Crohn's Disease: Introduction
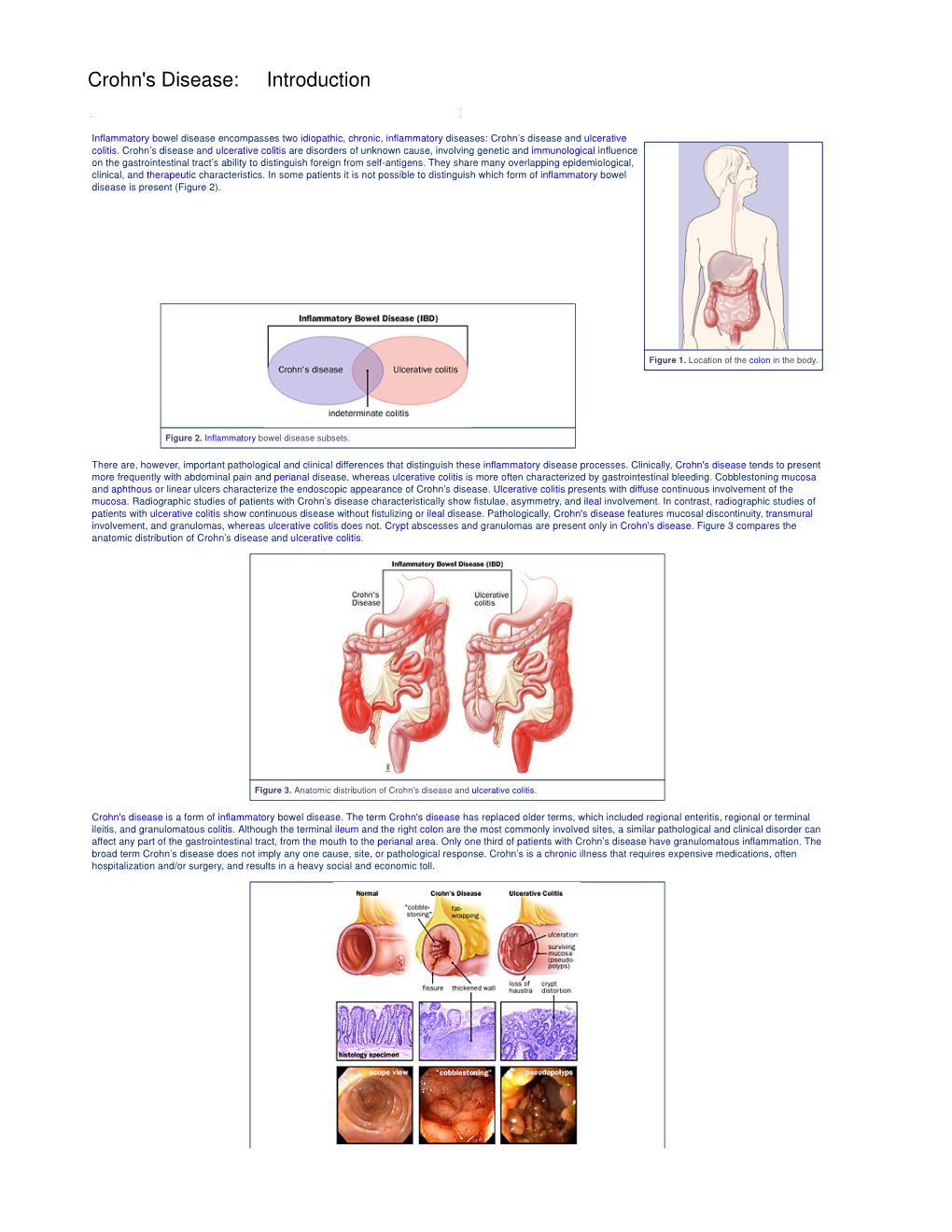
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Anatomy of the Rectum and Anal Canal
BASIC SCIENCE identify the rectosigmoid junction with confidence at operation. The anatomy of the rectum The rectosigmoid junction usually lies approximately 6 cm below the level of the sacral promontory. Approached from the distal and anal canal end, however, as when performing a rigid or flexible sigmoid- oscopy, the rectosigmoid junction is seen to be 14e18 cm from Vishy Mahadevan the anal verge, and 18 cm is usually taken as the measurement for audit purposes. The rectum in the adult measures 10e14 cm in length. Abstract Diseases of the rectum and anal canal, both benign and malignant, Relationship of the peritoneum to the rectum account for a very large part of colorectal surgical practice in the UK. Unlike the transverse colon and sigmoid colon, the rectum lacks This article emphasizes the surgically-relevant aspects of the anatomy a mesentery (Figure 1). The posterior aspect of the rectum is thus of the rectum and anal canal. entirely free of a peritoneal covering. In this respect the rectum resembles the ascending and descending segments of the colon, Keywords Anal cushions; inferior hypogastric plexus; internal and and all of these segments may be therefore be spoken of as external anal sphincters; lymphatic drainage of rectum and anal canal; retroperitoneal. The precise relationship of the peritoneum to the mesorectum; perineum; rectal blood supply rectum is as follows: the upper third of the rectum is covered by peritoneum on its anterior and lateral surfaces; the middle third of the rectum is covered by peritoneum only on its anterior 1 The rectum is the direct continuation of the sigmoid colon and surface while the lower third of the rectum is below the level of commences in front of the body of the third sacral vertebra. -

The Herbivore Digestive System Buffalo Zebra
The Herbivore Digestive System Name__________________________ Buffalo Ruminant: The purpose of the digestion system is to ______________________________ _____________________________. Bacteria help because they can digest __________________, a sugar found in the cell walls of________________. Zebra Non- Ruminant: What is the name for the largest section of Organ Color Key a ruminant’s Mouth stomach? Esophagus __________ Stomach Small Intestine Cecum Large Intestine Background Information for the Teacher Two Strategies of Digestion in Hoofed Mammals Ruminant Non‐ruminant Representative species Buffalo, cows, sheep, goats, antelope, camels, Zebra, pigs, horses, asses, hippopotamus, rhinoceros giraffes, deer Does the animal Yes, regurgitation No regurgitation regurgitate its cud to Grass is better prepared for digestion, as grinding Bacteria can not completely digest cell walls as chew material again? motion forms small particles fit for bacteria. material passes quickly through, so stool is fibrous. Where in the system do At the beginning, in the rumen Near the end, in the cecum you find the bacteria This first chamber of its four‐part stomach is In this sac between the two intestines, bacteria digest that digest cellulose? large, and serves to store food between plant material, the products of which pass to the rumination and as site of digestion by bacteria. bloodstream. How would you Higher Nutrition Lower Nutrition compare the nutrition Reaps benefits of immediately absorbing the The digestive products made by the bacteria are obtained via digestion? products of bacterial digestion, such as sugars produced nearer the end of the line, after the small and vitamins, via the small intestine. intestine, the classic organ of nutrient absorption. -

Report of Two Cases Presenting with Acute Abdominal Symptoms
Journal of Accident and Tension pneumothorax: report of two cases presenting J Accid Emerg Med: first published as 10.1136/emj.11.1.43 on 1 March 1994. Downloaded from Emergency Medicine 1993 with acute abdominal symptoms 10, 43-44 G.W. HOLLINS,1 T. BEATTIE,1 1. HARPER2 & K. LITTLE2 Departments of Accident and Emergency 1 Aberdeen Royal Infirmary, Foresterhill, Aberdeen and 2Royal Infirmary of Edinburgh, Lauriston Place, Edinburgh INTRODUCTION diagnoses were peptic ulcer disease or acute pancreatitis. Work-up appropriate to these diag- Tension pneumothorax constitutes a medical noses was commenced. An erect chest radiograph emergency and rapid diagnosis should be possible revealed a large pneumothorax with mediastinal on the basis of history and clinical examination. shift to the left. Following drainage using a large Following treatment with the delivery of high con- bore needle there was immediate resolution of his centration oxygen and the insertion of a large bore symptoms and all abdominal signs. An intercostal needle into the pleural space of the affected side, chest drain was formally sited and full expansion of the diagnosis can be confirmed radiologically and his right lung was achieved after 36 h. He was dis- an intercostal chest drain formally sited.1'2 We report charged home after 3 days. two cases where diagnosis was not made on the basis of history and examination alone. Both cases Case 2 presented with symptoms and signs suggestive of an acute intra-abdominal pathology and the diag- A 37-year-old male computer operator presented nosis was only made on radiological grounds. with a 1-week history of general malaise associated with mild neck and back pain. -

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

An Abdominal Tuberculosis Case Mimicking an Abdominal Mass Derya Erdog˘ Ana, Yasemin Tascı¸ Yıldızb, Esin Cengiz Bodurog˘ Luc and Naciye Go¨ Nu¨L Tanırd
Case report 81 An abdominal tuberculosis case mimicking an abdominal mass Derya Erdog˘ ana, Yasemin Tascı¸ Yıldızb, Esin Cengiz Bodurog˘ luc and Naciye Go¨ nu¨l Tanırd Abdominal tuberculosis is rare in childhood. It may be Departments of aPediatric Surgery, bRadiology, cPathology and dPediatric difficult to diagnose as it mimics various disorders. We Infectious Diseases, Dr Sami Ulus Maternity and Children’s Research and Training Hospital, Altındag˘ -Ankara, Turkey present a 12-year-old child with an unusual clinical Correspondence to Derya Erdog˘ an, Dr Sami Ulus Maternity and Children’s presentation who was diagnosed with abdominal Research and Training Hospital, Babu¨r caddesi No. 34 06080, tuberculosis only perioperatively. Ann Pediatr Surg Altındag˘ -Ankara, Turkey Tel: + 90 542 257 5522; fax: + 90 312 317 0353; 9:81–83 c 2013 Annals of Pediatric Surgery. e-mail: [email protected] Annals of Pediatric Surgery 2013, 9:81–83 Received 1 June 2012 accepted 3 January 2013 Keywords: abdominal tuberculosis, child, diagnosis Introduction hyperemia around the umbilicus. A mass with undefined Tuberculosis continues to be an important healthcare borders that filled the whole abdomen was present, and problem, especially in developing countries. Abdominal the paraumblical area was tender on palpation. The tuberculosis is quite rare and can present with different posteroanterior chest and plain abdominal radiographs clinical features in children compared with adults. It can showed nonspecific findings (Fig. 1). Abdominal ultra- be difficult to diagnose as it can mimic various abdominal sonography revealed stage 1 hydronephrosis, minimal diseases. splenomegaly, a multiloculated cystic, and a fine septated mass 51 Â 15 mm in size adjacent to the anterior border of Case report the liver and multiloculated cystic fine septated masses A 12-year-old boy presented with increasing abdominal 51 Â 38 mm in size adjacent to the pancreas inferiorly. -

Acute Gastroenteritis
Article gastrointestinal disorders Acute Gastroenteritis Deise Granado-Villar, MD, Educational Gap MPH,* Beatriz Cunill-De Sautu, MD,† Andrea In managing acute diarrhea in children, clinicians need to be aware that management Granados, MDx based on “bowel rest” is outdated, and instead reinstitution of an appropriate diet has been associated with decreased stool volume and duration of diarrhea. In general, drug therapy is not indicated in managing diarrhea in children, although zinc supplementation Author Disclosure and probiotic use show promise. Drs Granado-Villar, Cunill-De Sautu, and Objectives After reading this article, readers should be able to: Granados have disclosed no financial 1. Recognize the electrolyte changes associated with isotonic dehydration. relationships relevant 2. Effectively manage a child who has isotonic dehydration. to this article. This 3. Understand the importance of early feedings on the nutritional status of a child who commentary does has gastroenteritis. contain a discussion of 4. Fully understand that antidiarrheal agents are not indicated nor recommended in the an unapproved/ treatment of acute gastroenteritis in children. investigative use of 5. Recognize the role of vomiting in the clinical presentation of acute gastroenteritis. a commercial product/ device. Introduction Acute gastroenteritis is an extremely common illness among infants and children world- wide. According to the Centers for Disease Control and Prevention (CDC), acute diarrhea among children in the United States accounts for more than 1.5 million outpatient visits, 200,000 hospitalizations, and approximately 300 deaths per year. In developing countries, diarrhea is a common cause of mortality among children younger than age 5 years, with an estimated 2 million deaths each year. -

Mouth Esophagus Stomach Rectum and Anus Large Intestine Small
1 Liver The liver produces bile, which aids in digestion of fats through a dissolving process known as emulsification. In this process, bile secreted into the small intestine 4 combines with large drops of liquid fat to form Healthy tiny molecular-sized spheres. Within these spheres (micelles), pancreatic enzymes can break down fat (triglycerides) into free fatty acids. Pancreas Digestion The pancreas not only regulates blood glucose 2 levels through production of insulin, but it also manufactures enzymes necessary to break complex The digestive system consists of a long tube (alimen- 5 carbohydrates down into simple sugars (sucrases), tary canal) that varies in shape and purpose as it winds proteins into individual amino acids (proteases), and its way through the body from the mouth to the anus fats into free fatty acids (lipase). These enzymes are (see diagram). The size and shape of the digestive tract secreted into the small intestine. varies in each individual (e.g., age, size, gender, and disease state). The upper part of the GI tract includes the mouth, throat (pharynx), esophagus, and stomach. The lower Gallbladder part includes the small intestine, large intestine, The gallbladder stores bile produced in the liver appendix, and rectum. While not part of the alimentary 6 and releases it into the duodenum in varying canal, the liver, pancreas, and gallbladder are all organs concentrations. that are vital to healthy digestion. 3 Small Intestine Mouth Within the small intestine, millions of tiny finger-like When food enters the mouth, chewing breaks it 4 protrusions called villi, which are covered in hair-like down and mixes it with saliva, thus beginning the first 5 protrusions called microvilli, aid in absorption of of many steps in the digestive process. -

1311 Diploma in Medical Record Science Second
[LD 0212] AUGUST 2013 Sub. Code: 1311 DIPLOMA IN MEDICAL RECORD SCIENCE SECOND YEAR PAPER II – INTERNATIONAL CLASSIFICATION OF DISEASES (ICD-10) & SURGICAL PROCEDURES (ICM-9CM) Q.P. Code : 841311 Time : Three Hours Maximum : 100 marks Answer ALL questions I Write appropriate codes using ICD -10 (30 x 1 = 30) 1. Therapeutic introduction of hand tendon. 2. Excision of major partial thickness of eyelid excision. 3. Interphalangeal arthrodesis of Toe. 4. Division of percutaneous spinal cord nerve tracts. 5. Transfusion of allograft bone aetriosus. 6. Rastelli operation of truncus arteriosus. 7. Pyoloric sphincter dilatation. 8. Stapling of radius epiphyseal plate. 9. Suture of hands fascia. 10. Suture of hand fascia. 11. Repair of anterior wall (abdomen) hernia. 12. Foreign body removal without incision in t o the brain. 13. Repair of Tetrology of fallot. 14. Frontal Sinusectomy. 15. Urethral sling suspension. 16. Bone shaft transfer. 17. Coil of aneuryum repair. 18. Sling suspension. 19. Radio isotope scanning, pituitary gland. 20. Spinal shunt removal. 21. Acute lung edema. Due to external agent. 22. Proximal end tibial closed fracture was riding a two wheeler-slip & fell down. 23. Thrombosed internal hemorrhoids. 24. Secondary hypertension due to renal disorder. 25. Old myocardial infarction. 26. Fall from high place, injured elbow. 27. Chronic venous (peripheral) insufficiency. 28. Acute myeloid leukemia. 29. Post-operative intestine obstruction. 30. Abnormal pregnancy. II Writes appropriate codes using ICS-9CM (20 x 2 = 40) 1. Pregnant women suffering from acute salphingo oophoritis. 2. Accidental intake of ferrous salt. 3. Sprain of lumbar spine as stuck by another person. 4. -

Understanding the CBC
Understanding the CBC What is Hematology? Hematology is the science of blood and blood-forming tissues. Blood is made up of plasma and blood cells. Blood formation (hematopoesis) is a continuous process that occurs in the bone marrow. Within the bone marrow there is a pluripotent stem cell, the Mother Cell, the originator of all types of blood cells. The stem cell produces blood cells that exit the bone marrow and circulate in the blood system. Red cells circulate about four months, platelets last an average of ten days, and white cells range from only hours to a week or so. Stem cells that are found outside the bone marrow are called “peripheral stem cells” and are collected and frozen for stem cell transplants. What is a CBC? The CBC- the complete blood count, or the counts- is a lab test that will be ordered frequently on your child. This test determines the number, type, percentage, concentration and quality of the various types of blood cells that make up the blood. This test can be completed on blood that is collected by a finger stick, a lab draw from a central vein access and/or a straight draw from a peripheral vein, (usually from an arm, hand or foot). The CBC is commonly performed on an automated analyzer. However when abnormalities are noted in the blood, parts of the test can be completed manually. That is when the blood sample is viewed under the microscope. Some institutions commonly perform an extensively complete CBC and others may perform just specific aspects of the CBC. -

The Digestive System
Connective tissue The Digestive System Part 1 Structure of digestive system Functions Basic Structure of the Alimentary Canal Wall Tube is made up of four layers: 1. Mucosa 2. Submucosa 3. Muscularis externa 4. Serosa (Peritoneum) or Adventitia Mucosa The innermost wall of the alimentary tube. Consists of: • Epithelium - usually simple columnar epithelium with goblet cells; may be stratified squamous if protection is needed (e.g. esophagus) • Lamina propria – loose connective tissue • Muscularis mucosae – takes part in the formation of folds Submucosa Made up of loose connective tissue. Contains submucosal (Meissner’s) nervous plexus and blood vessels, sometimes glands. Muscularis externa Usually two layers of smooth muscle: • inner circular layer • outer longitudinal layer. • Myenteric (Auerbach’s) nervous plexus in between • Responsible for peristalsis (controlled by the nerve plexus) Outer membrane • A serous membrane/peritoneum consisting of the mesothelium (simple squamous epithelium), and a small amount of underlying loose connective tissue. • Or adventitia consisting only of connective tissue is found where the wall of the tube is directly attached or fixed to adjoining structures (i.e., body wall and certain organs). Enteric nervous system The Alimentary Canal Pharynx Common respiratory and digestive pathway (both air and swallowed food and drinks pass through). • Stratified squamous non-keratinized epithelium • Lamina propria contains many elastic fibers • No muscularis mucosae • No submucosa • Striated muscle in the muscularis externa Esophagus Fixed muscular tube that delivers food and liquid from the pharynx to the stomach. Esophagus Epithelium - stratified squamous Mucosal and submucosal glands of the esophagus secrete mucus to lubricate and protect the luminal wall. Esophageal glands proper lie in the submucosa. -

Medical Terminology Abbreviations Medical Terminology Abbreviations
34 MEDICAL TERMINOLOGY ABBREVIATIONS MEDICAL TERMINOLOGY ABBREVIATIONS The following list contains some of the most common abbreviations found in medical records. Please note that in medical terminology, the capitalization of letters bears significance as to the meaning of certain terms, and is often used to distinguish terms with similar acronyms. @—at A & P—anatomy and physiology ab—abortion abd—abdominal ABG—arterial blood gas a.c.—before meals ac & cl—acetest and clinitest ACLS—advanced cardiac life support AD—right ear ADL—activities of daily living ad lib—as desired adm—admission afeb—afebrile, no fever AFB—acid-fast bacillus AKA—above the knee alb—albumin alt dieb—alternate days (every other day) am—morning AMA—against medical advice amal—amalgam amb—ambulate, walk AMI—acute myocardial infarction amt—amount ANS—automatic nervous system ant—anterior AOx3—alert and oriented to person, time, and place Ap—apical AP—apical pulse approx—approximately aq—aqueous ARDS—acute respiratory distress syndrome AS—left ear ASA—aspirin asap (ASAP)—as soon as possible as tol—as tolerated ATD—admission, transfer, discharge AU—both ears Ax—axillary BE—barium enema bid—twice a day bil, bilateral—both sides BK—below knee BKA—below the knee amputation bl—blood bl wk—blood work BLS—basic life support BM—bowel movement BOW—bag of waters B/P—blood pressure bpm—beats per minute BR—bed rest MEDICAL TERMINOLOGY ABBREVIATIONS 35 BRP—bathroom privileges BS—breath sounds BSI—body substance isolation BSO—bilateral salpingo-oophorectomy BUN—blood, urea, nitrogen -

Vestibule Lingual Frenulum Tongue Hyoid Bone Trachea (A) Soft Palate
Mouth (oral cavity) Parotid gland Tongue Sublingual gland Salivary Submandibular glands gland Esophagus Pharynx Stomach Pancreas (Spleen) Liver Gallbladder Transverse colon Duodenum Descending colon Small Jejunum Ascending colon intestine Ileum Large Cecum intestine Sigmoid colon Rectum Appendix Anus Anal canal © 2018 Pearson Education, Inc. 1 Nasopharynx Hard palate Soft palate Oral cavity Uvula Lips (labia) Palatine tonsil Vestibule Lingual tonsil Oropharynx Lingual frenulum Epiglottis Tongue Laryngopharynx Hyoid bone Esophagus Trachea (a) © 2018 Pearson Education, Inc. 2 Upper lip Gingivae Hard palate (gums) Soft palate Uvula Palatine tonsil Oropharynx Tongue (b) © 2018 Pearson Education, Inc. 3 Nasopharynx Hard palate Soft palate Oral cavity Uvula Lips (labia) Palatine tonsil Vestibule Lingual tonsil Oropharynx Lingual frenulum Epiglottis Tongue Laryngopharynx Hyoid bone Esophagus Trachea (a) © 2018 Pearson Education, Inc. 4 Visceral peritoneum Intrinsic nerve plexuses • Myenteric nerve plexus • Submucosal nerve plexus Submucosal glands Mucosa • Surface epithelium • Lamina propria • Muscle layer Submucosa Muscularis externa • Longitudinal muscle layer • Circular muscle layer Serosa (visceral peritoneum) Nerve Gland in Lumen Artery mucosa Mesentery Vein Duct oF gland Lymphoid tissue outside alimentary canal © 2018 Pearson Education, Inc. 5 Diaphragm Falciform ligament Lesser Liver omentum Spleen Pancreas Gallbladder Stomach Duodenum Visceral peritoneum Transverse colon Greater omentum Mesenteries Parietal peritoneum Small intestine Peritoneal cavity Uterus Large intestine Cecum Rectum Anus Urinary bladder (a) (b) © 2018 Pearson Education, Inc. 6 Cardia Fundus Esophagus Muscularis Serosa externa • Longitudinal layer • Circular layer • Oblique layer Body Lesser Rugae curvature of Pylorus mucosa Greater curvature Duodenum Pyloric Pyloric sphincter antrum (a) (valve) © 2018 Pearson Education, Inc. 7 Fundus Body Rugae of mucosa Pyloric Pyloric (b) sphincter antrum © 2018 Pearson Education, Inc.