Onions: Their Cancer Prevention Properties Holly L. Nicastro1, Sharon A. Ross2, and John A. Milner3,† Abstract The Allium genus includes garlic, onions, shallots, leeks, and potential mechanisms of individual sulfur-containing com- chives. These vegetables are popular in cuisines worldwide and pounds and of various preparations and extracts of these are valued for their potential medicinal properties. Epidemio- vegetables, including decreased bioactivation of carcinogens, logic studies, while limited in their abilities to assess Allium antimicrobial activities, and redox modification. Allium vege- consumption, indicate some associations of Allium vegetable tables and their components have effects at each stage of consumption with decreased risk of cancer, particularly cancers carcinogenesis and affect many biologic processes that modify of the gastrointestinal tract. Limited intervention studies have cancer risk. This review discusses the cancer-preventive effects of been conducted to support these associations. The majority of Allium vegetables, particularly garlic and onions, and their supportive evidence on Allium vegetables cancer-preventive bioactive sulfur compounds and highlights research gaps. effects comes from mechanistic studies. These studies highlight Cancer Prev Res; 8(3); 181–9. Ó2015 AACR. Introduction group of foods that has raised considerable interest for their putative cancer-preventive properties is the Allium genus. Increasingly governmental entities and other organizations are Allium is the Latin word for garlic. It is part of a monocot genus proposing a wide range of food policies to promote health. These of flowering plants frequently referred to as the onion genus. -

Spice Basics
SSpicepice BasicsBasics AAllspicellspice Allspice has a pleasantly warm, fragrant aroma. The name refl ects the pungent taste, which resembles a peppery compound of cloves, cinnamon and nutmeg or mace. Good with eggplant, most fruit, pumpkins and other squashes, sweet potatoes and other root vegetables. Combines well with chili, cloves, coriander, garlic, ginger, mace, mustard, pepper, rosemary and thyme. AAnisenise The aroma and taste of the seeds are sweet, licorice like, warm, and fruity, but Indian anise can have the same fragrant, sweet, licorice notes, with mild peppery undertones. The seeds are more subtly fl avored than fennel or star anise. Good with apples, chestnuts, fi gs, fi sh and seafood, nuts, pumpkin and root vegetables. Combines well with allspice, cardamom, cinnamon, cloves, cumin, fennel, garlic, nutmeg, pepper and star anise. BBasilasil Sweet basil has a complex sweet, spicy aroma with notes of clove and anise. The fl avor is warming, peppery and clove-like with underlying mint and anise tones. Essential to pesto and pistou. Good with corn, cream cheese, eggplant, eggs, lemon, mozzarella, cheese, olives, pasta, peas, pizza, potatoes, rice, tomatoes, white beans and zucchini. Combines well with capers, chives, cilantro, garlic, marjoram, oregano, mint, parsley, rosemary and thyme. BBayay LLeafeaf Bay has a sweet, balsamic aroma with notes of nutmeg and camphor and a cooling astringency. Fresh leaves are slightly bitter, but the bitterness fades if you keep them for a day or two. Fully dried leaves have a potent fl avor and are best when dried only recently. Good with beef, chestnuts, chicken, citrus fruits, fi sh, game, lamb, lentils, rice, tomatoes, white beans. -

Chapter 4 Antimicrobial Properties of Organosulfur Compounds
Chapter 4 Antimicrobial Properties of Organosulfur Compounds Osman Sagdic and Fatih Tornuk Abstract Organosulfur compounds are defi ned as organic molecules containing one or more carbon-sulfur bonds. These compounds are present particularly in Allium and Brassica vegetables and are converted to a variety of other sulfur con- taining compounds via hydrolysis by several herbal enzymes when the intact bulbs are damaged or cut. Sulfur containing hydrolysis products constitute very diverse chemical structures and exhibit several bioactive properties as well as antimicrobial. The antimicrobial activity of organosulfur compounds has been reported against a wide spectrum of bacteria, fungi and viruses. Despite the wide antimicrobial spec- trum, their pungent fl avor/odor is the most considerable factor restricting their com- mon use in foods as antimicrobial additives. However, meat products might be considered as the most suitable food materials in this respect since Allium and Brassica vegetables especially garlic and onion have been used as fl avoring and preservative agents in meat origin foods. In this chapter, the chemical diversity and in vitro and in food antimicrobial activity of the organosulfur compounds of Allium and Brassica plants are summarized. Keywords Organosulfur compounds • Garlic • Onion • Allium • Brassica • Thiosulfi nates • Glucosinolates O. Sagdic (*) Department of Food Engineering, Faculty of Chemical and Metallurgical Engineering , Yildiz Teknik University , 34220 Esenler , Istanbul , Turkey e-mail: [email protected] F. Tornuk S a fi ye Cikrikcioglu Vocational College , Erciyes University , 38039 Kayseri , Turkey A.K. Patra (ed.), Dietary Phytochemicals and Microbes, 127 DOI 10.1007/978-94-007-3926-0_4, © Springer Science+Business Media Dordrecht 2012 128 O. -
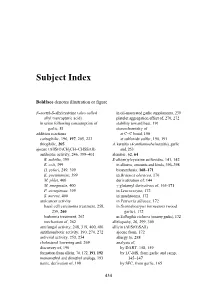
Subject Index
Subject Index Boldface denotes illustration or figure N-acetyl-S-allylcysteine (also called in oil-macerated garlic supplements, 239 allyl mercapturic acid) platelet aggregation effect of, 270, 272 in urine following consumption of stability toward heat, 191 garlic, 81 stereochemistry of addition reactions at C=C bond, 190 carbophilic, 196, 197, 205, 223 at sulfoxide sulfur, 190, 191 thiophilic, 205 A. keratitis (Acanthamoeba keratitis), garlic ajoene (AllS(O)CH2CH=CHSSAll) and, 253 antibiotic activity, 246, 399–401 alembic, 62, 64 B. subtilis, 399 S-alk(en)ylcysteine sulfoxides, 141, 142 E. coli, 399 in alliums, amounts and kinds, 396–398 H. pylori, 249, 399 biosynthesis, 168–171 K. pneumoniae, 399 in Brassica oleracea, 170 M. phlei, 400 derivatization of, 144 M. smegmatis, 400 γ-glutamyl derivatives of, 165-171 P. aeruginosa, 399 in Leucocoryne, 172 S. aureus, 400 in mushrooms, 172 anticancer activity in Petiveria alliacea, 172 basal cell carcinoma treatment, 258, in Scorodocarpus borneensis (wood 259, 260 garlic), 172 leukemia treatment, 262 in Tulbaghia violacea (society garlic), 172 mechanism of, 262 allelopathy, 26, 299, 300 antifungal activity, 248, 319, 400, 401 allicin (AllS(O)SAll) antithrombotic activity, 190, 270, 272 ajoene from, 172 antiviral activity, 253, 254 allergy to, 288 cholesterol lowering and, 269 analysis of, discovery of, 190 by DART, 158, 159 formation from allicin, 70, 172, 191, 192 by LC-MS, from garlic and ramp, monomethyl and dimethyl analogs, 193 145–147 name, derivation of, 190 by SFC, from garlic, 165 434 Subject Index 435 antibiotic activity of, 69, 72, 244, 318, thioacrolein from, 155 319, 399–401 3-vinyl-4H-1,2-dithiin and 2-vinyl- E. -

The Human Allicin-Proteome S-Thioallylation of Proteins by The
Free Radical Biology and Medicine 131 (2019) 144–153 Contents lists available at ScienceDirect Free Radical Biology and Medicine journal homepage: www.elsevier.com/locate/freeradbiomed Original article The human allicin-proteome: S-thioallylation of proteins by the garlic T defence substance allicin and its biological effects ⁎ Martin C.H. Gruhlkea, ,1, Haike Antelmannb,1, Jörg Bernhardtc, Veronika Kloubertd, Lothar Rinkd, Alan J. Slusarenkoa a Department of Plant Physiology, RWTH Aachen University, Worringer Weg 1, D-52056 Aachen, Germany b Freie Universität Berlin, Institute of Biology-Microbiology, Königin-Luise-Str. 12-16, D-14195 Berlin, Germany c Institute of Microbiology, University of Greifswald, Felix-Hausdorff-Straße 8, D-17489 Greifswald, Germany d Institute of Immunology, RWTH Aachen University Hospital, Pauwelsstraße 30, D-52074 Aachen, Germany ARTICLE INFO ABSTRACT Keywords: A single clove of edible garlic (Allium sativum L.) of about 10 g produces up to 5 mg of allicin (diallylthiosulfi- Allicin nate), a thiol-reactive sulfur-containing defence substance that gives injured garlic tissue its characteristic smell. S-thioallylation Allicin induces apoptosis or necrosis in a dose-dependent manner but biocompatible doses influence cellular Protein modification metabolism and signalling cascades. Oxidation of protein thiols and depletion of the glutathione pool are Cysteine thought to be responsible for allicin's physiological effects. Here, we studied the effect of allicin on post-trans- Cytoskeleton lational thiol-modification in human Jurkat T-cells using shotgun LC-MS/MS analyses. We identified 332pro- Actin Glycolysis teins that were modified by S-thioallylation in the Jurkat cell proteome which causes a mass shift of 72 Da on Warburg effect cysteines. -

Garlic – “The Stinking Rose”, “Plant Talisman”, “Camphor of the Poor” Same – S-Adenosyl L- Methionine
Supplement Sampler Garlic – “The Stinking Rose”, “Plant Talisman”, “Camphor of the Poor” SAMe – S-adenosyl L- methionine Best Indications Common cold: reducing incidence and duration.1 Hypertension: drop in systolic (SBP) and diastolic blood pressure (DBP) seen in hypertensive patients.2 Topical ringworm, athlete’s foot, and jock itch: topical application of garlic (in gel or paste form) may help treat dermatophytosis.3 Atherosclerosis: although current evidence suggests that it does not correct hyperlipidemia in humans, garlic has been shown to reduce progression of atherosclerosis via uncertain mechanisms in animal models.4-6 Background Garlic’s scientific name is Allium Sativum. Garlic has been referred to for various treatments in ancient medical texts from Egypt, Rome, China, India, and ancient Sumerians.7,8 Ancient Greek Olympic athletes ate garlic for an athletic boost.7,8 Mechanism of Action Hypertension: current research shows that garlic activates constitutive nitric oxide synthase, thus causing vasodilation and reduction of blood pressure.2 Dermatophytosis and common cold: an organosulfur component found in garlic, ajoene, has been found to have many antimicrobial and antifungal properties, including quorum sensing inhibition and antioxidant action.8,9 Best Studies One study assessed 146 participants over a 3-month period, with half of the participants taking a placebo tablet, and half taking garlic (one capsule containing 180 mg allicin powder per day), noting cold-like symptoms during this period.1 There were 24 occurrences of the common cold in the garlic group, versus 65 in the placebo group (P-value < 0.001), resulting in fewer days of illness in the garlic group compared with the placebo group (111 versus 366). -

Evaluation of Allicin Stability in Processed Garlic of Different Cultivars
Food Science and Technology ISSN 0101-2061 DDOI http://dx.doi.org/10.1590/1678-457X.6397 Evaluation of allicin stability in processed garlic of different cultivars Patricia PRATI1*, Celina Maria HENRIQUE1, Aparecida Sônia de SOUZA2, Vera Sônia Nunes da SILVA2, Maria Teresa Bertoldo PACHECO2 Abstract This research aimed at evaluating the suitability of five different garlic cultivars for the processing of unsalted garlic paste, chopped fried garlic, and fried sliced garlic. The concentration of allicin in the products was evaluated immediately after processing and at 45-day intervals during 180 days of storage. Allicin concentrations in raw garlic of the varieties under study differed (20.73 a 24.31mg of allicin g–1 garlic). Stability exhibited a similar between the varieties according to the type of processing utilized. Processing into paste was more favorable to the preservation of allicin than the other processes. The amount of allicin lost during the process to obtain paste for the different varieties was less than 9.5%, and it reached a maximum loss of 22% for the commercial varieties during storage (180 days). All fried garlic samples showed a decrease by 99% in the content of allicin right after processing. The processing of garlic in the form of acidified paste preserved its bioactive characteristics during storage. Keywords: bioactive compounds; allicin stability; Allium sativum L.; garlic fried; garlic paste. 1 Introduction Garlic (Allium sativum L.) occupies a prominent position Although considered non-nutritive, the compounds formed among human foods, not only as a condiment, but also due from the decomposition of alliin play an important role in the to its therapeutic properties, attributed to the presence of diet as antioxidants, protecting against certain degenerative bioactive compounds (Tepe et al., 2005). -

Allium Ursinum and Allium Sativum
PHARMACEUTICAL AND CHEMICAL ANALYSIS OF THE COMPONENTS CARRYING THE ANTIPLATELET ACTIVITY OF EXTRACTS FROM ALLIUM URSINUM AND ALLIUM SATIVUM Dissertation zur Erlangung des akademischen Grades Dr.rer.med. an der Medizinischen Fakultät der Universität Leipzig eingereicht von: Dina Talat Tawfiq Sabha geboren am 18.08.1979 in Amman/ Jordanien angefertigt in der Klinik für Herzchirurgie, Universität Leipzig (Direktor:Prof. Dr. Friedrich-Wilhelm Mohr) Betreuer: Prof. Dr. Stefan Dhein i Bibliographische Beschreibung: Titel: Pharmazeutische und chemische Analyse der Inhaltsstoffe von Allium ursinum und Allium sativum, die für die Thrombozytenaggregations- hemmende Wirkung verantworlich sind. (englischer Original-Titel: Pharmaceutical and chemical analysis of the components carrying the antiplatelet activity of extracts from Allium ursinum and Allium sativum) -2011. 126 Seiten. Leipzig, Medizinische Fakultät der Universität Leipzig, Klinik für Herzchirurgie, Dissertation, 2011. Autor: Sabha, Dina Talat Tawfiq 126 S., 102 Lit., 9 Tabellen, 55 Abbildungen ii Contents 1. Introduction: ...................................................................................................................... 1 1.1 Historical background.................................................................................................. 1 1.2 Antiplatelets drugs: Types and side effects ................................................................. 2 1.3 Need for new approach............................................................................................... -

WO 2012/143403 Al 26 October 2012 (26.10.2012) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2012/143403 Al 26 October 2012 (26.10.2012) P O P C T (51) International Patent Classification: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, A23L 1/30 (2006.01) A23L 1/305 (2006.01) DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, A61K 31/19 (2006.01) HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, (21) International Application Number: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, PCT/EP2012/057093 OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, (22) International Filing Date: SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, 18 April 2012 (18.04.2012) TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (26) Publication Language: English GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, (30) Priority Data: UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, 61/476,345 18 April 201 1 (18.04.201 1) US TJ, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, EE, ES, FI, FR, GB, GR, HR, HU, IE, IS, IT, LT, LU, (71) Applicant (for all designated States except US) : NESTEC LV, MC, MK, MT, NL, NO, PL, PT, RO, RS, SE, SI, SK, S.A.