Mechanism of Action Pharmacokinetics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1: Clinical Pharmacokinetics 1
1: CLINICAL PHARMACOKINETICS 1 General overview: clinical pharmacokinetics, 2 Pharmacokinetics, 4 Drug clearance (CL), 6 Volume of distribution (Vd), 8 The half-life (t½), 10 Oral availability (F), 12 Protein binding (PB), 14 pH and pharmacokinetics, 16 1 Clinical pharmacokinetics General overview General overview: clinical pharmacokinetics 1 The ultimate aim of drug therapy is to achieve effi cacy without toxicity. This involves achieving a plasma concentration (Cp) within the ‘therapeutic window’, i.e. above the min- imal effective concentration (MEC), but below the minimal toxic concentration (MTC). Clinical pharmacokinetics is about all the factors that determine variability in the Cp and its time-course. The various factors are dealt with in subsequent chapters. Ideal therapeutics: effi cacy without toxicity Minimum Toxic Concentration (MTC) Ideal dosing Minimum Effective Concentration (MEC) Drug concentration Time The graph shows a continuous IV infusion at steady state, where the dose-rate is exactly appropriate for the patient’s clearance (CL). Inappropriate dosing Dosing too high in relation to the patient’s CL – toxicity likely Minimum Toxic Concentration (MTC) Minimum Effective Concentration (MEC) Dosing too low in relation to the Drug concentration patient’s CL – drug may be ineffective Time Some reasons for variation in CL Low CL High CL Normal variation Normal variation Renal impairment Increased renal blood fl ow Genetic poor metabolism Genetic hypermetabolism Liver impairment Enzyme induction Enzyme inhibition Old age/neonate 2 General overview Clinical Pharmacokinetics Pharmacokinetic factors determining ideal therapeutics If immediate effect is needed, a loading dose (LD) must be given to achieve a desired 1 concentration. The LD is determined by the volume of distribution (Vd). -

Pharmacokinetics, Biodistribution, and Pharmacodynamics of Drug Delivery Systems
JPET Fast Forward. Published on March 5, 2019 as DOI: 10.1124/jpet.119.257113 This article has not been copyedited and formatted. The final version may differ from this version. JPET # 257113 Title: Pharmacokinetic and Pharmacodynamic Properties of Drug Delivery Systems Authors: Patrick M. Glassman, Vladimir R. Muzykantov Affiliation: Department of Systems Pharmacology and Translational Therapeutics, Perelman School of Medicine, University of Pennsylvania Address: 3400 Civic Center Boulevard, Bldg 421, Philadelphia, Pennsylvania 19104-5158, United States Downloaded from jpet.aspetjournals.org at ASPET Journals on September 24, 2021 1 JPET Fast Forward. Published on March 5, 2019 as DOI: 10.1124/jpet.119.257113 This article has not been copyedited and formatted. The final version may differ from this version. JPET # 257113 Running Title: PK/PD Properties of Drug Delivery Systems Corresponding Authors: Vladimir R. Muzykantov ([email protected], (215) 898-9823) and Patrick M. Glassman ([email protected]) # of Text Pages: 22 # of Tables: 2 # of Figures: 4 Word Count – Abstract: 144 Word Count – Introduction: 350 Word Count – Discussion: N/A Downloaded from Non-Standard Abbreviations: Absorption, Distribution, Metabolism, and Elimination (ADME) Biodistribution (BD) Drug Delivery Systems (DDSs) Enhanced Permeability & Retention (EPR) jpet.aspetjournals.org Gastrointestinal (GI) Intravenously (IV) Neonatal Fc Receptor (FcRn) Monoclonal Antibody (mAb) Reticuloendothelial System (RES) at ASPET Journals on September 24, 2021 Pharmacodynamics (PD) Pharmacokinetics (PK) Physiologically-Based Pharmacokinetic (PBPK) Subcutaneously (SC) Target-Mediated Drug Disposition (TMDD) Recommended Section: Drug Discovery and Translational Medicine 2 JPET Fast Forward. Published on March 5, 2019 as DOI: 10.1124/jpet.119.257113 This article has not been copyedited and formatted. -

Clinical Pharmacology 1: Phase 1 Studies and Early Drug Development
Clinical Pharmacology 1: Phase 1 Studies and Early Drug Development Gerlie Gieser, Ph.D. Office of Clinical Pharmacology, Div. IV Objectives • Outline the Phase 1 studies conducted to characterize the Clinical Pharmacology of a drug; describe important design elements of and the information gained from these studies. • List the Clinical Pharmacology characteristics of an Ideal Drug • Describe how the Clinical Pharmacology information from Phase 1 can help design Phase 2/3 trials • Discuss the timing of Clinical Pharmacology studies during drug development, and provide examples of how the information generated could impact the overall clinical development plan and product labeling. Phase 1 of Drug Development CLINICAL DEVELOPMENT RESEARCH PRE POST AND CLINICAL APPROVAL 1 DISCOVERY DEVELOPMENT 2 3 PHASE e e e s s s a a a h h h P P P Clinical Pharmacology Studies Initial IND (first in human) NDA/BLA SUBMISSION Phase 1 – studies designed mainly to investigate the safety/tolerability (if possible, identify MTD), pharmacokinetics and pharmacodynamics of an investigational drug in humans Clinical Pharmacology • Study of the Pharmacokinetics (PK) and Pharmacodynamics (PD) of the drug in humans – PK: what the body does to the drug (Absorption, Distribution, Metabolism, Excretion) – PD: what the drug does to the body • PK and PD profiles of the drug are influenced by physicochemical properties of the drug, product/formulation, administration route, patient’s intrinsic and extrinsic factors (e.g., organ dysfunction, diseases, concomitant medications, -

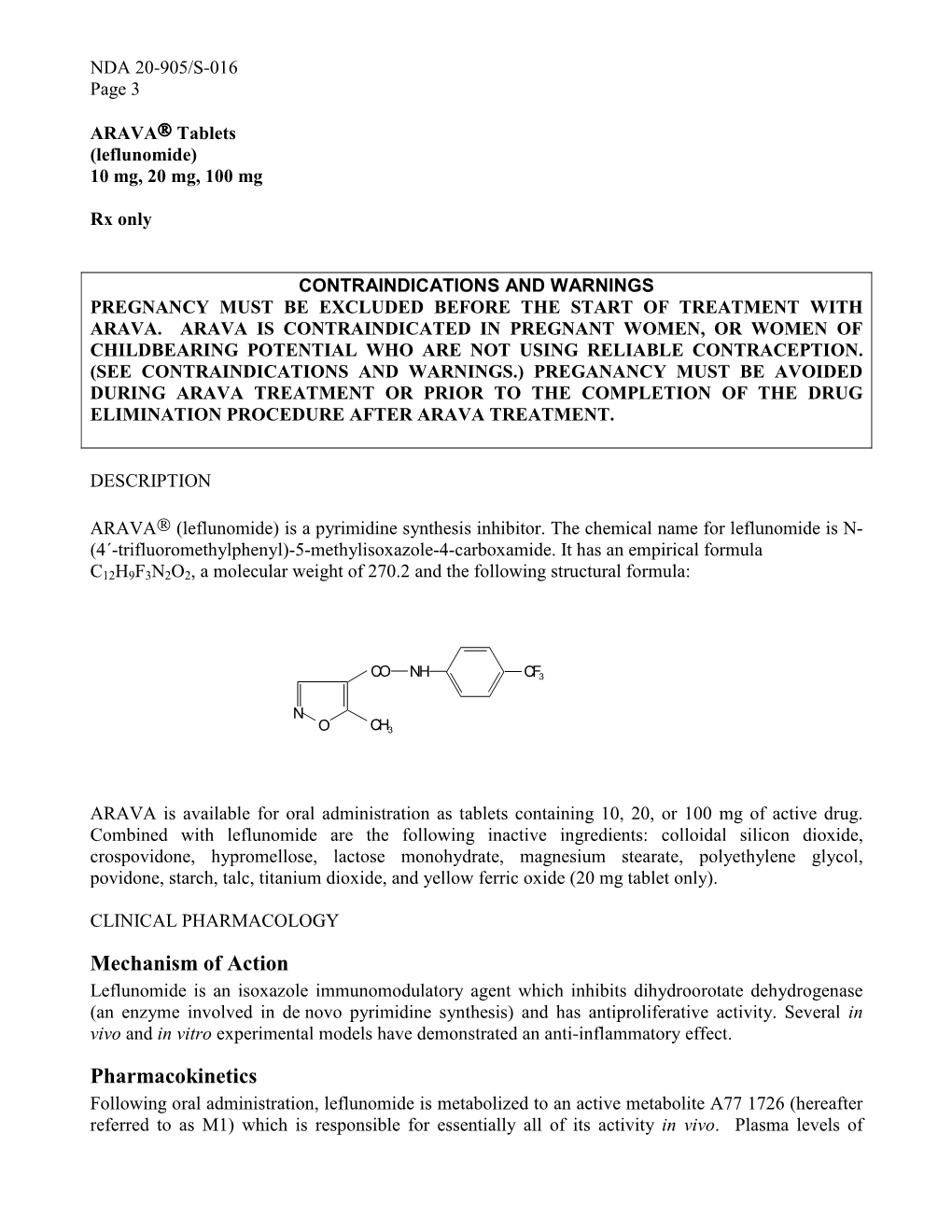
DESCRIPTION CLINICAL PHARMACOLOGY Mechanism Of
NDA 20-844/ Topamav Sprinkle Capsules Approved Labeling Text Version: 10/26/98 DESCRIPTION Topiramate is a sulfamate-substituted monosaccharide that is intended for use as an antiepileptic drug. TOPAMAX@ (topiramate capsules) Sprinkle Capsules are available as I5 mg, 25 mg and 50mg sprinkle capsules for oral administration as whole capsules or for opening and sprinkling onto soft food. Topiramate is a white crystalline powder with a bitter taste. Topiramate is most soluble in alkaline solutions containing sodium hydroxide or sodium phosphate and hawng a pH of 9 to IO. It is freely soluble in acetone, chloroform, dimethylsulfoxide, and ethanol. The solubility in water is 9.8 mg/mL. Its saturated solution has a pH of 6.3. Topiramate has the molecular formula C,,H,,NO,S and a molecular weight of 339.37. Topiramate is designated chemically as 2,3:4,5-Di-O-isopropylidene-~- D-fructopyranose sulfamate and has the following structural formula: H3C CH3 TOPAMAX” (topiramate capsules) Sprinkle Capsules contain topiramate coated beads in a hard gelatin capsule. The inactive ingredients are: sugar spheres (sucrose and starch), povidone, cellulose acetate, gelatin, silicone dioxide, sodium lauryl sulfate, titanium dioxide, and black pharmaceutical ink. CLINICAL PHARMACOLOGY Mechanism of Action: The precise mechanism by which topiramate exerts its antiseizure effect is unknown; however, electrophysiological and biochemical studies of the effects of topiramate on cultured neurons have revealed three properties that may contribute to topiramate’s antiepileptic efficacy. First, action potentials elicited repetitively by a sustained depolarization of the neurons are blocked by topiramate in a time-dependent manner, suggestive of a state-dependent sodium channel blocking action. -

Moving Beyond Single Gene-Drug Pairs in Clinical Pharmacogenomics Testing
Moving Beyond Single Gene-Drug Pairs in Clinical Pharmacogenomics Testing Yuan Ji, PhD, DABCP, FACMG Gwendolyn McMillin, PhD, DABCC Learning Objectives • Describe the strengths and limitations of pharmacogenomic testing. • List examples of single gene-drug associations with the strongest levels of evidence for clinical implementation. • Discuss cautions when considering the use of multi-gene drug associations to inform drug therapy decisions. 2 Disclosure • None 3 Outline • Singe gene-drug based pharmacogenomics (PGx) testing – An introduction – Evidence and examples – Considerations for developing and evaluating clinical PGx laboratory developed tests (LDTs) • Multi-gene PGx panels – Evidence and examples – PROs and CONs for utilizing PGx panels – Considerations for successful PGx implementation 4 Single Gene-Drug Based PGx Testing Yuan Ji, PhD, DABCP, FACMG Medical Director of Genomics and Genetics; PGx, ARUP Laboratories Associate Professor (Clinical) of Pathology, University of Utah Medications: Myths and Facts • are~30% peoplenot take“one at least-size one medication fits all” within a 30-day period • Most medications cause adverse drug events (ADEs) • Some medications like antibiotics may do more harm than good • CDC statistics: – ~ 200,000 ADEs-related ER visits in pediatric population (17 years or younger) – ~ 450,000 ADEs-related ER visits in older adults (65 years or older) – Medications, e.g., anticoagulant warfarin • Many ADEs are preventable by closely supervising of dosing, blood tests (therapeutic drug monitoring, TDM), -

Immediately Dangerous to Life Or Health (IDLH) Value Profile: Butane
Butane CAS® No. 106-97-8 DEPARTMENT OF HEALTH AND HUMAN SERVICES Center for Disease Control and Prevention National Institute of Occupational Safety and Health This page intentionally left blank. Immediately Dangerous to Life or Health (IDLH) Value Profile Butane [CAS® No. 106-97-8] H3C CH3 DEPARTMENT OF HEALTH AND HUMAN SERVICES Centers for Disease Control and Prevention National Institute for Occupational Safety and Health This document is in the public domain and may be freely copied or reprinted. Disclaimer Mention of any company or product does not constitute endorsement by the National Institute for Occupational Safety and Health (NIOSH). In addition, citations to websites external to NIOSH do not constitute NIOSH endorsement of the sponsoring organizations or their programs or products. Furthermore, NIOSH is not responsible for the content of these websites. Ordering Information To receive this document or information about other occupational safety and health topics, contact NIOSH: Telephone: 1-800-CDC-INFO (1-800-232-4636) TTY: 1-888-232-6348 E-mail: [email protected] or visit the NIOSH ebsite at: www.cdc.gov/niosh For a monthly update on news at NIOSH, subscribe to NIOSH eNews by visiting www.cdc.gov/niosh/eNews. Suggested Citation NIOSH [2016]. Immediately dangerous to life or health (IDLH) value profile: butane. By Dotson GS, Maier A, Parker A, Haber L. Cincinnati, OH: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupa- tional Safety and Health, DHHS (NIOSH) Publication 2016-174. DHHS (NIOSH) Publication No. 2016-174 September 2016 ii IDLH Value Profile for Butane Foreword Chemicals are a ubiquitous component of the modern workplace. -

Multiple Drug Resistance: a Fast-Growing Threat
Review Article ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2019.21.003572 Multiple Drug Resistance: A Fast-Growing Threat Eremwanarue Aibuedefe Osagie1,2* and Shittu Hakeem Olalekan1 1Department of Plant Biology and Biotechnology, University of Benin, Nigeria 2Lahor Research Laboratories and Diagnostics Centre, Nigeria *Corresponding author: Eremwanarue Aibuedefe Osagie, Department of Plant Biology and Biotechnology, University of Benin, Nigeria ARTICLE INFO Abstract Received: September 03, 2019 The spread of antibiotic resistant bacteria is a growing problem and a public health Published: September 10, 2019 issue. Over the years, various genetic mechanisms concerned with antibiotic resistance have been identified to be natural and acquired resistance. The natural resistance Citation: Eremwanarue Aibuedefe Osag- ie, Shittu Hakeem Olalekan. Multiple Geneticinvolved Elements mutation [MGEs] via target such modification,as plasmid, transposon reduced permeability, and integrons efflux genetic system elements and Drug Resistance: A Fast-Growing Threat. on the other hand, acquired resistance via horizontal gene tranfer include Moblie Biomed J Sci & Tech Res 21(2)-2019. Integrons are widely distributed, especially in Gram-negative bacteria; they are carried BJSTR. MS.ID.003572. bythat Mobile can acquire, Genetic exchange, Elements and such express as plasmids, genes embeddedand transposons, within whichGene Cassettespromote [GC].their spread within bacterial communities and have been studied mainly in the clinical setting Keywords: Antibiotics; Multiple Drug for their involvement in antibiotic resistance, their role in the environment is now an Resistant Bacteria; Mobile Genetic increasing focus of attention. The aim of this review is to educate the populise about Element; Integrons Plasmid the mechanisms of multiple drug resistance bacteria isolates and the danger ahead if appropriate regulations are not put in place especially in developing country like Nigeria. -

Pharmacology Part 2: Introduction to Pharmacokinetics
J of Nuclear Medicine Technology, first published online May 3, 2018 as doi:10.2967/jnmt.117.199638 PHARMACOLOGY PART 2: INTRODUCTION TO PHARMACOKINETICS. Geoffrey M Currie Faculty of Science, Charles Sturt University, Wagga Wagga, Australia. Regis University, Boston, USA. Correspondence: Geoff Currie Faculty of Science Locked Bag 588 Charles Sturt University Wagga Wagga 2678 Australia Telephone: 02 69332822 Facsimile: 02 69332588 Email: [email protected] Foot line: Introduction to Pharmacokinetics 1 Abstract Pharmacology principles provide key understanding that underpins the clinical and research roles of nuclear medicine practitioners. This article is the second in a series of articles that aims to enhance the understanding of pharmacological principles relevant to nuclear medicine. This article will build on the introductory concepts, terminology and principles of pharmacodynamics explored in the first article in the series. Specifically, this article will focus on the basic principles associated with pharmacokinetics. Article 3 will outline pharmacology relevant to pharmaceutical interventions and adjunctive medications employed in general nuclear medicine, the fourth pharmacology relevant to pharmaceutical interventions and adjunctive medications employed in nuclear cardiology, the fifth the pharmacology related to contrast media associated with computed tomography (CT) and magnetic resonance imaging (MRI), and the final article will address drugs in the emergency trolley. 2 Introduction As previously outlined (1), pharmacology is the scientific study of the action and effects of drugs on living systems and the interaction of drugs with living systems (1-7). For general purposes, pharmacology is divided into pharmacodynamics and pharmacokinetics (Figure 1). The principle of pharmacokinetics is captured by philosophy of Paracelsus (medieval alchemist); “only the dose makes a thing not a poison” (1,8,9). -

Action and Resistance Mechanisms of Antibiotics: a Guide for Clinicians
J Anaesthesiol Clin Pharmacol. 2017 Jul-Sep; 33(3): 300–305. PMCID: PMC5672523 doi: 10.4103/joacp.JOACP_349_15: 10.4103/joacp.JOACP_349_15 PMID: 29109626 Action and resistance mechanisms of antibiotics: A guide for clinicians Garima Kapoor, Saurabh Saigal,1 and Ashok Elongavan2 Department of Microbiology, Gandhi Medical College, Bhopal, Madhya Pradesh, India 1Department of Trauma and Emergency, AIIMS, Bhopal, Madhya Pradesh, India 2Department of Critical Care Medicine, Columbia Asia Hospital, Bengaluru, Karnataka, India Address for correspondence: Dr. Garima Kapoor, Department of Microbiology, Gandhi Medical College, Bhopal, Madhya Pradesh, India. E-mail: [email protected] Copyright : © 2017 Journal of Anaesthesiology Clinical Pharmacology This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms. Abstract Infections account for a major cause of death throughout the developing world. This is mainly due to the emergence of newer infectious agents and more specifically due to the appearance of antimicrobial resistance. With time, the bacteria have become smarter and along with it, massive imprudent usage of antibiotics in clinical practice has resulted in resistance of bacteria to antimicrobial agents. The antimicrobial resistance is recognized as a major problem in the treatment of microbial infections. The biochemical resistance mechanisms used by bacteria include the following: antibiotic inactivation, target modification, altered permeability, and “bypass” of metabolic pathway. Determination of bacterial resistance to antibiotics of all classes (phenotypes) and mutations that are responsible for bacterial resistance to antibiotics (genetic analysis) are helpful. -

Molecular Targets of Pepper As Bioavailability Enhancer
OPEM www.opem.org Oriental Pharmacy and Experimental Medicine 2009 9(4), 269-276 DOI 10.3742/OPEM.2009.9.4.269 Molecular targets of pepper as bioavailability enhancer Priyanshee Gohil and Anita Mehta* Department of Pharmacology, LM College of Pharmacy, Navrangpura, Ahmedabad–380009, Gujarat, India Received for publication January 21, 2008; accepted March 20, 2009 SUMMARY Black pepper (family Piperaceae), is called king of spices because it is one of the oldest spice and alone accounts for about 35% of the world’s total spice trade. The pepper is used in Ayurvedic medicine for the treatment of various ailments particularly neurological, broncho-pulmonary and gastrointestinal disorders. Pepper has also been reported to have various pharmacological actions but recently, it is highlighted as a bioavailability enhancer. This results in higher plasma concentration of drugs, nutrients, ions and other xenobiotics, rendering them more bioavailable for physiological as well as pharmacological actions in the body. Numerous scientific studies reported that piperine; a main bioactive compound of pepper, is responsible for its bioavailability enhancing property. It’s a well known fact that pepper enhances bioavailability by inhibition of microsomal enzyme system but other mechanisms are also responsible to acts as a bioavailability enhancer. The brief overview of the mechanism of action of pepper as well as its applications as bioavailability enhancer is given in the present article. Key words: Piperine; Bioavailability enhancer INTRODUCTION and 3 - 5% (on dry weight basis) in P. nigrum Linn (black pepper) and P. longum Linn (long pepper) Pepper species present as one of the key component respectively. It is isolated from fruits and it is in many preparations and formulations in traditional absent in the leaves and stem of plants. -

Mechanism of Action Pharmacokinetics
NDA 21-748/S-002 Page 3 Glumetza ™, 500 mg (metformin hydrochloride extended release tablets) tablet, film coated, extended release DESCRIPTION GLUMETZA (metformin hydrochloride) extended release tablet is an oral antihyperglycemic drug used in the management of type 2 diabetes. Metformin hydrochloride (N,N- dimethylimidodicarbonimidic diamide hydrochloride) is not chemically or pharmacologically related to any other classes of oral antihyperglycemic agents. The structural formula of metformin hydrochloride (metformin HCl) is as shown: Metformin HCl is a white to off-white crystalline compound with a molecular formula of C4H11N5•HCl and a molecular weight of 165.63. Metformin HCl is freely soluble in water and is practically insoluble in acetone, ether, and chloroform. The pKa of metformin is 12.4. The pH of a 1% aqueous solution of metformin hydrochloride is 6.68. GLUMETZA tablets are modified release dosage forms that contain 500 mg or 1000 mg of metformin HCl. Each 500 mg tablet contains coloring, hypromellose, magnesium stearate, microcrystalline cellulose and polyethylene oxide. Each 1000 mg tablet contains crospovidone, dibutyl sebacate, ethylcellulose, glyceryl behenate, polyvinyl alcohol, polyvinylpyrrolidone, and silicon dioxide. GLUMETZA 500 and 1000 mg tablets both utilize polymer- based, oral drug delivery systems, which allow delivery of metformin HCl to the upper gastrointestinal (GI) tract. CLINICAL PHARMACOLOGY Mechanism of Action Metformin is an antihyperglycemic agent, which improves glucose tolerance in patients with type 2 diabetes, lowering both basal and postprandial plasma glucose. Its pharmacologic mechanisms of action are different from other classes of oral antihyperglycemic agents. Metformin decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilization. -

Pharmacokinetics and Pharmacology of Drugs Used in Children
Drug and Fluid Th erapy SECTION II Pharmacokinetics and Pharmacology of Drugs Used CHAPTER 6 in Children Charles J. Coté, Jerrold Lerman, Robert M. Ward, Ralph A. Lugo, and Nishan Goudsouzian Drug Distribution Propofol Protein Binding Ketamine Body Composition Etomidate Metabolism and Excretion Muscle Relaxants Hepatic Blood Flow Succinylcholine Renal Excretion Intermediate-Acting Nondepolarizing Relaxants Pharmacokinetic Principles and Calculations Atracurium First-Order Kinetics Cisatracurium Half-Life Vecuronium First-Order Single-Compartment Kinetics Rocuronium First-Order Multiple-Compartment Kinetics Clinical Implications When Using Short- and Zero-Order Kinetics Intermediate-Acting Relaxants Apparent Volume of Distribution Long-Acting Nondepolarizing Relaxants Repetitive Dosing and Drug Accumulation Pancuronium Steady State Antagonism of Muscle Relaxants Loading Dose General Principles Central Nervous System Effects Suggamadex The Drug Approval Process, the Package Insert, and Relaxants in Special Situations Drug Labeling Opioids Inhalation Anesthetic Agents Morphine Physicochemical Properties Meperidine Pharmacokinetics of Inhaled Anesthetics Hydromorphone Pharmacodynamics of Inhaled Anesthetics Oxycodone Clinical Effects Methadone Nitrous Oxide Fentanyl Environmental Impact Alfentanil Oxygen Sufentanil Intravenous Anesthetic Agents Remifentanil Barbiturates Butorphanol and Nalbuphine 89 A Practice of Anesthesia for Infants and Children Codeine Antiemetics Tramadol Metoclopramide Nonsteroidal Anti-infl ammatory Agents 5-Hydroxytryptamine