Developing a Total Quality Management Framework for Healthcare Organizations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Industrial Engineering and Management Sciences 1
Industrial Engineering and Management Sciences 1 Methods for designing and analyzing industrial experiments. Blocking; INDUSTRIAL ENGINEERING randomization; multiple regression; factorial and fractional factorial experiments; response surface methodology; Taguchi's robust design; AND MANAGEMENT SCIENCES split plot experimentation. Homework, labs, and project. Prerequisite: IEMS 201-0, IEMS 303-0, or equivalent. Degree Types: PhD IEMS 308-0 Data Science and Analytics (1 Unit) The Industrial Engineering and Management Sciences PhD Program Focuses on select problems in data science, in particular clustering, (https://www.mccormick.northwestern.edu/industrial/phd-program/) association rules, web analytics, text mining, and dimensionality produces researchers who combine strength in core methodologies reduction. Lectures will be completed with exercises and projects in open of operations research (e.g., optimization, stochastic modeling and source framework R. Prior knowledge of classification techniques and R simulation, statistics, and data analytics) with the ability to apply them is required. to yield practical benefits in solving problems that are important in the Prerequisites: IEMS 304-0; COMP_SCI 217-0. real world. The program offers students the opportunity to use skills IEMS 310-0 Operations Research (1 Unit) in computing, mathematical analysis and modeling, and economics to Survey of operations research techniques. Linear programming, decision produce research that helps to improve the efficiency, quality, and the theory, stochastic processes, game theory. May not be taken for credit potential of organizations to fulfill their missions. The program prepares with or after IEMS 313-0. students for research-based careers in industry, academia, non-profit, and Prerequisites: IEMS 201-0 or IEMS 202-0; GEN_ENG 205-1 or MATH 240-0. -

Industrial Engineering Roles in Industry
Industrial Engineering Roles In Industry Prepared by the IIE-IAB (Institute of Industrial Engineers – Industry Advisory Board) www.iienet.org What Do IEs Do? • Industrial Engineers work to make things better, be theyyp processes ,p, products or s ystems • Typical focus areas include: – Project Management – Manufacturing, Production and Distribution – Supply Chain Management – Productivity, Methods and Process Eng ineerin g – Quality Measurement and Improvement – Program Management – Ergonomics/Human Factors – Technology Development and Transfer – Strategic Planning – Management of Change – Financ ia l Eng ineer ing 2 Projjgect Management • Develop the detailed work breakdown structure of complex activities and form them into an integrated plan • Provide time based schedules and resource allocations for complex plans or implementations • UjtUse project managemen tthitft techniques to perform • Industrial Engineering analyses and investigations • Conduct facility planning and facility layout development of new and revised production plants and office buildings • Form and direct both small and large teams that work towards a defined objective , scope & deliverables • Perform risk analysis of various project options and outcomes 3 Manufacturing, Production and Distribution •Particippgate in design reviews to ensure manufacturabilit y of the product • Determine methods and procedures for production distribution activity • Create documentation and work instructions for production and distribution • Manage resources and maintain schedule requirements -

Ergonomic Challenges for Nanotechnology Safety and Health
of Ergo al no rn m u ic o s J Kim, J Ergonomics 2016, 6:5 Journal of Ergonomics DOI: 10.4172/2165-7556.1000e160 ISSN: 2165-7556 Editorial Open Access Ergonomic Challenges for Nanotechnology Safety and Health Practices In-Ju Kim Department of Industrial Engineering and Engineering Management, College of Engineering, University of Sharjah, PO Box 27272, Sharjah, United Arab Emirates Corresponding author: In-Ju Kim, Department of Industrial Engineering and Engineering Management, College of Engineering, University of Sharjah, PO Box 27272, Sharjah, United Arab Emirates, Tel: 0501340498; E-mail: [email protected] Received date: July 27, 2016; Accepted date: July 30, 2016; Published date: July 31, 2016 Copyright: ©2016 Kim IJ et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Introduction These tiny-sized substances are known as nanomaterials and could be either natural or anthropogenic in their origins [9]. Nanotechnology Nanotechnology has been broadly introduced to a wide range of involves the manipulation of matter on nanometer scales and offers the industry fields such as aeronautics, agriculture, architectural design, potential for unparalleled improvements in many different areas [11]. bio-medical engineering, communication sciences, constructions, The capability to operate matters at the atomic or molecular level environmental science, food production, and information technology makes it possible to form new materials, structures, and devices that over the last decades [1-4]. Nanotechnology has the perspective to develop exclusive physical and chemical properties related to nanoscale radically advance the efficiency of current industries and industrial structures. -
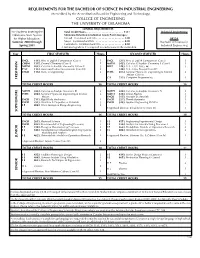
Requirements for the Bachelor of Science In
REQUIREMENTS FOR THE BACHELOR OF SCIENCE IN INDUSTRIAL ENGINEERING (Accredited by the Accreditation Board for Engineering and Technology) COLLEGE OF ENGINEERING THE UNIVERSITY OF OKLAHOMA GENERAL REQUIREMENTS For Students Entering the Total Credit Hours .......................... 131• Industrial Engineering Oklahoma State System Minimum Retention/Graduation Grade Point Averages: for Higher Education: Overall - Combined and OU ....................2.00 0913A Summer 2000 through Major - Combined and OU ....................2.00 Bachelor of Science in Spring 2001 Curriculum - Combined and OU .................2.00 Industrial Engineering A minimum grade of C is required for each course in the curriculum. Year FIRST SEMESTER Hours SECOND SEMESTER Hours ENGL 1113, Prin. of English Composition (Core I) 3 ENGL 1213, Prin. of English Composition (Core I) 3 CHEM 1315, General Chemistry (Core II) 5 MATH 2423, Calculus & Analytic Geometry II (Core I) 3 MATH 1823, Calculus & Analytic Geometry I (Core I) 3 HIST 1483, U.S., 1492-1865, or 3 P SC 1113, American Federal Government (Core III) 3 1493, U.S., 1865-Present (Core IV) ENGR 1112, Intro. to Engineering 2 PHYS 2514, General Physics for Engineering & Science 4 Majors (Core II) C S 1313, Computer Programming 3 FRESHMAN TOTAL CREDIT HOURS 16 TOTAL CREDIT HOURS 16 MATH 2433, Calculus & Analytic Geometry III 3 MATH 2443, Calculus & Analytic Geometry IV 3 PHYS 2524, General Physics for Engineering & Science 4 MATH 3333, Linear Algebra 3 Majors ENGR 2153, Strength of Materials 3 ENGR 2113, Rigid Body Mechanics -

Information Technology and Business Process Redesign
-^ O n THE NEW INDUSTRIAL ENGINEERING: INFORMATION TECHNOLOGY AND BUSINESS PROCESS REDESIGN Thomas H. Davenport James E. Short CISR WP No. 213 Sloan WP No. 3190-90 Center for Information Systems Research Massachusetts Institute of Technology Sloan School of Management 77 Massachusetts Avenue Cambridge, Massachusetts, 02139-4307 THE NEW INDUSTRIAL ENGINEERING: INFORMATION TECHNOLOGY AND BUSINESS PROCESS REDESIGN Thomas H. Davenport James E. Short June 1990 CISR WP No. 213 Sloan WP No. 3190-90 ®1990 T.H. Davenport, J.E. Short Published in Sloan Management Review, Summer 1990, Vol. 31, No. 4. Center for Information Systems Research ^^** ^=^^RfF§ - DP^/i/gy Sloan School of Management ^Ti /IPf?i *''*'rr r .. Milw.i.l. L T*' Massachusetts Institute of Technology j LIBRARJP.'Bh.^RfES M 7 2000 RECBVED The New Industrial Engineering: Information Technology and Business Process Redesign Thomas H. Davenport James E. Shon Emsi and Young MIT Sloan School of Management Abstract At the turn of the century, Frederick Taylor revolutionized the design and improvement of work with his ideas on work organization, task decomposition and job measurement. Taylor's basic aim was to increase organizational productivity by applying to human labor the same engineering principles that had proven so successful in solving technical problems in the workplace. The same approaches that had transformed mechanical activity could also be used to structure jobs performed by people. Taylor, rising from worker to chief engineer at Midvale Iron Works, came to symbolize the ideas and practical realizations in industry that we now call industrial engineering (EE), or the scientific school of management^ In fact, though work design remains a contemporary IE concern, no subsequent concept or tool has rivaled the power of Taylor's mechanizing vision. -

Introduction to Industrial Engineering
INTRODUCTION TO INDUSTRIAL ENGINEEING Industrial Engineering Definition Industrial Engineers plan, design, implement and manage integrated production and service delivery systems that assure performance, reliability, maintainability, schedule adherence and cost control Development of I. E. from Turner, Mize and Case, “Introduction to Industrial and Systems Engineering” I. E. History from Turner, Mize and Case, “Introduction to Industrial and Systems Engineering” U.S. Engineering Jobs from 2003 BLS % of Eng. Jobs % Growth (2012) • Electrical 19.8% 3-9% • Civil and Environmental 18.6% 3 -9% • Mechanical 14.5% 3-9% • Industrial 13.1% 10-20% •All Others <5.0% IE Prospects • Industrial engineers are expected to have employment growth of 14 percent over the projections decade, faster than the average for all occupations. As firms look for new ways to reduce costs and raise productivity, they increasingly will turn to industrial engineers to develop more efficient processes and reduce costs, delays, and waste. This focus should lead to job growth for these engineers, even in some manufacturing industries with declining employment overall. Because their work is similar to that done in management occupations, many industrial engineers leave the occupation to become managers. Numerous openings will be created by the need to replace industrial engineers who transfer to other occupations or leave the labor force. US Engineering Employment 2008 Civil engineers 278,400 Mechanical engineers 238,700 Industrial engineers 214,800 Electrical engineers 157,800 -

Catastrophic Household Expenditure for Healthcare in Turkey: Clustering Analysis of Categorical Data
data Article Catastrophic Household Expenditure for Healthcare in Turkey: Clustering Analysis of Categorical Data Onur Dogan 1,* , Gizem Kaya 2, Aycan Kaya 3 and Hidayet Beyhan 2 1 Department of Industrial Engineering, Izmir Bakircay University, Izmir 35665, Turkey 2 Department of Management Engineering, Istanbul Technical University, Istanbul 34367, Turkey 3 Department of Industrial Engineering, Istanbul Technical University, Istanbul 34367, Turkey * Correspondence: [email protected] Received: 24 June 2019; Accepted: 27 July 2019; Published: 29 July 2019 Abstract: The amount of health expenditure at the household level is one of the most basic indicators of development in countries. In many countries, health expenditure increases relative to national income. If out-of-pocket health spending is higher than the income or too high, this indicates an economical alarm that causes a lower life standard, called catastrophic health expenditure. Catastrophic expenditure may be affected by many factors such as household type, property status, smoking and drinking alcohol habits, being active in sports, and having private health insurance. The study aims to investigate households with respect to catastrophic health expenditure by the clustering method. Clustering enables one to see the main similarity and difference between the groups. The results show that there are significant and interesting differences between the five groups. C4 households earn more but spend less money on health problems by the rate of 3.10% because people who do physical exercises regularly have fewer health problems. A household with a family with one adult, landlord and three people in total (mother or father and two children) in the cluster C5 earns much money and spends large amounts for health expenses than other clusters. -

Risk Management – an Area of Knowledge for All Engineers
RISK MANAGEMENT – AN AREA OF KNOWLEDGE FOR ALL ENGINEERS A Discussion Paper By: Paul R. Amyotte, P.Eng.1 & Douglas J. McCutcheon, P.Eng.2 1Chemical Engineering Program Department of Process Engineering & Applied Science Dalhousie University Halifax, Nova Scotia, Canada B3J 2X4 <[email protected]> 2Industrial Safety & Loss Management Program Faculty of Engineering University of Alberta Edmonton, Alberta, Canada T6G 2G6 <[email protected]> Prepared For: The Research Committee of the Canadian Council of Professional Engineers October 2006 SUMMARY The purpose of this paper is to “seed” the discussion by the Research Committee of the Canadian Council of Professional Engineers (CCPE) on the topic of risk management. The paper is in part a research paper and in its entirety a position paper. As can be inferred from the title, the authors hold the firm opinion that risk management is an area of knowledge with which all engineers should have familiarity and a level of competence according to their scope of practice. The paper first makes the distinction between hazard and risk. The two terms are often used interchangeably when in fact they are quite different. A hazard is a chemical or physical condition that has the potential to cause harm or damage to people, environment, assets or production. Risk, on the other hand, is the possibility or chance of harm arising from a hazard; risk is a function of probability and severity of consequences. A description of the process of risk management is then given. A generic framework for risk management is presented to illustrate the essential activities of hazard identification and the analysis, assessment and management of risks. -

Supreme Court of the United States
No. 17-1104 IN THE Supreme Court of the United States AIR AND LIQUID SYSTEMS CORP., et al., Petitioners, v. ROBERTA G. DEVRIES, INDIVIDUALLY AND AS ADMINISTRATRIX OF THE ESTATE OF JOHN B. DEVRIES, DECEASED, et al., Respondents. –––––––––––––––––––––––––––––– INGERSOLL RAND COMPANY , Petitioner, v. SHIRLEY MCAFEE, EXECUTRIX OF THE ESTATE OF KENNETH MCAFEE, AND WIDOW IN HER OWN RIGHT, Respondent. ON WRIT OF CERTIORARI TO THE UNITED STATES CouRT OF APPEALS FOR THE THIRD CIRcuIT BRIEF FOR RESPONDENTS DENYSE F. CLANCY RicHARD P. MYERS KAZAN, MCCLAIN, SATTERLEY Counsel of Record & GREENWOOD ROBERT E. PAUL 55 Harrison Street, Suite 400 ALAN I. REicH Oakland, CA 94607 PATRick J. MYERS (877) 995-6372 PAUL, REicH & MYERS, P.C. [email protected] 1608 Walnut Street, Suite 500 Philadelphia, PA 19103 (215) 735-9200 [email protected] Counsel for Respondents (Additional Counsel Listed on Inside Cover) 281732 JONATHAN RUckdESCHEL WILLIAM W.C. HARTY THE RUckdESCHEL LAW PATTEN, WORNOM, HATTEN FIRM, LLC & DIAMONSTEIN 8357 Main Street 12350 Jefferson Avenue, Ellicott City, MD 21043 Suite 300 (410) 750-7825 Newport News, VA 23602 [email protected] (757) 223-4500 [email protected] Counsel for Respondents i QUESTION PRESENTED Under general maritime negligence law, does a manufacturer have a duty to warn users of the known hazards arising from the expected and intended use of its own product? ii TABLE OF CONTENTS Page QUESTION PRESENTED .......................i TABLE OF CONTENTS......................... ii TABLE OF APPENDICES .....................viii TABLE OF CITED AUTHORITIES ...............x INTRODUCTION ...............................1 COUNTER STATEMENT OF THE CASE .........6 A. Respondents were exposed to asbestos during the expected and intended use of petitioners’ machines ..................6 1. -

Design of a Self-Audit Tool for the Application of Lockout on Machinery in the Province of Quebec, Canada to Control Hazardous Energies
safety Article Design of a Self-Audit Tool for the Application of Lockout on Machinery in the Province of Quebec, Canada to Control Hazardous Energies Benyamin Karimi 1,* , Damien Burlet-Vienney 2, Yuvin Chinniah 1 and Barthelemy Aucourt 1 1 Department of Mathematics and Industrial Engineering, Polytechnique Montreal, P.O. Box 6079, Station Centre-ville, Montreal, QC H3C 3A7, Canada 2 Department of Mechanical and Physical Risk Prevention, Institut de recherche Robert-Sauvé en santé et en sécurité du travail (IRSST), 505 De Maisonneuve Blvd. West, Montreal, QC H3A 3C2, Canada * Correspondence: [email protected]; Tel.: +1-514-340-5121 (ext. 2271) Received: 13 June 2019; Accepted: 9 August 2019; Published: 13 August 2019 Abstract: Failure to apply lockout procedures for the control of hazardous energies is one of the main causes of machinery-related fatal and serious injuries in North America. The absence of audits of lockout or the lack of proper tools for auditing lockout is prevalent, and thus the application of lockout is often not fully in compliance with standards and regulations. A self-audit tool for the application of lockout procedures for machinery was developed on the basis of the current standards and regulations, and previous research. The tool was then tested for content validity through experts’ opinions and qualitative feedback from six organizations in the province of Quebec in Canada. The developed audit tool defines the actual procedures to audit, as well as the surrounding conditions that are needed and the prerequisites based on standards, regulations, and findings from previous research. The results showed that the tool displayed a high content validity index and demonstrated that the usability, applicability, and comprehensiveness of the tool were adequate. -

Industrial Engineering and Operations Research 1
Industrial Engineering and Operations Research 1 the paper-and-pencil test, or an IELTS Band score of at least 7 on a Industrial Engineering 9-point scale (note that individual programs may set higher levels for any of these); and and Operations 4. Sufficient undergraduate training to do graduate work in the given Research field. Applicants Who Already Hold a Graduate Degree The Department of Industrial Engineering and Operations Research The Graduate Council views academic degrees not as vocational training (IEOR) offers three graduate programs: a Master of Engineering certificates, but as evidence of broad training in research methods, (MEng), a Master of Science (MS), and a PhD. These programs have independent study, and articulation of learning. Therefore, applicants who been developed to meet the needs of individuals with backgrounds in already have academic graduate degrees should be able to pursue new engineering or the mathematical sciences who wish to enhance their subject matter at an advanced level without the need to enroll in a related knowledge of the theory, development, and use of quantitative models for or similar graduate program. design, analysis, risk management, and decision-making. This knowledge Programs may consider students for an additional academic master’s or applies to complex systems in the industrial, service, or public sectors, professional master’s degree only if the additional degree is in a distinctly including energy systems, supply chains, healthcare systems, and different field. financial systems. Students may concentrate on theoretical studies in preparation for doctoral-level research, or on applications of state-of-the- Applicants admitted to a doctoral program that requires a master’s degree art techniques to real world problems. -

NIOSH Research and Demonstration Grants. Fiscal Year 1993 Pdf Icon[PDF – 11.6
NIOSH RESEARCH AND DEMONSTRATION GRANTS FISCAL YEAR 1993 NICl5M U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Centers for Disease Control and Prevention National Institute for Occupational Safety and Health Atlanta, Georgia 30333 August 1994 DISCLAIMER Mention of company names or products does not constitute endorsement by the National Institute for Occupational Safety and Health. DliHS(NIOSH} Publication No. 94-131 ii FOREWORD The National Institute for Occupational Safety and Health (NIOSH) is mandated by the provisions of the Occupational Safety and Health Act of 1970 and the Federal Mine Safety and Health Amendments Act of 1977 to conduct research and demonstrations relating to occupational safety and health. Our overall goal is the prevention of illnesses, injuries, and deaths. Recognizing the valuable contributions of extramural scientists to this endeavor, NIOSH sponsors outstanding research through a grants program, which complements the lnstitute's intramural research program. The creativity and special resources available in the scientific community make the grants program a key component in achieving the Nation's goal to have safe jobs and healthy workers. We anticipate an expanded extramural research program in the coming years. To maximize the grants program's usefulness in protecting workers, NIOSH funds projects that are scientifically sound and related to program priorities. We are interested in funding grants that will ultimately be of practical value in solving workplace problems. This report provides a readily available source of information on the status and scope of the research grants program of NIOSH (all active grants during fiscal year 1993: October 1, 1992, to September 30, 1993).