Correction of Abnormal Renal Blood Flow Response to Angiotensin II by Converting Enzyme Inhibition in Essential Hypertensives
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
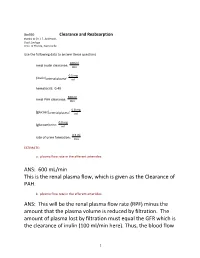
ANS: 600 Ml/Min This Is the Renal Plasma Flow, Which Is Given As the Clearance of PAH
Bio390 Clearance and Reabsorption thanks to Dr. J.F. Anderson, Dept Zoology Univ. of Florida, Gainesville Use the following data to answer these questions. 100 ml renal inulin clearance: min 0.5 mg [inulin]arterial plasma: ml hematocrit: 0.40 600 ml renal PAH clearance: min 0.8 mg [glucose]arterial plasma: ml 0.0 mg [glucose]urine: ml 0.5 ml rate of urine formation: min ESTIMATE: a. plasma flow rate in the afferent arterioles: ANS: 600 mL/min This is the renal plasma flow, which is given as the Clearance of PAH. b. plasma flow rate in the efferent arterioles: ANS: This will be the renal plasma flow rate (RPF) minus the amount that the plasma volume is reduced by filtration. The amount of plasma lost by filtration must equal the GFR which is the clearance of inulin (100 ml/min here). Thus, the blood flow 1 in the efferent arteriole is 600 - 100 ml/min = 500 ml/min in this problem c. plasma flow rate in the renal veins: ANS: by the time that blood enters the veins, nearly all of the water lost during filtration has made its way back to the blood (especially if the subject is dehydrated!). If urine is being formed at a rate of 0.5 mL/min, then that represents (essentially) the volume of water lost per min. So, the renal venous plasma flow rate = RPF- urine loss = 600 - 0.5 = 599.5 ml/min d. renal blood flow rate in renal artery in ml/min ANS: 833 mL/min the hct = 40% (0.4). -

Impaired Tubular Secretion of Organic Solutes in Acute Kidney Injury
Original Investigation Impaired Tubular Secretion of Organic Solutes in Acute Kidney Injury Frank J. O’Brien,1 Robert D. Mair,2,3 Natalie S. Plummer,2,3 Timothy W. Meyer,2,3 Scott M. Sutherland,4 and Tammy L. Sirich2,3 Abstract Background Impairment of kidney function is routinely assessed by measuring the accumulation of creatinine, an organic solute cleared largely by glomerular filtration. We tested whether the clearance of solutes that undergo tubular secretion is reduced in proportion to the clearance of creatinine in humans with AKI. Methods Four endogenously produced organic solutes (phenylacetylglutamine [PAG], hippurate [HIPP], indoxyl sulfate [IS], and p-cresol sulfate [PCS]) were measured in spot urine and plasma samples from ten patients with AKI and 17 controls. Fractional clearance relative to creatinine was calculated to assess tubular secretion. Fractional clearance values were calculated in terms of the free, unbound levels of HIPP, IS, and PCS that bind to plasma proteins. Results Fractional clearance values for PAG, HIPP, IS, and PCS were .1.0 in patients with AKI as well as controls, indicating that these solutes were still secreted by the tubules of the injured kidneys. Fractional clearance values were, however, significantly lower in patients with AKI than controls, indicating that kidney injury reduced tubular secretion more than glomerular filtration (AKI versus control: PAG, 2.160.7 versus 4.661.4, P,0.001; HIPP, 1065 versus 1567, P50.02; IS, 1066 versus 2867, P,0.001; PCS, 3.361.8 versus 1063, P,0.001). Free plasma levels rose out of proportion to total plasma levels for each of the bound solutes in AKI, so that calculating their fractional clearance in terms of their total plasma levels failed to reveal their impaired secretion. -

Production of Hypertonic Urine in the Absence of Pituitary Antidiuretic Hormone
Production of Hypertonic Urine in the Absence of Pituitary Antidiuretic Hormone Robert W. Berliner, Douglas G. Davidson J Clin Invest. 1957;36(10):1416-1427. https://doi.org/10.1172/JCI103541. Research Article Find the latest version: https://jci.me/103541/pdf PRODUCTION OF HYPERTONIC URINE IN THE ABSENCE OF PITUITARY ANTIDIURETIC HORMONE 1 BY ROBERT W. BERLINER AND DOUGLAS G. DAVIDSON 2 (From the Laboratory of Kidney and Electrolyte Metabolism, National Heart Institute, National Institutes of Health, Public Health Sertice, Department of Health, Education, and Welfare, Bethesda, Md.) (Submitted for publication May 1, 1957; accepted May 23, 1957) The mechanism by which pituitary antidiuretic permeability of the tubule membrane to water. hormone (ADH) produces its renal effect has The change to hypertonicity cannot be so readily not been clearly established. Under ordinary con- attributed to an effect on water permeability with- ditions, in the absence of ADH, urine of a con- out some assumptions as to the mechanism by centration considerably below that of plasma is which the hypertonicity is produced. However, produced in large volume. With increasing it is a reasonable hypothesis that the mechanism amounts of ADH, administered or secreted, the for the production of hypertonicity is not depen- osmotic pressure of the urine rises to and above dent upon ADH but that its effects are unmasked, that of plasma. With respect to total water bal- in the presence of ADH, by 1) changes in the vol- ance, the quantitatively more important contri- ume and concentration of urine delivered to it and, bution to water economy is the change between possibly, 2) changes in the permeability of the maximally dilute and isotonic urine, since this, in membranes separating the concentrating mecha- normal man, may involve a change in water ex- nism from the urine in the tubule lumen. -

A Compendium of Research
NASA TECHNICAL NASA TM X-3308 MEMORANDUM CO CO I X c PHYSIOLOGIC RESPONSES TO WATER IMMERSION IN MAN: A COMPENDIUM OF RESEARCH James Kollias, Dena Van Derveer, Karen J. Dorchak, and John E. Greenleaf Ames Research Center Moffett Field, Calif. 94035 ^ *" /V NATIONAL AERONAUTICS AND SPACE ADMINISTRATION • WASHINGTON, D. C. • FEBRUARY 1976 1. Report No. 2. Government Accession No. 3. Recipient's Catalog No. NASA TM X-3308 4. Title and Subtitle 5. Report Date February 1976 PHYSIOLOGIC RESPONSES TO WATER IMMERSION IN MAN: 6. Performing Organization Code A COMPENDIUM OF RESEARCH 7. Author(s) 8. Performing Organization Report No. A-6038 James Kollias, Dena Van Derveer, Karen J. Dorchak, and John E. Greenleaf 10. Work Unit No. 9. Performing Organization Name and Address 970-21-14-05 NASA Ames Research Center 11. Contract or Grant No. Moffett Field, Calif. 94035 13. Type of Report and Period Covered 12. Sponsoring Agency Name and Address Technical Memorandum National Aeronautics and Space Administration 14. Sponsoring Agency Code Washington, D. C. 20546 15. Supplementary Notes 16. Abstract Since the advent of space flight programs, scientists have been searching for ways to reproduce the zero-gravity effects of weightlessness. Brief periods of weightlessness up to 1 minute were feasible using Keplerian trajectory, but comprehen- sive study of the prolonged effects of the weightless state necessitated the development of other methods. Thus far the two approaches most widely used have been complete bedrest and fluid immersion. Surprisingly, these simulated environments have produced essentially all of the symptoms found in astronauts. This compendium contains reports appearing in the literature through December 1973. -

Renal Function in Mice: Effects of Volume Expansion and Angiotensin II
J Am Soc Nephrol 10: 2631–2636, 1999 Renal Function in Mice: Effects of Volume Expansion and Angiotensin II LUDEK CERVENKA,* KENNETH D. MITCHELL,† and L. GABRIEL NAVAR† *Department of Experimental Medicine, Institute for Clinical and Experimental Medicine, Prague, Czech Republic; and †Department of Physiology, Tulane University School of Medicine, New Orleans, Louisiana. Abstract. The present study was performed to validate a simple (83 6 2 mmHg), but led to significantly greater values in both means for assessing renal function in anesthetized mice and to GFR and RPF (1.35 6 0.14 versus 1.01 6 0.1 ml/min z g and characterize the renal hemodynamic responses to acute volume 11.26 6 1.39 versus 6.29 6 0.5 ml/min z g, respectively). expansion and how these responses are altered by concurrent Infusion of AngII during volume expansion led to significant angiotensin II (AngII) infusions. Inulin and para-aminohippu- elevations of MAP (100 6 3 mmHg, P , 0.05) and prevented rate clearances were used to assess GFR and renal plasma flow the increases in GFR and RPF elicited by volume expansion (RPF) in three groups of male C57Bl/6 mice anesthetized with (0.77 6 0.08 and 5.35 6 0.48 ml/min z g, respectively). inactin (100 mg/kg, intraperitoneally) and ketamine (10 mg/ Volume expansion also elicited marked increases in absolute kg). To avoid the hypotension associated with repeated blood and fractional sodium excretion (6.1 6 1.0 versus 0.62 6 0.2 sampling, a single blood sample was taken after three timed mEq/min z g and 3.1 6 0.7 versus 0.4 6 0.1%, respectively). -

A Didactic Approach to Renal Clearance
A Didactic Approach to Renal Clearance Vander Baptista, PhD Department of Physiological Sciences, Centre of Biological Sciences, Federal University of Santa Catarina, 88040-970 Florianópolis, SC – Brazil [email protected] Abstract Renal clearance encompasses a somewhat abstract concept, which makes it a hard-to-visualize phenomenon. It is a confusing topic for students and a difficult task for the instructor to teach. In order to improve or facilitate the teaching-learning process of renal clearance, an alternative strategy is presented here. To properly characterize the components of renal clearance, this didactic model splits renal clearance into two distinct portions of flow rates. The information is organized in a sequential structure, from the simplest ideas to the most complex concepts, assisting both teacher and student in addressing renal clearance. https://doi.org/10.21692/haps.2020.022 Key words: renal clearance, didactic model, cumulative sequence, renal physiology, kidney Introduction The clearance methods are a useful way to quantify the The renal excretion rate of a substance S (ERS) is the amount glomerular filtration rate, tubular reabsorption, and tubular of S removed from the body by the kidneys per unit of time secretion (Hall and Guyton 2011). In a broader vision, as (mg/min). By using the same reasoning, it can be written pointed out by Dr. Donald W. Seldin: “The clearance concept ERS = x US, where is the urinary excretion rate (urinary is central to three critical areas of nephrology”; it was a key volume per unit of time) and US is the concentration of S in feature for understanding the nature of urine formation, for the urine. -

Tion, UV, in the Clearance Calculation, Ie, IV/P = Ously by the Infusion Technique, and on the Appli
COMPARISON OF THE CONSTANT INFUSION AND URINE COLLECTION TECHNIQUES FOR THE MEASUREMENT OF RENAL FUNCTION 1 BY EUGENE Y. BERGER, SAUL J. FARBER, AND DAVID P. EARLE, JR. WITH THE TECHNICAL ASSISTANCE OF ROSALYN JACKENTHAL (From the Third [New York University] Research Service, Goldwater Memorial Hospital, and the Department of Medicine, New York University College of Medicine, New York City) (Received for publication May 8, 1948) For any exogenous substance which is neither bladder rinses with water and air. The maximum rate metabolized, stored nor excreted otherwise than in of excretion of PAH by the tubules (TmPaH) was also measured in some of the experiments (3). Three or the urine, the rate of excretion must be equal to the more serial urine collection periods of 15 to 30 minutes rate of infusion under conditions where its plasma each were measured. level and volume of distribution are constant. Priming injections of inulin and PAH were given This steady state, as indicated by a constant plasma intravenously in amounts calculated to achieve plasma level, will be designated infusion equilibrium. levels of 5 to 20 and 2 to 3 mg. per cent respectively. The approximate volume of distribution for an average A simplified method for the measurement of normal subject was taken as 15 liters for inulin and 20 glomerular filtration rate and the effective renal liters for PAH. Priming injections of 2 grams of inulin plasma flow based upon the above principle has and 0.8 gram sodium p-aminohippurate were frequently been described elsewhere (1). In the application used and generally resulted in plasma levels of 10 to 15 of the principle, the rate of infusion, IV (where I and 2.5 to 3.0 mg. -

Impaired Tubular Secretion of Organic Solutes in Acute Kidney Injury
Kidney360 Publish Ahead of Print, published on June 24, 2020 as doi:10.34067/KID.0001632020 1 Impaired Tubular Secretion of Organic Solutes in Acute Kidney Injury Frank J. O’Brien1, Robert D. Mair2,3, Natalie S. Plummer2,3, Timothy W. Meyer2,3, *Scott M. Sutherland4, *Tammy L. Sirich2,3 1The Department of Medicine, Washington University, St. Louis, MO 2The Department of Medicine, Stanford University, Palo Alto, CA 3The Department of Medicine, VA Palo Alto Healthcare System, Palo Alto, CA 4The Department of Pediatrics, Lucile Packard Children’s Hospital, Stanford University, Palo Alto, CA *SMS and TLS are Joint Senior Authors Correspondence: Tammy L. Sirich Nephrology 111R Palo Alto VAHCS 3801 Miranda Ave. Palo Alto, CA 94304 [email protected] Copyright 2020 by American Society of Nephrology. 2 Abstract Background. Impairment of kidney function is routinely assessed by measuring the accumulation of creatinine, an organic solute cleared largely by glomerular filtration. We tested whether the clearance of solutes which undergo tubular secretion is reduced in proportion to the clearance of creatinine in humans with acute kidney injury (AKI). Methods. Four endogenously produced organic solutes – phenylacetylglutamine (PAG), hippurate (HIPP), indoxyl sulfate (IS), and p-cresol sulfate (PCS) – were measured in spot urine and plasma samples from 10 AKI patients and 17 control subjects. Fractional clearance relative to creatinine was calculated to assess tubular secretion. Fractional clearance values were calculated in terms of the free, unbound levels of HIPP, IS, and PCS which bind to plasma proteins. Results. Fractional clearance values for PAG, HIPP, IS, and PCS were greater than 1.0 in AKI patients as well as control subjects, indicating that these solutes were still secreted by the tubules of the injured kidneys. -
Effects of Positive Pressure Ventilation on Intrarenal Blood Flow in Infant Primates
Pediat. Res. 8: 792-796 (1974) Antidiuretic hormone intrarenal blood flow developmental physiology kidney intermittent positive pressure ventilation Effects of Positive Pressure Ventilation on Intrarenal Blood Flow in Infant Primates EDDIE S. MOO RE,(^^) MAURINA B. GALVEZ, JOHN B. PATON, DAVID E. FISHER, AND RICHARD E. BEHRMAN Department of Pediatvics, University of Illinois College of Medicine, Chicago, Illinois, USA Extract cortical flow rates in patients with acute failure. Horster and Thurau (9) found that superficial cortical and juxtamedullary Measurement of intrarenal distribution of renal blood flow nephrons in adult rats have different functional capacities. It by injection of radionuclides in 3-5-day-old infant monkeys can be speculated that the occurrence of decreased urine flow showed a preponderance of outer cortical over inner cortical might result from redistribution of blood to inner cortical " flow with flow rates of 4.23 and 2.54 ml/min/g, respectively. nephrons with possible greater reabsorptive capacity. The Intermit tent positive pressure ventilation (IPPV) causes a extent and character of overall renal function may therefore reversal of this flow pattern. The theoretical difference in be in part dependent upon intrarenal distribution as well as on nephron function in these two areas suggests that this reversal total renal blood flow. Although the studies of Jose et al. (1 1) in intrarenal flow induced by IPPV may have important demonstrated a low cortical flow and low total renal blood clinical implications. flow in infant puppies, few studies have been done in infants to measure the effect on intrarenal flow to various stimuli and Speculation how this would affect overall renal function. -
Renal Function in Dogswith Pyometra
Acta vet. scand. 1964, 5, 56-73. From the Department of Surgery and Department of Clinical Biochemistry, Royal Veterinary College, Stockholm, Sweden. RENAL FUNCTION IN DOGS WITH PYOMETRA 3. GLOMERULAR FILTRATION RATE, EFFECTIVE RENAL PLASMA FLOW, AND THE RELATION BETWEEN SOLUTE EXCRETION RATE AND MAXIMUM URINE OSMOLARITY DURING DEHYDRATION By Ake Asheim In bitches with pyometra (chronic purulent endometritis) the ability of the kidneys to excrete concentrated urine is impair ed with polyuria and polydipsia as a result (Asheim 1963 b). Since the limitation in concentrating ability cannot be ascribed to extrarenal causes (insufficiency of the hypothalamic-hypo physeal system, Asbeim 1963 a), it can fairly confidently be assumed to be of renal origin. Renal disease of whatever cause can lead to a reduction in the number of functioning nephrons. The residual functioning nephrons assume a greater excretory burden and because of this a greater osmotic load per nephron. This counterbalances the obligatory water resorption in the proximal tubules and results in so-called osmotic diuresis (Bricker et al. 1960, Kleeman et al. 1960). The osmotic diuresis is combined with a reduction of maximum urine osmolarity (max. Uosm) which is not affected by exogenous antidiuretic hormone (West & Rapoport 1950, Page & Reem 1952, Zak et al. 1954, Dorhout Mees 1959). As the osmotic load increases, max. Uosm gradually decreases until it approaches plasma osmolarity (Posm). Renal damage has been reported in bitches with pyometra (Bloom 1954). One has to take into account the possibility that the functioning renal mass can be reduced to such a degree to 57 give an osmotic diuresis which can explain the reduction of max. -
![L3-Renal Clearance [PDF]](https://docslib.b-cdn.net/cover/4012/l3-renal-clearance-pdf-7994012.webp)
L3-Renal Clearance [PDF]
At the end of this session, the students should be able to: Describe the concept of renal plasma clearance Use the formula for measuring renal clearance Use clearance principles for inulin, creatinine etc. for determination of GFR Explain why it is easier for a physician to use creatinine clearance Instead of Inulin for the estimation of GFR Describe glucose and urea clearance Explain why we use of PAH clearance for measuring renal blood flow Mind map Concept of clearance rate of glomerular filtration Clearance is the volume of plasma that is completely Assess severity of renal cleared of a substance each damage minute. Tubular secretion&reabsorption of renal clearance renal different substances. The important of important The Clearance Equation Clearance tests CX = (UX X V)/ PX endogenous where creatinine Urea Uric acid CX = Renal clearance (ml/min) UX X V = excretion rate of substance X exogenous U = Concentration of X in urine X Inulin Para amino Diodrast (di-iodo V = urine flow rate in ml/min hippuric acid pyridone acetic acid) Px= concentration of substance X in the plasma Measurement of glomerular Measurement of renal Measurement of renal filtration rate (GFR) plasma flow (RPF) blood flow (RBF) GFR is measured by the RPF can be estimated from RBF is calculated from clearance of a glomerular maker the clearance of an organic the RPF and hematocrit like Creatinine & Inulin . acid Para-aminohippuric acid (PAH) The formula used to calculate GFR or RPF is CX = (UX X V)/ PX X could be PAH , creatinine and inulin The formula used to calculate RBF is RBF= RPF \ 1-Hct Or RBF=RPF% \ 100-Hct Hematocrit is the fraction of blood volume that is occupied by red blood cells and 1-Hct or 100-Hct is the fraction of blood volume that is occupied only by plasma Criteria of a substance used Criteria of a substance used for for GFR measurement renal plasma flow measurement 1.freely filtered 1.freely filtered 2.not secreted by the tubular cells 2.rapidly and completely secreted by the renal tubular cells 3.not reabsorbed by the tubular cells. -

Clinical Applications of a Kinetic Model of Hippurate Distribution and Renal Clearance
CLINICAL APPLICATIONS OF A KINETIC MODEL OF HIPPURATE DISTRIBUTION AND RENAL CLEARANCE JosephA. DeGrazia,Paul0. Scheibe,PeterE.Jackson,ZoltanJ. Lucas, William R.Fair,JohnM. Vogel*, and LeonardJ. Blumin Stanford Medical Center, Stanford, California, A nalytical Development Associates Corporation, Cupertino, California, Community Hospital of Los Gatos-Saratoga, Los Gatos, California, USPHS Hospital, San Francisco, California, and Veterans Administration Hospital, San Francisco, California Measurements of effective renal plasma flow yield the basic parameters of renal physiology of and urine flow fractions have been obtained by interest to the clinician. the application of a new kinetic model of o-iodo Recent advances in nuclear medicine instrumenta hippurate distribution and renal clearance. tion and computing have made it possible to further Good agreement was obtained between these develop the radiohippurate method so that it is a estimates and those of comparable parameters quantitative measure of specific kidney functions obtained by conventional split-function tech (10—15). In general, these methods have used a niques using p-aminohippurate and inuliii@ Also, computer to aid in the adjustment of the variable examples have been presented of the use of this parameters of a mathematical description of hip test for the evaluation of patients suffering from purate turnover in the body to extract quantitative well-documented renal diseases. These uses have clinically useful data not usually obtained from the included serial testing in patients with major conventional renogram. renal artery occlusion, bilateral renal vein In this paper we report the first clinical applica thrombosis, obstruction due to stone, or trans tion of a new split-function renal test using an ex plant rejection.