Solar and Ultraviolet Radiation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Table S6. Names and Functions of 44 Target Genes and 4 Housekeeping Genes Assessed for Gene Expression Measurements
Table S6. Names and functions of 44 target genes and 4 housekeeping genes assessed for gene expression measurements. Gene Gene name Function Category Reference CD45 CD45 (leukocyte common antigen) Regulation of T-cell and B-cell antigen receptor signaling Adaptive NCBI, UniProt HIVEP2 Human immunodeficiency virus typeI enhancer2 Transcription factor, V(D)J recombination, MHC enhancer binding Adaptive (Diepeveen et al. 2013) HIVEP3 Human immunodeficiency virus typeI enhancer3 Transcription factor, V(D)J recombination, MHC enhancer binding Adaptive (Diepeveen et al. 2013) IgM-lc Immunoglobulin light chain Recognition of antigen or pathogen Adaptive NCBI, UniProt Integ-Bt Integrin-beta 1 Cell signaling and adhesion of immunoglobulin Adaptive NCBI, UniProt Lymph75 Lymphocyte antigen 75 Directs captured antigens to lymphocytes Adaptive (Birrer et al. 2012) Lympcyt Lymphocyte cytosolic protein 2 Positive role in promoting T-cell development and activation Adaptive NCBI, UniProt TAP Tap-binding protein (Tapasin) Transport of antigenic peptides, peptide loading on MHC I Adaptive NCBI, UniProt AIF Allograft inflammation factor Inflammatory responses, allograft rejection, activation of macrophages Innate (Roth et al. 2012) Calrcul Calreticulin Chaperone, promotes phagocytosis and clearance of apoptotic cells Innate NCBI, UniProt Cf Coagulation factor II Blood clotting and inflammation response Innate (Birrer et al. 2012) IL8 Interleukin 8 Neutrophil chemotactic factor, phagocytosis, inflammatory activity Innate NCBI, UniProt Intf Interferon induced transmembrane protein 3 Negative regulation of viral entry into host cell, antiviral response Innate NCBI, UniProt Kin Kinesin Intracellular transport Innate (Roth et al. 2012) LectptI Lectin protein type I Pathogen recognition receptors (C-type lectin type I) Innate NCBI, UniProt LectpII Lectin protein type II Pathogen recognition receptors (C-type lectin type II) Innate NCBI, UniProt Nramp Natural resistance-assoc macrophage protein Macrophage activation Innate (Roth et al. -

Mygene.Info R Client
MyGene.info R Client Adam Mark, Ryan Thompson, Chunlei Wu May 19, 2021 Contents 1 Overview ..............................2 2 Gene Annotation Service ...................2 2.1 getGene .............................2 2.2 getGenes ............................2 3 Gene Query Service ......................3 3.1 query ..............................3 3.2 queryMany ...........................4 4 makeTxDbFromMyGene....................5 5 Tutorial, ID mapping .......................6 5.1 Mapping gene symbols to Entrez gene ids ........6 5.2 Mapping gene symbols to Ensembl gene ids .......7 5.3 When an input has no matching gene ...........8 5.4 When input ids are not just symbols ............8 5.5 When an input id has multiple matching genes ......9 5.6 Can I convert a very large list of ids?............ 11 6 References ............................. 11 MyGene.info R Client 1 Overview MyGene.Info provides simple-to-use REST web services to query/retrieve gene annotation data. It’s designed with simplicity and performance emphasized. mygene is an easy-to-use R wrapper to access MyGene.Info services. 2 Gene Annotation Service 2.1 getGene • Use getGene, the wrapper for GET query of "/gene/<geneid>" service, to return the gene object for the given geneid. > gene <- getGene("1017", fields="all") > length(gene) [1] 1 > gene["name"] [[1]] NULL > gene["taxid"] [[1]] NULL > gene["uniprot"] [[1]] NULL > gene["refseq"] [[1]] NULL 2.2 getGenes • Use getGenes, the wrapper for POST query of "/gene" service, to return the list of gene objects for the given character vector of geneids. > getGenes(c("1017","1018","ENSG00000148795")) DataFrame with 3 rows and 7 columns 2 MyGene.info R Client query _id X_version entrezgene name <character> <character> <integer> <character> <character> 1 1017 1017 4 1017 cyclin dependent kin. -

Kin Discrimination Promotes Horizontal Gene Transfer Between Unrelated Strains in Bacillus Subtilis
ARTICLE https://doi.org/10.1038/s41467-021-23685-w OPEN Kin discrimination promotes horizontal gene transfer between unrelated strains in Bacillus subtilis ✉ Polonca Stefanic 1,5,6 , Katarina Belcijan1,5, Barbara Kraigher 1, Rok Kostanjšek1, Joseph Nesme2, Jonas Stenløkke Madsen2, Jasna Kovac 3, Søren Johannes Sørensen 2, Michiel Vos 4 & ✉ Ines Mandic-Mulec 1,6 Bacillus subtilis is a soil bacterium that is competent for natural transformation. Genetically 1234567890():,; distinct B. subtilis swarms form a boundary upon encounter, resulting in killing of one of the strains. This process is mediated by a fast-evolving kin discrimination (KD) system consisting of cellular attack and defence mechanisms. Here, we show that these swarm antagonisms promote transformation-mediated horizontal gene transfer between strains of low related- ness. Gene transfer between interacting non-kin strains is largely unidirectional, from killed cells of the donor strain to surviving cells of the recipient strain. It is associated with acti- vation of a stress response mediated by sigma factor SigW in the donor cells, and induction of competence in the recipient strain. More closely related strains, which in theory would experience more efficient recombination due to increased sequence homology, do not upregulate transformation upon encounter. This result indicates that social interactions can override mechanistic barriers to horizontal gene transfer. We hypothesize that KD-mediated competence in response to the encounter of distinct neighbouring strains could maximize the probability of efficient incorporation of novel alleles and genes that have proved to function in a genomically and ecologically similar context. 1 Biotechnical Faculty, University of Ljubljana, Ljubljana, Slovenia. -
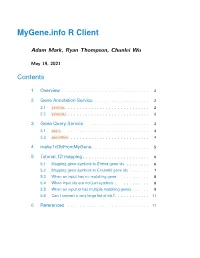
Mygene.Info R Client
MyGene.info R Client Adam Mark, Ryan Thompson, Chunlei Wu May 19, 2021 Contents 1 Overview ..............................2 2 Gene Annotation Service ...................2 2.1 getGene .............................2 2.2 getGenes ............................2 3 Gene Query Service ......................3 3.1 query ..............................3 3.2 queryMany ...........................4 4 makeTxDbFromMyGene....................5 5 Tutorial, ID mapping .......................6 5.1 Mapping gene symbols to Entrez gene ids ........6 5.2 Mapping gene symbols to Ensembl gene ids .......7 5.3 When an input has no matching gene ...........8 5.4 When input ids are not just symbols ............8 5.5 When an input id has multiple matching genes ......9 5.6 Can I convert a very large list of ids?............ 11 6 References ............................. 11 MyGene.info R Client 1 Overview MyGene.Info provides simple-to-use REST web services to query/retrieve gene annotation data. It’s designed with simplicity and performance emphasized. mygene is an easy-to-use R wrapper to access MyGene.Info services. 2 Gene Annotation Service 2.1 getGene • Use getGene, the wrapper for GET query of "/gene/<geneid>" service, to return the gene object for the given geneid. > gene <- getGene("1017", fields="all") > length(gene) [1] 1 > gene["name"] [[1]] NULL > gene["taxid"] [[1]] NULL > gene["uniprot"] [[1]] NULL > gene["refseq"] [[1]] NULL 2.2 getGenes • Use getGenes, the wrapper for POST query of "/gene" service, to return the list of gene objects for the given character vector of geneids. > getGenes(c("1017","1018","ENSG00000148795")) DataFrame with 3 rows and 7 columns 2 MyGene.info R Client query _id X_version entrezgene name <character> <character> <integer> <character> <character> 1 1017 1017 4 1017 cyclin dependent kin. -

Bioinformatics - 2 - Investigation of C
Advanced Skills in Biochemistry: Bioinformatics - 2 - Investigation of C. elegans protein kinase polypeptides Exercise 1 The purpose of this workshop is to familarise you with some of the databases and tools that are available for the analysis of proteins. For the purposes of this exercise, you will again be investigating the family of catalytic subunits of the cyclic AMP-dependent protein kinase (PK-A) in the free-living nematode, C. elegans. 1. The C. elegans polypeptide sequences we are interested in are encoded by the F47F2.1 gene on the X chromosome and the kin-1 gene on chromosome 1. In addition, we need the sequence of the mouse PK-A - catalytic subunit. The easiest way of obtaining each of these sequences is by making use of the Sequence Retrieval System (SRS). You should therefore visit the SRS Homepage: http://srs6.ebi.ac.uk/ 2. From the home page, select the Library Page tab. Then, under the UniProt Universal Protein Resource section, select the UniProtKB and UniParc databases. Then select the Standard Query Form. You should then carry out separate searches for the following accession numbers (i.e. select AccessionNumber from the drop-down menu in place of the default AllText): P05132, UPI000002AC77 and Q7JP68. These searches should find records for the polypeptide sequence for the mouse -catalytic subunit, the polypeptide sequence of the catalytic subunit encoded by the kin-1 gene and the F47F2.1b polypeptide sequence. Each of the records should be saved locally (e.g. on the desktop). 3. You should now prepare a simple text -

Karyomegalic Interstitial Nephritis and DNA Damage-Induced Polyploidy in Fan1 Nuclease-Defective Knock-In Mice
Downloaded from genesdev.cshlp.org on September 24, 2021 - Published by Cold Spring Harbor Laboratory Press RESEARCH COMMUNICATION Fancd2 ubiquitylation (K561) causes defective ICL repair Karyomegalic interstitial (Garcia-Higuera et al. 2001; Knipscheer et al. 2009; Deans nephritis and DNA damage- and West 2011). Fan1 is a 5′ flap endonuclease recruited to sites where induced polyploidy in Fan1 replisomes stall—for example, at ICLs—in a manner that requires Fancd2 ubiquitylation (Kratz et al. 2010; Liu et al. nuclease-defective knock-in 2010; MacKay et al. 2010; Smogorzewska et al. 2010). The mice nuclease activities of Fan1 are mediated by a C-terminal “ ” 1 1 VRR_nuc domain (Iyer et al. 2006), which is conserved Christophe Lachaud, Meghan Slean, in all orthologs as far back as yeasts. Fan1 also has a SAP- Francesco Marchesi,2 Claire Lock,3 Edward Odell,3 type DNA-binding domain and a UBZ4-type ubiquitin- Dennis Castor,1,4 Rachel Toth,1 binding domain, which interacts with ubiquityl-Fancd2, and John Rouse1 thereby recruiting Fan1 to sites of replisome stalling. Fan1 is required for efficient ICL repair, but, surprisingly, 1MRC Protein Phosphorylation and Ubiquitylation Unit, College this does not require interaction with ubiquityl-Fancd2 of Life Sciences, Sir James Black Centre, University of Dundee, (Lachaud et al. 2016). Similarly, genetic analyses in worms Dundee DD1 5EH, United Kingdom 2School of Veterinary and human cells showed that Fan1 and Fancd2 mutations Medicine, College of Medical, Veterinary, and Life Sciences, are not epistatic with respect to hypersensitivity to ICL- University of Glasgow, Glasgow G61 1QH, United Kingdom inducing drugs, suggesting that the two genes are not 3Department of Head and Neck Pathology, Guy’s Hospital, equivalent in function when it comes to ICL repair (Yosh- London SE1 9RT, United Kingdom ikiyo et al. -

Somamer Reagents Generated to Human Proteins Number Somamer Seqid Analyte Name Uniprot ID 1 5227-60
SOMAmer Reagents Generated to Human Proteins The exact content of any pre-specified menu offered by SomaLogic may be altered on an ongoing basis, including the addition of SOMAmer reagents as they are created, and the removal of others if deemed necessary, as we continue to improve the performance of the SOMAscan assay. However, the client will know the exact content at the time of study contracting. SomaLogic reserves the right to alter the menu at any time in its sole discretion. Number SOMAmer SeqID Analyte Name UniProt ID 1 5227-60 [Pyruvate dehydrogenase (acetyl-transferring)] kinase isozyme 1, mitochondrial Q15118 2 14156-33 14-3-3 protein beta/alpha P31946 3 14157-21 14-3-3 protein epsilon P62258 P31946, P62258, P61981, Q04917, 4 4179-57 14-3-3 protein family P27348, P63104, P31947 5 4829-43 14-3-3 protein sigma P31947 6 7625-27 14-3-3 protein theta P27348 7 5858-6 14-3-3 protein zeta/delta P63104 8 4995-16 15-hydroxyprostaglandin dehydrogenase [NAD(+)] P15428 9 4563-61 1-phosphatidylinositol 4,5-bisphosphate phosphodiesterase gamma-1 P19174 10 10361-25 2'-5'-oligoadenylate synthase 1 P00973 11 3898-5 26S proteasome non-ATPase regulatory subunit 7 P51665 12 5230-99 3-hydroxy-3-methylglutaryl-coenzyme A reductase P04035 13 4217-49 3-hydroxyacyl-CoA dehydrogenase type-2 Q99714 14 5861-78 3-hydroxyanthranilate 3,4-dioxygenase P46952 15 4693-72 3-hydroxyisobutyrate dehydrogenase, mitochondrial P31937 16 4460-8 3-phosphoinositide-dependent protein kinase 1 O15530 17 5026-66 40S ribosomal protein S3 P23396 18 5484-63 40S ribosomal protein -

Self-Identity Barcodes Encoded by Six Expansive Polymorphic Toxin Families Discriminate Kin in Myxobacteria
Self-identity barcodes encoded by six expansive polymorphic toxin families discriminate kin in myxobacteria Christopher N. Vassalloa,1 and Daniel Walla,2 aDepartment of Molecular Biology, University of Wyoming, Laramie, WY 82071 Edited by Christine Jacobs-Wagner, Yale University, West Haven, CT, and approved October 24, 2019 (received for review July 20, 2019) Myxobacteria are an example of how single-cell individuals can dynamic OM proteins, and, when 2 compatible cells touch, transition into multicellular life by an aggregation strategy. For these multiple receptor complexes from each cell coalesce into distinct and all organisms that consist of social groups of cells, discrimination foci that bridge the boundary between the 2 cells. This transient against, and exclusion of, nonself is critical. In myxobacteria, TraA is interaction culminates in an apparent membrane fusion and bi- a polymorphic cell surface receptor that identifies kin by homotypic directional transfer of proteins and lipids before cells separate by binding, and in so doing exchanges outer membrane (OM) proteins gliding motility (5–7). This striking and robust behavior is and lipids between cells with compatible receptors. However, TraA thought to help rejuvenate and maintain homeostasis of the cell variability alone is not sufficient to discriminate against all cells, as envelope in a population that ages or encounters insults in traA allele diversity is not necessarily high among local strains. To constantly fluctuating environments (8, 9). increase discrimination ability, myxobacteria include polymorphic In nutrient-rich soils, myxobacteria populations are numerous OM lipoprotein toxins called SitA in their delivered cargo, which and diverse (10, 11). Local strains compete with each other and poison recipient cells that lack the cognate, allele-specific SitI immu- must establish and maintain a group identity by recognizing and nity protein. -

Genome-Wide Association Studies in Alzheimer Disease
NEUROLOGICAL REVIEW Genome-Wide Association Studies in Alzheimer Disease Stephen C. Waring, DVM, PhD; Roger N. Rosenberg, MD he genetics of Alzheimer disease (AD) to date support an age-dependent dichotomous model whereby earlier age of disease onset (Ͻ60 years) is explained by 3 fully penetrant genes (APP [NCBI Entrez gene 351], PSEN1 [NCBI Entrez gene 5663], and PSEN2 [NCBI Entrez gene 5664]), whereas later age of disease onset (Ն65 years) representing most cases Tof AD has yet to be explained by a purely genetic model. The APOE gene (NCBI Entrez gene 348) is the strongest genetic risk factor for later onset, although it is neither sufficient nor necessary to ex- plain all occurrences of disease. Numerous putative genetic risk alleles and genetic variants have been reported. Although all have relevance to biological mechanisms that may be associated with AD patho- genesis, they await replication in large representative populations. Genome-wide association studies have emerged as an increasingly effective tool for identifying genetic contributions to complex dis- eases and represent the next frontier for furthering our understanding of the underlying etiologic, bio- logical, and pathologic mechanisms associated with chronic complex disorders. There have already been success stories for diseases such as macular degeneration and diabetes mellitus. Whether this will hold true for a genetically complex and heterogeneous disease such as AD is not known, al- though early reports are encouraging. This review considers recent publications from studies that have successfully applied genome-wide association methods to investigations of AD by taking advantage of the currently available high-throughput arrays, bioinformatics, and software advances. -

GAPGOM—An R Package for Gene Annotation Prediction Using GO Metrics Casper Van Mourik1,2, Rezvan Ehsani3,4,5* and Finn Drabløs1*
van Mourik et al. BMC Res Notes (2021) 14:162 https://doi.org/10.1186/s13104-021-05580-1 BMC Research Notes RESEARCH NOTE Open Access GAPGOM—an R package for gene annotation prediction using GO metrics Casper van Mourik1,2, Rezvan Ehsani3,4,5* and Finn Drabløs1* Abstract Objective: Properties of gene products can be described or annotated with Gene Ontology (GO) terms. But for many genes we have limited information about their products, for example with respect to function. This is particularly true for long non-coding RNAs (lncRNAs), where the function in most cases is unknown. However, it has been shown that annotation as described by GO terms to some extent can be predicted by enrichment analysis on properties of co- expressed genes. Results: GAPGOM integrates two relevant algorithms, lncRNA2GOA and TopoICSim, into a user-friendly R package. Here lncRNA2GOA does annotation prediction by co-expression, whereas TopoICSim estimates similarity between GO graphs, which can be used for benchmarking of prediction performance, but also for comparison of GO graphs in general. The package provides an improved implementation of the original tools, with substantial improvements in performance and documentation, unifed interfaces, and additional features. Keywords: Gene ontology, Annotation, Prediction, Long non-coding RNAs Introduction processes of gene regulation [3], but any useful annota- Te properties of gene products like proteins or non-pro- tion is in most cases missing. However, it has been shown tein coding RNAs (ncRNAs) can be described with Gene for example by Jiang et al. that annotation by GO terms Ontology (GO) terms as provided by the GO Consor- to some extent can be predicted [4]. -

Mouse Models of Inherited Retinal Degeneration with Photoreceptor Cell Loss
cells Review Mouse Models of Inherited Retinal Degeneration with Photoreceptor Cell Loss 1, 1, 1 1,2,3 1 Gayle B. Collin y, Navdeep Gogna y, Bo Chang , Nattaya Damkham , Jai Pinkney , Lillian F. Hyde 1, Lisa Stone 1 , Jürgen K. Naggert 1 , Patsy M. Nishina 1,* and Mark P. Krebs 1,* 1 The Jackson Laboratory, Bar Harbor, Maine, ME 04609, USA; [email protected] (G.B.C.); [email protected] (N.G.); [email protected] (B.C.); [email protected] (N.D.); [email protected] (J.P.); [email protected] (L.F.H.); [email protected] (L.S.); [email protected] (J.K.N.) 2 Department of Immunology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand 3 Siriraj Center of Excellence for Stem Cell Research, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand * Correspondence: [email protected] (P.M.N.); [email protected] (M.P.K.); Tel.: +1-207-2886-383 (P.M.N.); +1-207-2886-000 (M.P.K.) These authors contributed equally to this work. y Received: 29 February 2020; Accepted: 7 April 2020; Published: 10 April 2020 Abstract: Inherited retinal degeneration (RD) leads to the impairment or loss of vision in millions of individuals worldwide, most frequently due to the loss of photoreceptor (PR) cells. Animal models, particularly the laboratory mouse, have been used to understand the pathogenic mechanisms that underlie PR cell loss and to explore therapies that may prevent, delay, or reverse RD. Here, we reviewed entries in the Mouse Genome Informatics and PubMed databases to compile a comprehensive list of monogenic mouse models in which PR cell loss is demonstrated.