OVERVIEW of COAGULATION TESTING Educational Commentary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Coagulation Testing: High Hematocrit-Anticoagulant Adjustment
PREANALYTIC PULSE Coagulation Testing: High Hematocrit-Anticoagulant Adjustment In 1980, CLSI released H21-A4 guidelines for coagulation testing, which included the recommendation to adjust/correct the amount of citrate in blue-top evacuated blood collection tubes for patients presenting hematocrits greater than 55%. In addition to the CLSI guidelines, the CAP hematology checklist HEM.22830 includes the question, “Are there documented guidelines for the detection and special handling of specimens with elevated hematocrits?” Principle The adjustment is to assure the plasma:anticoagulant ratio (not the blood:anticoagulant ratio) stays consistent. A patient with high hematocrit, greater than 55%, will result in less plasma after centrifugation. The plasma fraction will contain an increased concentration of sodium citrate anticoagulant. The increased concentration may result in falsely prolonged test results for Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT). Formula 1. To calculate the corrected 3.2% sodium citrated whole blood for hematocrit > 55%, adjust the citrate to the proper volume with the following formula: -3 C = (1.85 x 10 )(100-HCT)(Vblood) Where: C = volume of sodium citrate required for that volume of blood HCT = patient’s hematocrit V = volume of blood required in the blood collection tube (example if a 3mL tube is used the blood draw volume is 2.7mL) 1.85 x 10-3 is a constant (considering the citrate volume, blood volume, and citrate concentration). 2. Example: Patient has a Hct of 60% and the patient’s blood will be drawn into a 3mL VACUETTE® sodium citrate (blue-top) blood collection tube. Adjustment of the sodium citrate volume is calculated as: C = (1.85 x 10-3)(100-60)(2.7mL) C = 0.20mL (rounded up from 01.998mL) Remove: 0.30 - 0.20 = 0.10mL of sodium citrate to be removed (0.30 is the difference between the total tube volume of 3.0mL and the blood drawn into the tube of 2.7mL) Method The instructions to prepare an adjusted sodium citrate tube are to be documented in the Laboratory Standard Operating Procedures. -
Role of Real-Time / Accurate Diagnostic Testing in Patient Blood Management Programs
ROLE OF REAL-TIME / ACCURATE DIAGNOSTIC TESTING IN PATIENT BLOOD MANAGEMENT PROGRAMS POINT-OF-CARE TESTING “Diagnostic testing is an essential component of Patient Blood Management. The accurate assessment of the true causes of bleeding dysfunction facilitates the employment of evidence based, goal directed therapy to rapidly prevent and treat excess blood loss. “ Sherri Ozawa RN, Clinical Director, Institute of Patient Blood Management, Englewood Hospital Medical Center, Englewood, New Jersey. PATIENT BLOOD MANAGEMENT Interdisciplinary Managing Blood Conservation Anemia Modalities “The timely application of evidence based medical and surgical concepts designed to manage IMPROVED anemia, optimize hemostasis, and PATIENT minimize blood loss in order to OUTCOMES improve patient outcomes.” SABM© 2018 - Society for the Advancement of Blood Management (SABM.org) Optimizing Patient-Centered Coagulation Decision Making Point-of-care testing forms an integral part of PBM, enabling accurate and real-time diagnosis of anemia and bleeding and facilitating precise and targeted hemostatic intervention. 1 Conventional coagulation tests are unable to provide needed information on actual bleeding risk/defects 1, thus delaying appropriate and targeted treatment. Slow turnaround times for laboratory-based conventional coagulation tests are one of the major drivers of empirical treatment regimens, which inevitably result in some patients receiving unnecessary, inappropriate and avoidable transfusions, with associated increased morbidity and mortality, and -
Global Assays of Hemostasis in the Diagnostics of Hypercoagulation and Evaluation of Thrombosis Risk Elena N Lipets1 and Fazoil I Ataullakhanov1,2,3,4,5,6*
Lipets and Ataullakhanov Thrombosis Journal (2015) 13:4 DOI 10.1186/s12959-015-0038-0 REVIEW Open Access Global assays of hemostasis in the diagnostics of hypercoagulation and evaluation of thrombosis risk Elena N Lipets1 and Fazoil I Ataullakhanov1,2,3,4,5,6* Abstract Thrombosis is a deadly malfunctioning of the hemostatic system occurring in numerous conditions and states, from surgery and pregnancy to cancer, sepsis and infarction. Despite availability of antithrombotic agents and vast clinical experience justifying their use, thrombosis is still responsible for a lion’s share of mortality and morbidity in the modern world. One of the key reasons behind this is notorious insensitivity of traditional coagulation assays to hypercoagulation and their inability to evaluate thrombotic risks; specific molecular markers are more successful but suffer from numerous disadvantages. A possible solution is proposed by use of global, or integral, assays that aim to mimic and reflect the major physiological aspects of hemostasis process in vitro. Here we review the existing evidence regarding the ability of both established and novel global assays (thrombin generation, thrombelastography, thrombodynamics, flow perfusion chambers) to evaluate thrombotic risk in specific disorders. The biochemical nature of this risk and its detectability by analysis of blood state in principle are also discussed. We conclude that existing global assays have a potential to be an important tool of hypercoagulation diagnostics. However, their lack of standardization currently impedes their application: different assays and different modifications of each assay vary in their sensitivity and specificity for each specific pathology. In addition, it remains to be seen how their sensitivity to hypercoagulation (even when they can reliably detect groups with different risk of thrombosis) can be used for clinical decisions: the risk difference between such groups is statistically significant, but not large. -

64Th Annual SSC Meeting, in Conjunction with the 2018 ISTH Congress in Dublin, Ireland Meeting Minutes Standing Committees Coagulation Standards Committee
64th Annual SSC meeting, in conjunction with the 2018 ISTH Congress in Dublin, Ireland Meeting Minutes Standing Committees Coagulation Standards Committee............................................................... 3 Subcommittees Animal, Cellular and Molecular Models ........................................................ 6 Biorheology .................................................................................................. 9 Control of Anticoagulation ............................................................................ 15 Disseminated Intravascular Coagulation ...................................................... 20 Factor VIII, Factor IX and Rare Coagulation Disorders ................................ 23 Factor XI and the Contact System ............................................................... 27 Factor XIII and Fibrinogen ............................................................................ 30 Fibrinolysis ................................................................................................... 34 Genomics in Thrombosis and Hemostasis ................................................... 38 Hemostasis and Malignancy ........................................................................ 47 Lupus Anticoagulant/Phospholipid Dependent Antibodies ........................... 51 Pediatric and Neonatal Hemostasis and Thrombosis ................................... 57 Perioperative and Critical Care Thrombosis and Hemostasis ...................... 66 Plasma Coagulation Inhibitors ..................................................................... -

Pre-Analytical Variables in the Coagulation Lab: Why Does It Matter?
Generate Knowledge Pre-Analytical Variables in the Coagulation Lab: Why Does It Matter? Paul Riley, PhD, MBA Pre-Analytical Variables: Objectives 1. Define Pre-Analytical variables 2. Explain how blood collection may impact test results 3. Describe best practices for sample transport and storage 4. Review sample processing procedures 5. Identify patient variables that may affect coagulation testing What are Pre-Analytical Variables? Includes everything that may affect a patient specimen from the clinician ordering the test to the point of analysis Some patient variables are out of the lab’s control (medications, lipemia, icterus, etc.) The biggest source of laboratory error - far exceeds analytical error Scope? Up to 70% of testing errors occur in the pre-analytical phase1 It is not always clear when a sample is received in the lab that it may be unsuitable or compromised Lab results lead to clinical action 70-80% of all clinical decisions regarding patient care are based on lab results Coag samples are especially susceptible Sample collection initiates clotting PT and PTT are complex enzymatic reactions 1. Plebani M: Quality indicators to detect pre-analytical errors in Laboratory testing. Clin Biochem Rev 2012; 33:85-88 Scope? What are the ramifications of pre-analytical errors for the patient? Misdiagnosis Inappropriate treatment Diligence is required on the part of the laboratory to prevent incorrect results Must have quality indicators in place to monitor the steps of the pre- analytical phase Event management where errors are investigated and corrected so that repeat events are prevented Scope? When a sample is compromised: • the test result may reflect the status of the sample • but not reflect the clinical status of the patient Guidelines In order to improve the quality of patients results, sample collection and handling should follow the CLSI guideline H21-A5; 2008 Test Ordering Is the right test ordered on the right patient? Coag is confusing - Names sound alike! Factor X vs. -
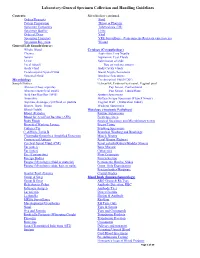
Laboratory-General Specimen Collection and Handling Guidelines
Laboratory-General Specimen Collection and Handling Guidelines Contents: Microbiology continued. Orders/Requests Stool Patient Preparation Throat or Pharynx Specimen Containers Tuberculosis (TB) Specimen Quality Urine Order of Draw Viral Specimen Transport VRE Surveillance (Vancomycin- Resistant entercoccus) Specimen Rejection Wound General Lab Sample/Source: Whole Blood Cytology (Cytopathology) Plasma Aspiration, Fine Needle Serum Aspiration, Cyst Fluids Urine Submission of slide Fecal (Stool) Tips on making smears Body Fluid Body Cavity Fluids Cerebrospinal Spinal Fluid Breast Nipple Secretions Synovial Fluid Brushing Specimens Microbiology Cerebrospinal Fluid (CSF) Sample/Source: Ectocervix, Endocervical canal, Vaginal pool Abscess (Deep aspirate) Pap Smear, Conventional Abscess (superficial swab) Pap Smear, Liquid Base Acid Fast Bacillus (AFB) Sputum Specimens Anaerobic Surface Scrape Specimen (Tzanck Smear) Aspirate, drainage, cyst fluid, or pustule Vaginal Wall (Maturation Index) Biopsy, Bone, Tissue Washing Specimens Blood (Adult) Histology (Anatomic Pathology) Blood )Pediatric Routine Submission Blood for Acid Fast Bacillus (AFB) Fresh Specimen Body Fluids Surgical Specimen and Microbiology test(s) Bronchial Washing Lavage Breast Tissue Catheter Tip Brushing Specimens C. difficile Toxin B Bronchial Washing and Brushings Chlamydia/Gonorrhea Amplified Detection Muscle Biopsy Crytococcal Antigen Renal Biopsy (Kidney) Cerebral Spinal Fluid (CSF) Renal calculi (Kidney/Bladder Stones) Ear (outer) Bone Marrow Ear (inner) Cytogenics Eye -

Point of Care Coagulation Testing
POINT OF CARE COAGULATION TESTING Dr Danny Morland Royal Victoria Infirmary Newcastle upon Tyne 11 th October 2016 Introduction Declarations of Interest: None CONTENT Introduction to POCT Principles Interpretation Treatment Literature NUTH Experience Point Of Care Testing (POCT) Medical diagnostic testing at (or near) the point of care. POCT PROS CONS • Quick • Cost (potentially) • Convenient • Quality • Reliable • Training • Efficient • Workload • Recording • Risk of inappropriate decision-making Point of Care Coagulation Testing (POCCT) Viscoelastic properties of whole blood clot Thromboelastography = Thromboelastometry (TEG) (ROTEM) Purported Benefits over Standard Tests • Measures whole blood, not just plasma • Looks at clot generation and propagation beyond the point of clot appearance • Allows comment on clot ‘quality’ • Can identify fibrinolysis FAST –potential information on clotting status within 5mins of test starting POCCT vs Standard Lab Tests POCCT LAB • Whole blood • Highly standardised • Clot beyond first • Trained, professional staff appearance • Quality control • Clot quality • Well established • Identify fibrinolysis • Complete picture • FAST • Cost PRINCIPLES Viscoelasticity Hardware OUTPUTS Panel Testing – Normal results INTERPRETATION Normal Low Platelets Normal Hypo-fibrinogenaemia Heparin Effect Normal TREATMENT LIMITATIONS AND WARNINGS • Treatment should be administered according to the clinical picture (e.g. volume & current rate of blood loss) • Viscoelastic devices are not uniformly sensitive to all disturbances -

PDF Download
364 Review Article Can We Measure the Individual Prothrombotic or Prohemorrhagic Tendency by Global Coagulation Tests? Ã Ã Sara Reda1, Laure Morimont2,3, Jonathan Douxfils2,3 Heiko Rühl1 1 Institute of Experimental Hematology and Transfusion Medicine, Address for correspondence Heiko Rühl, MD, Institute of University of Bonn, Bonn, Germany Experimental Hematology and Transfusion Medicine, University of 2 Department of Pharmacy, Namur Thrombosis and Hemostasis Bonn, Venusberg-Campus 1, 53127 Bonn, Germany Center,UniversityofNamur,Namur,Belgium (e-mail: [email protected]). 3 Qualiblood s.a., Namur, Belgium Hämostaseologie 2020;40:364–378. Abstract Hemostasis is a complex process in which abnormalities can cause shifts toward prothrombotic or prohemorrhagic states resulting in thrombosis or bleeding, respec- tively. Several coagulation tests may be required to characterize these defects but may yet not always reflect a patient’s true hemostatic capacity. Thus, global coagulation tests aiming to simulate the coagulation process in vitro instead of measuring single components thereof are certainly of interest to assess prothrombotic or prohemor- rhagic tendencies. This review describes the development and application of global Keywords coagulation tests, concentrating on the more widely used methods of viscoelastometry ► global coagulation and thrombin generation. A focus is placed on conditions characterized by simulta- tests neous changes of various components of hemostasis, such as anticoagulant therapy or ► hypercoagulability hormone-induced coagulopathy, in which global coagulation tests are especially ► bleeding promising. If the key challenges of standardization and automation of these tests ► anticoagulant drugs are solved, as is the case with automated thrombogram or clot waveform analysis, ► hormone-induced global coagulation assays will play an important role in the future of laboratory coagulopathy diagnostics of hemostasis and thrombosis. -

Five-Minute Preparation of Platelet-Poor Plasma for Routine Coagulation Testing A
املجلة الصحية لرشق املتوسط املجلد السادس عرش العدد الثاين Five-minute preparation of platelet-poor plasma for routine coagulation testing A. Sultan1 إعداد يستغرق 5دقائق للبﻻزما الفقرية بالصفيحات من أجل اﻻختبار الروتيني للتخثر أمحد حسن سلطان تتطلب اخلﻻصـة:الدﻻئل اﻹرشادية ملؤسسة املعايري اﻹكلينيكية ومعايري املختربات أن جترى اﻻختبارات الروتينية للتخثر ببﻻزما فقرية بالصفيحات )أقل من 000 10 صفيحة/مكرولرت(، وحترض من كامل الدم املضاف إليه السرتات وجرى تنبيذه برسعة منخفضة ملدة 10 – 30 دقيقة. وملقارنة النتائج التي تم احلصول عليها من البﻻزما التي خضعت للتنبيذ ملدة 5دقائق برسعة 3000جاذبية أو ملدة 10 دقائق برسعة 2000 جاذبية، أجريت مقايسة شملت 46عينة مأخوذة من بالغني أصحاء أسوياء بقصد التعرف عىل زمن الربوثرومني، وزمن الثرومبوبﻻستني اجلزئي املفعّل لواملعدَّ الدويل املسوَّ ى. ﻻ يوجد اختﻻفات يعتد هبا يف نتائج اﻻختبار، ُواستنتج ِأن النبذ ملدة مخس دقائق بمقدار g 3000يعترب ًاختيارا ًموثوقا فيه ًومفيدا للحد من الوقت املستغرق يف هذه اﻻختبارات. ABSTRACT Clinical and Laboratory Standard Institute guidelines require that routine coagulation tests are performed with platelet-poor plasma (< 10 000 platelets/µL) and prepared from whole citrated blood centrifuged at low speed for 10–30 minutes. To compare results obtained from plasma centrifuged for 5 minutes at 3000 g or for 10 minutes at 2000 g, 46 blood samples from normal healthy adults were assayed for prothrombin time, international normalized ratio and activated partial thromboplastin time. No significant differences were found in test results and it was concluded that 5 minutes centrifugation at 3000 g is a reliable and useful option to reduce the turnaround time for these tests. Préparation en cinq minutes d’un plasma pauvre en plaquettes pour les tests d’hémostase de routine RÉSUMÉ Les recommandations du CLSI (Clinical and Laboratory Standard Institute) imposent que les tests d’hémostase soient réalisés avec du plasma pauvre en plaquettes (< 10 000 plaquettes/µL) et préparés à partir de sang total citraté, centrifugé à vitesse lente pendant 10 à 30 minutes. -

EDUCATION Four Compartments
J R Coll Physicians Edinb 2014; 44:42–5 CME http://dx.doi.org/10.4997/JRCPE.2014.110 © 2014 Royal College of Physicians of Edinburgh Coagulation YL Chee Consultant Haematologist, Department of Haematology-Oncology, National University Hospital, Singapore ABSTRACT The haemostatic system comprises four compartments: the vasculature, Correspondence to YL Chee platelets, coagulation factors, and the fibrinolytic system. There is presently no Consultant Haematologist laboratory or near-patient test capable of reproducing the complex regulated Department of Haematology- Oncology interaction between these four compartments. The prothrombin time (PT) and NUHS Tower Block Level 7 activated partial thromboplastin time (APTT) only test the coagulation protein 1E Kent Ridge Road compartment of the system and results have to be carefully interpreted in the Singapore 119228 context of the clinical presentation and assay limitations. This article will give a e-mail general overview of the limitations of PT and APTT and discuss specific issues that [email protected] need to be considered when the tests are requested, in the context of anticoagulant monitoring, bleeding symptoms, and routine preoperative screening. Of these indications, routine preoperative screening is the most controversial and is generally not warranted in the absence of an abnormal bleeding history. KEYWORDS Prothrombin time, activated partial thromboplastin time, thrombin clotting time, preoperative screening, bleeding history, coagulation screen DECLARATIONS OF INTERESTS No conflicts of interest declared. INTRODUCTION Intrinsic pathway Extrinsic pathway The normal haemostatic system comprises four Factor XII/HMWK*/PK** compartments, the vasculature, platelets, coagulation proteins and the fibrinolytic system. When a blood Factor XI Factor XIa vessel is injured, all four compartments interact in a coordinated manner to prevent blood loss by forming a Factor IX Factor IXa Factor VIIa clot and localising this to the area of injury. -

Coagulation Simplified…
Coagulation Simplified… Published by ACKNOWLEDGEMENTS CONTENTS We gratefully acknowledge the support and funding provided by the Ontario Ministry of Health 1. The Basics of Coagulation and Clot Breakdown . 4–7 and Long-Term Care. 2. Routine Coagulation Tests . 8–17 Special thanks to the following people and organizations who provided their expertise in Evaluating coagulation in the laboratory . 8 reviewing the content of this handbook: Sample collection for coagulation testing . 9 Prothrombin Time (PT) . 10 L Gini Bourner (QMP-LS Hematology Committee) International Normalized Ratio (INR) . 11 L Dr. Jeannie Callum Activated Partial Thromboplastin Time (APTT) . 12 L Dr. Allison Collins Thrombin Time (TT) . 13 Fibrinogen . 14 L Dr. William Geerts D-dimer . 15 L Dr. Alejandro Lazo-Langner Anti-Xa assay . 16 L Dr. Ruth Padmore (QMP-LS Hematology Committee) Summary . 17 L Anne Raby (QMP-LS Hematology Committee) 3. Anticoagulant Drugs . 18–25 L Dr. Margaret Rand Unfractionated Hepari n (UFH) . 18 L Dr. Alan Tinmouth Low Molecular Weight Heparins (LMWHs) . 19 Fondaparinux . 20 Warfarin . 21 Thanks also to: Direct Thrombin Inhibitors (DTI) . 23 L Dale Roddick, photographer, Sunnybrook Health Sciences Centre Direct Xa Inhibitors . 25 L Reena Manohar, graphic artist, Sunnybrook Health Sciences Centre 4. Evaluating Abnormal Coagulation Tests . 26–29 L The ECAT Foundation Prolonged PT / INR with normal APTT . 26 CLOT-ED Images used or modified with permission from Prolonged APTT with normal PT / INR . 27 the ECAT Foundation, The Netherlands. Prolonged APTT and PT / INR . 28 Prolonged Thrombin Time (TT) with normal or prolonged APTT and PT / INR . 29 March 2013 5. Approach to the Evaluation of the Bleeding Patient . -

Viscoelastic Testing Inside and Beyond the Operating Room
299-308 Review Article Viscoelastic testing inside and beyond the operating room Liang Shen, Sheida Tabaie, Natalia Ivascu Department of Anesthesiology, Weill Cornell Medical College, New York, NY, USA Contributions: (I) Conception and design: L Shen, N Ivascu; (II) Administrative support: None; (III) Provision of study materials or patients: L Shen, S Tabaie; (IV) Collection and assembly of data: L Shen, S Tabaie; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Liang Shen, MD, MPH. Department of Anesthesiology, Weill Cornell Medical College, 525 East 68 St., P300 New York, NY 10065, USA. Email: [email protected]. Abstract: Hemorrhage is a major contributor to morbidity and mortality during the perioperative period. Current methods of diagnosing coagulopathy have various limitations including long laboratory runtimes, lack of information on specific abnormalities of the coagulation cascade, lack of in vivo applicability, and lack of ability to guide the transfusion of blood products. Viscoelastic testing offers a promising solution to many of these problems. The two most-studied systems, thromboelastography (TEG) and rotational thromboelastometry (ROTEM), offer similar graphical and numerical representations of the initiation, formation, and lysis of clot. In systematic reviews on the clinical efficacy of viscoelastic tests, the majority of trials analyzed were in cardiac surgery patients. Reviews of the literature suggest that transfusions of packed red blood cells (pRBC), plasma, and platelets are all decreased in patients whose transfusions were guided by viscoelastic tests rather than by clinical judgement or conventional laboratory tests. Mortality appears to be lower in the viscoelastic testing groups, despite no difference in surgical re-intervention rates and massive transfusion rates.