Urinary Incontinence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![TAHUN 2018 [Kos Perkhidmat an (RM)] PEMBEDAHAN AM 1 Pharyngo](https://docslib.b-cdn.net/cover/6830/tahun-2018-kos-perkhidmat-an-rm-pembedahan-am-1-pharyngo-146830.webp)
TAHUN 2018 [Kos Perkhidmat an (RM)] PEMBEDAHAN AM 1 Pharyngo
JADUAL 6 FI PEMBEDAHAN TAHUN TAHUN TAHUN TAHUN 2018 [Kos Bil. Prosedur (BM) 2016 2015 (RM) 2017 (RM) Perkhidmat (RM) an (RM)] PEMBEDAHAN AM 1 Pharyngo-laryngo-oesophagectomy with reconstruction 5,407 7,012 8,617 11,024 2 Tracheo-oesophageal fistula 4,673 5,789 6,904 8,578 3 Total pancreatectomy 4,451 5,419 6,386 7,837 4 Pancreato duodenectomy (eg.Whipple’s operation) 4,451 5,419 6,386 7,837 5 Adrenalectomy 3,924 4,540 5,156 6,080 6 Adrenalectomy – bilateral 4,052 4,753 5,454 6,505 7 Total Parotidectomy –preserving of facial nerve 2,729 3,548 4,367 5,595 8 Partial Parotidectomy –preserving of facial nerve 2,517 3,195 3,873 4,890 9 Total thyroidectomy 2,252 2,753 3,254 4,005 10 Partial thyroidectomy 2,211 2,685 3,159 3,870 11 Hemithyroidectomy 2,211 2,685 3,159 3,870 12 Subtotal thyroidectomy bilateral 2,234 2,723 3,212 3,945 13 Thyroglossal Cyst 1,694 1,824 1,953 2,147 14 Block Dissection of cervical glands 3,170 4,284 5,397 7,068 15 Parathyroidectomy 2,410 3,017 3,623 4,533 16 Mastectomy with/without axillary clearance 1,935 2,226 2,516 2,951 17 Wide excision for carcinoma breast 1,760 1,934 2,107 2,367 18 Total oesophagectomy and interposition of intestine 4,532 6,554 8,575 11,607 19 Repair of diaphragmatic hernia-transabdominal 2,322 2,870 3,418 4,240 20 Total gastrectomy 2,635 3,392 4,149 5,284 21 Partial gastrectomy (benign disease) 2,274 2,790 3,305 4,079 22 Partial gastrectomy (malignant disease) 2,451 3,085 3,718 4,669 Page 1 JADUAL 6 FI PEMBEDAHAN TAHUN TAHUN TAHUN TAHUN 2018 [Kos Bil. -

Vesicovaginal Fistula (Vvf) 1
VESICOVAGINAL FISTULA (VVF) 1 REVIEW PROF-1186 VESICOVAGINAL FISTULA (VVF) PROF. DR. M. SHUJA TAHIR PROF. DR. MAHNAZ ROOHI FRCS (Edin), FCPS Pak (Hon) FRCOG (UK) Professor of Surgery Professor & Head of Department Gynae & Obst. Independent Medical College, Gynae Unit-I, Allied Hospital, Faisalabad. Punjab Medical College, Faisalabad. Article Citation: Muhammad Shuja Tahir, Mahnaz Roohi. Vesicovaginal fistula (VVF). Professional Med J Mar 2009; 16(1): 1-11. ABSTRACT... Vesicovaginal fistula is not an uncommon condition. It gives rise to multiple socio-psychological problems for women usually of younger age. It can be prevented by improving the level of education, health care and poverty. Early diagnosis and appropriate treatment is required to help the patient. Preoperative assessment , treatment of co-morbid factors, proper surgical approach & technique ensures success of surgery. Postoperative care of the patient is equally important to avoid surgical failure. addition to the medical sequelae from these fistulas. It can be caused by injury to the urinary tract, which can occur accidentally during surgery to the pelvic area, such as a hysterectomy. It can also be caused by a tumor in the vesicovaginal area or by reduced blood supply due to tissue death (necrosis) caused by radiation therapy or prolonged labor during childbirth. Patients with vaginal fistulas usually present 1 to 3 weeks after a gynecologic surgery with complaints of continuous urinary incontinence, vaginal discharge, pain or an abnormal urinary stream. Obstetric fistula lies along a continuum of problems affecting women's reproductive health, starting with genital infections and finishing with Vesicovaginal fistula maternal mortality. It is the single most dramatic aftermath of neglected childbirth due to its disabling It is a condition that arises mostly from trauma sustained nature and dire social, physical and psychological during child birth or pelvic operations caused by the consequences. -

15-1040-Junu Oh-Neuronal.Key
Neuronal Control of the Bladder Seung-June Oh, MD Department of urology, Seoul National University Hospital Seoul National University College of Medicine Contents Relevant end organs and nervous system Reflex pathways Implication in the sacral neuromodulation Urinary bladder ! body: detrusor ! trigone and bladder neck Urethral sphincters B Preprostatic S Smooth M. Sphincter Passive Prostatic S Skeletal M. Sphincter P Prostatic SS P-M Striated Sphincter Membraneous SS Periurethral Striated M. Pubococcygeous Spinal cord ! S2–S4 spinal cord ! primary parasympathetic micturition center ! bladder and distal urethral sphincter ! T11-L2 spinal cord ! sympathetic outflow ! bladder and proximal urethral sphincter Peripheral innervation ! The lower urinary tract is innervated by 3 principal sets of peripheral nerves: ! parasympathetic -pelvic n. ! sympathetic-hypogastric n. ! somatic nervous systems –pudendal n. ! Parasympathetic and sympathetic nervous systems form pelvic plexus at the lateral side of the rectum before reaching bladder and sphincter Sympathetic & parasympathetic systems ! Sympathetic pathways ! originate from the T11-L2 (sympathetic nucleus; intermediolateral column of gray matter) ! inhibiting the bladder body and excite the bladder base and proximal urethral sphincter ! Parasympathetic nerves ! emerge from the S2-4 (parasympathetic nucleus; intermediolateral column of gray matter) ! exciting the bladder and relax the urethra Sacral somatic system !emerge from the S2-4 (Onuf’s nucleus; ventral horn) !form pudendal nerve, providing -

Clinical and Functional Anatomy of the Urethral Sphincter
Review Article International Neurourology Journal Int Neurourol J 2012;16:102-106 http://dx.doi.org/10.5213/inj.2012.16.3.102 pISSN 2093-4777 · eISSN 2093-6931 INJ Clinical and Functional Anatomy of the Urethral Sphincter Junyang Jung, Hyo Kwang Ahn, Youngbuhm Huh Department of Anatomy, Kyung Hee University School of Medicine, Seoul, Korea Continence and micturition involve urethral closure. Especially, insufficient strength of the pelvic floor muscles including the urethral sphincter muscles causes urinary incontinence (UI). Thus, it is most important to understand the main mechanism causing UI and the relationship of UI with the urethral sphincter. Functionally and anatomically, the urethral sphincter is made up of the internal and the external sphincter. We highlight the basic and clinical anatomy of the internal and the external sphinc- ter and their clinical meaning. Understanding these relationships may provide a novel view in identifying the main mechanism causing UI and surgical techniques for UI. Keywords: Urethral sphincters; Pudendal nerve; Autonomic nervous system; Urinary incontinence; Urination INTRODUCTION tomical damage to the ligaments, facial support, and pelvic floor musculature, including the levator ani [8]. The pudendal nerve The urethral sphincter is crucial for the maintenance of urinary innervating the EUS is susceptible to injury during vaginal birth continence [1,2]. The urethral sphincter refers to one of the fol- because it travels between the sacrospinous and sacrotuberous lowing muscles [3]: 1) the internal urethral sphincter (IUS), ligaments [9]. In this article, we discuss the basic and clinical which consists of smooth muscle and is continuous with the anatomy of the urethral sphincter and the relationship between detrusor muscle and under involuntary control, and 2) the ex- the urethral sphincter and UI. -

Abnormality of the Middle Phalanx of the 4Th Toe Abnormality of The
Glucocortocoid-insensitive primary hyperaldosteronism Absence of alpha granules Dexamethasone-suppresible primary hyperaldosteronism Abnormal number of alpha granules Primary hyperaldosteronism Nasogastric tube feeding in infancy Abnormal alpha granule content Poor suck Nasal regurgitation Gastrostomy tube feeding in infancy Abnormal alpha granule distribution Lumbar interpedicular narrowing Secondary hyperaldosteronism Abnormal number of dense granules Abnormal denseAbnormal granule content alpha granules Feeding difficulties in infancy Primary hypercorticolismSecondary hypercorticolism Hypoplastic L5 vertebral pedicle Caudal interpedicular narrowing Hyperaldosteronism Projectile vomiting Abnormal dense granules Episodic vomiting Lower thoracicThoracolumbar interpediculate interpediculate narrowness narrowness Hypercortisolism Chronic diarrhea Intermittent diarrhea Delayed self-feeding during toddler Hypoplastic vertebral pedicle years Intractable diarrhea Corticotropin-releasing hormone Protracted diarrhea Enlarged vertebral pedicles Vomiting Secretory diarrhea (CRH) deficient Adrenocorticotropinadrenal insufficiency (ACTH) Semantic dementia receptor (ACTHR) defect Hypoaldosteronism Narrow vertebral interpedicular Adrenocorticotropin (ACTH) distance Hypocortisolemia deficient adrenal insufficiency Crohn's disease Abnormal platelet granules Ulcerative colitis Patchy atrophy of the retinal pigment epithelium Corticotropin-releasing hormone Chronic tubulointerstitial nephritis Single isolated congenital Nausea Diarrhea Hyperactive bowel -

Urinary System
OUTLINE 27.1 General Structure and Functions of the Urinary System 818 27.2 Kidneys 820 27 27.2a Gross and Sectional Anatomy of the Kidney 820 27.2b Blood Supply to the Kidney 821 27.2c Nephrons 824 27.2d How Tubular Fluid Becomes Urine 828 27.2e Juxtaglomerular Apparatus 828 Urinary 27.2f Innervation of the Kidney 828 27.3 Urinary Tract 829 27.3a Ureters 829 27.3b Urinary Bladder 830 System 27.3c Urethra 833 27.4 Aging and the Urinary System 834 27.5 Development of the Urinary System 835 27.5a Kidney and Ureter Development 835 27.5b Urinary Bladder and Urethra Development 835 MODULE 13: URINARY SYSTEM mck78097_ch27_817-841.indd 817 2/25/11 2:24 PM 818 Chapter Twenty-Seven Urinary System n the course of carrying out their specific functions, the cells Besides removing waste products from the bloodstream, the uri- I of all body systems produce waste products, and these waste nary system performs many other functions, including the following: products end up in the bloodstream. In this case, the bloodstream is ■ Storage of urine. Urine is produced continuously, but analogous to a river that supplies drinking water to a nearby town. it would be quite inconvenient if we were constantly The river water may become polluted with sediment, animal waste, excreting urine. The urinary bladder is an expandable, and motorboat fuel—but the town has a water treatment plant that muscular sac that can store as much as 1 liter of urine. removes these waste products and makes the water safe to drink. -

Comparision of out Come of Vesico-Vaginal Fistula Repair With
Comparision of outcome of vesico vaginal fistula repair with and without omental patch Muhammad Tariq et al Original Article Comparision of Out Come of Muhammad Tariq* Iftikhar Ahmed** Muhammad Arif*** Vesico-Vaginal Fistula Repair with Muhammad Ashiq Ali**** Muhammad Iqbal Khan***** and Without Omental Patch Objective: to evaluate the outcome of vesicovaginal fistula repair with and without Post Graduate Registrar, interposition of omental patch. Department of Urology & Renal Study Design: Case Series Study Transplant Center BVH Bahawalpur Place and Duration: This study was carried out at Department of Urology & Renal ** Assistant Professor, Department Transplant center Bahawal Victoria Hospital Bahawalpur, from July 2008 to July 2010 of Urology & Renal Transplant Materials and Methods: Fifty patients having large size trigonal and supratrigonal Center. BVH Bahawalpur vesicovaginal fistula were included in this study. Those patients in whom urethra, rectum ***Medical Officer, Orthopedic are involved and those having vesicovaginal fistula due to radiation or malignancy were Complex BVH Bahawalpur. excluded from the study. All these patients were admitted from outdoor of Urology **** Orthopedic Surgeon. department. After getting complete history and investigation the diagnosis was made. *****House Officer Department of Patients were divided into two groups. In group A, vesicovaginal fistula repair was done by Urology & Renal Transplant Center interposition of omental patch between urinary bladder and vagina in group B, BVH Bahawalpur vesicovaginal fistula repair was done without interposition of omental patch. The result of both these group were compared. Results: Fifty patients were included in this study. Ages of these patients were between 20-70 year. Size of the fistula was between 3cm to 6cm. -

Vesico-Vaginal Fistulae; Review of the Causes, Diagnosis and Treatment
VESICO-VAGINAL FISTULAE The Professional Medical Journal www.theprofesional.com ORIGINAL PROF-2525 VESICO-VAGINAL FISTULAE; REVIEW OF THE CAUSES, DIAGNOSIS AND TREATMENT Dr. Bilqis Aslam Baloch1, Dr. Abdul Salam2, Dr. ZaibUnnisa3, Dr. Haq Nawaz4 1. FCPS Associate Professor of ABSTRACT… Objectives: To review the causes, diagnosis and treatment of vesico-vaginal Gynecology & Obstetrics fistulae in the department of Gynaecology& Obstetrics, and Urology Department Civil Hospital Bolan Medical College Quetta 2. MBBS, M.Phil Quetta. Background: Vesico-vaginal fistula is not life threatening medical disease, but the woman Department of Pharmacology face problems like demoralization, isolation, social boycott and even divorce. The etiology of Bolan Medical College Quetta the condition has been changed over the years and in developed countries obstetrical fistula are rare and they are usually result of gynecological surgeries or radiotherapy. In countries like Pakistan the situation is different, here literacy rate is low, parity rate is high and medical facilities are deficient. People manage delivery at home and usually multi parity. Urogenital fistula surgery doesn’t require special or advance technology but needs experienced urogynecologist with trained team and post operative care which can restore health, hope and sense of dignity to women. Methods: A retrospective study of 60 patients with different types of vesico-vaginal Correspondence Address: fistula werereviewed between January 2005 to December 2008. Patients were analyzed with Dr. BilqisAslamBaloch Associate Professor of regard to age, parity, cause, diagnosis, mode of treatment and outcome. Patients were also Gynaecology& Obstetrics evaluated initially according to prognosis. Results: During the study of four year period 60 APB/10 BMC Brewary Road Quetta patients of vesico-vaginal fistulae were reviewed. -

Scrutinization and Management of Urological Complications Attributed to Obstetrics and Gynecological Surgery Pritesh Jain1, Sandeep Gupta2, Dilip K Pal3
ORIGINAL ARTICLE Scrutinization and Management of Urological Complications Attributed to Obstetrics and Gynecological Surgery Pritesh Jain1, Sandeep Gupta2, Dilip K Pal3 ABSTRACT Aim: To review iatrogenic urological injuries due to obstetric and gynecological surgeries treated in the urology and gynecology department analyzing urinary tract anatomy, etiologic factors, diagnosis, treatment, and outcomes. Materials and methods: We reviewed all cases of urological injuries managed in our institution from January 2009 to December 2016 which were associated with obstetric and gynecological procedures. Results: Eighty-one patients were treated in the department during our study period. The most commonly injured organ was the bladder in 64.7% followed by ureter in 31.8%. Intraoperative diagnosis was made in 11.1% (9) cases, whereas 88.89% (72) cases were diagnosed postoperatively. Out of 81 cases, 66.7% (54) patients succumbed to urologic injuries as a result of gynecological procedures, while 33.3% (27) cases were due to obstetrical procedures. Vesicovaginal fistula (VVF) was the most common sequel followed by ureterovaginal fistula (UVF) in 42 (51.8%) and 15 (18.5%) cases, respectively. VVF combined with UVF and rectovaginal fistula were seen in 2 cases each. Although rare among various urogenital fistulas, vesicouterine fistula was encountered in three (3.7%) cases. All cases were managed with open or laparoscopic surgery with success in all but two patients. Conclusion: Complex gynecological procedures are gradually emerging as an important cause of urological injuries, second to obstetrical causes. Intraoperative detection and correction takes a vital part in determining structural integrity of the tissue and eliminating misery of the patient. -

The Distal Convoluted Tubule and Collecting Duct
Chapter 23 *Lecture PowerPoint The Urinary System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • Urinary system rids the body of waste products. • The urinary system is closely associated with the reproductive system – Shared embryonic development and adult anatomical relationship – Collectively called the urogenital (UG) system 23-2 Functions of the Urinary System • Expected Learning Outcomes – Name and locate the organs of the urinary system. – List several functions of the kidneys in addition to urine formation. – Name the major nitrogenous wastes and identify their sources. – Define excretion and identify the systems that excrete wastes. 23-3 Functions of the Urinary System Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Diaphragm 11th and 12th ribs Adrenal gland Renal artery Renal vein Kidney Vertebra L2 Aorta Inferior vena cava Ureter Urinary bladder Urethra Figure 23.1a,b (a) Anterior view (b) Posterior view • Urinary system consists of six organs: two kidneys, two ureters, urinary bladder, and urethra 23-4 Functions of the Kidneys • Filters blood plasma, separates waste from useful chemicals, returns useful substances to blood, eliminates wastes • Regulate blood volume and pressure by eliminating or conserving water • Regulate the osmolarity of the body fluids by controlling the relative amounts of water and solutes -

Urogenital Fistula: Studies on Epidemiology and Treatment Outcomes in High-Income and Low- and Middle-Income Countries
UROGENITAL FISTULA: STUDIES ON EPIDEMIOLOGY AND TREATMENT OUTCOMES IN HIGH-INCOME AND LOW- AND MIDDLE-INCOME COUNTRIES Work submitted to Newcastle University for the degree of Doctor of Science in Medicine September 2018 Paul Hilton MB, BS (Newcastle University, 1974); MD (Newcastle University, 1981); FRCOG (Royal College of Obstetricians & Gynaecologists, 1996) Clinical Academic Office (Guest) and Institute of Health and Society (Affiliate) Newcastle University, Newcastle upon Tyne, United Kingdom ii Table of contents Table of contents ..................................................................................................................iii List of tables ......................................................................................................................... v List of figures ........................................................................................................................ v Declaration ..........................................................................................................................vii Abstract ............................................................................................................................... ix Dedication ............................................................................................................................ xi Acknowledgements ............................................................................................................ xiii Funding ..................................................................................................................................... -
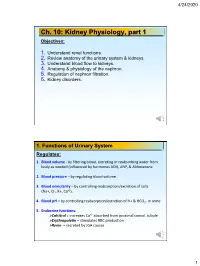
Kidney Physiology, Part 1 Objectives
4/24/2020 Ch. 10: Kidney Physiology, part 1 Objectives: 1. Understand renal functions. 2. Review anatomy of the urinary system & kidneys. 3. Understand blood flow to kidneys. 4. Anatomy & physiology of the nephron. 5. Regulation of nephron filtration. 6. Kidney disorders. 1. Functions of Urinary System Regulates: 1. Blood volume - by filtering blood, excreting or reabsorbing water from body as needed (influenced by hormones ADH, ANP, & Aldosterone 2. Blood pressure – by regulating blood volume. 3. Blood osmolarity – by controlling reabsorption/excretion of salts (Na+, Cl-, K+, Ca+2). 4. Blood pH – by controlling reabsorption/excretion of H+ & HCO3- in urine. 5. Endocrine functions: >Calcitrol = increases Ca+2 absorbed from proximal convol. tubule >Erythropoietin = stimulates RBC production >Renin = secreted by JGA causes 1 4/24/2020 Urinary Facts: ─ Kidneys CAN filter 5.5L/40min OR 180 L/day! ─ 99% of filtrate is automatically reabsorbed,, regardless of hydration state ─ 1% might/might not be reabsorbed – depends on hormones. ─ Avg urine output (pee) = 0.7 – 2.0 L/day (30 – 80 ml/hr) • Oliguria = smaller than normal urine output • Polyuria = higher than normal urine output • Anuria = no urine production (BAD) ─ Obligatory water loss = 400 ml (must pee out to rid body of wastes) ─ “osmolality” = osmoles (Osm) of solute per kg of solvent (Osm/kg) ─ “osmolarity” = osmoles (Osm) of solute per liter of solution (Osm/L) More accurate for understanding osmotic effects than mass of solute in solution Different kinds of solute can have different sizes Some solutions may have multiple kinds of solute 2. REVIEW anatomy of Urinary System Kidneys = paired organs, posterior abdominal cavity - 8 – 12 renal lobes per kidney - lobes contain millions of nephrons - adrenal glands on top of kidneys.