L3-Renal Clearance [PDF]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -

Suppression of Antidiuretic Hormone Secretion by Clonidine in the Anesthetized Dog
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Kidney International, Vol. 7 (1975), p. 405—412. Suppression of antidiuretic hormone secretion by clonidine in the anesthetized dog MICHAEL H. HUMPHREYS and IAN A. REID with the technical assistance of LANCE YA NAN CHOU University of California Renal Center, San Francisco General Hospital, and the Departments of Medicine and Physiology, University of California Medical Center, San Francisco, California Suppression of antidiuretic hormone secretion by clonidine in l'augmentation initiale de Ia pression artérielle par une constric- the anesthetized dog. 5tudies were performed to determine the tion aortique sus-rénale. Au contraire, V, Tc2o et Vosm ne sont mechanism by which the antihypertensive agent clonidine pas modifies par Ia clonidine administrée a sept chiens hypo- increases urine flow (V). In 11 anesthetized, hydropenic dogs, i.v. physectomisés qui recoivent une perfusion constante d'ADH administration of clonidine (30 gJkg) increased arterial pressure (80 1LU/kg/min), malgré des modifications hémodynamiques from 128±4 to 142±3 mm Hg and slowed heart rate from semblables. Les résultats suggCrent que Ia clonidine augmente V 138±7 to 95±7 beats/mm within 30 mm of injection; blood par l'inhibition de Ia liberation d'ADH, peut-être par une voie pressure then fell to 121 5 mm Hg 30 to 60 mm after injection, indirecte empruntant les affets alpha adrCnergiques de Ia and 112 5 mm Hg in the next 30-mm period. V increased from drogue sur Ia circulation. 0.36±0.09 to 0.93±0.13 mI/mm and urine osmolality (Uo,m) decreased from 1378±140 to 488±82 mOsm/kg of H20 30 to 60 mm following injection (P<0.001). -

Studies in Para-Aminohippuric Acid Synthesis in the Human: Its Application As a Liver Function Test
STUDIES IN PARA-AMINOHIPPURIC ACID SYNTHESIS IN THE HUMAN: ITS APPLICATION AS A LIVER FUNCTION TEST William P. Deiss, Philip P. Cohen J Clin Invest. 1950;29(8):1014-1020. https://doi.org/10.1172/JCI102332. Research Article Find the latest version: https://jci.me/102332/pdf STUDIES IN PARA-AMINOHIPPURIC ACID SYNTHESIS IN THE HUMAN: ITS APPLICATION AS A LIVER FUNCTION TEST By WILLIAM P. DEISS AND PHILIP P. COHEN (From the Departments of Medicine and Physiological Chemistry, University of Wisconsin Medical School, Madison, Wisconsin) (Submitted for publication February 24, 1950; accepted, April 17, 1950) Synthesis of p-aminohippuric acid (PAH) from All the subjects received 3 g. of sodium PAB (in the p-aminobenzoic acid (PAB) in animal liver slices commercial tablet form with a starch filler) orally at and homogenates has been shown to resemble least two hours after a light breakfast. On separate occasions 14 subjects, eight of the normal group and closely, both chemically and thermodynamically, six of the liver impairment group, were given 25 ml. the synthesis of peptides (1-3). This reaction of a 20% solution of Glycine, N.F. in addition to the has been utilized in the hippuric acid synthesis oral sodium PAB. One normal subject was given 0.8 g. test for liver function since 1933 (4) and has found of sodium benzoate intravenously ten minutes before the oral dose of sodium PAB. wide clinical application (5-7). Hippuric acid, Five ml. blood samples were withdrawn at regular however, must be determined in the urine and, intervals after administration of sodium PAB and in two consequently, relatively normal renal excretion is normal subjects four hourly total urine specimens were necessary. -
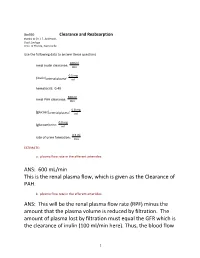
ANS: 600 Ml/Min This Is the Renal Plasma Flow, Which Is Given As the Clearance of PAH
Bio390 Clearance and Reabsorption thanks to Dr. J.F. Anderson, Dept Zoology Univ. of Florida, Gainesville Use the following data to answer these questions. 100 ml renal inulin clearance: min 0.5 mg [inulin]arterial plasma: ml hematocrit: 0.40 600 ml renal PAH clearance: min 0.8 mg [glucose]arterial plasma: ml 0.0 mg [glucose]urine: ml 0.5 ml rate of urine formation: min ESTIMATE: a. plasma flow rate in the afferent arterioles: ANS: 600 mL/min This is the renal plasma flow, which is given as the Clearance of PAH. b. plasma flow rate in the efferent arterioles: ANS: This will be the renal plasma flow rate (RPF) minus the amount that the plasma volume is reduced by filtration. The amount of plasma lost by filtration must equal the GFR which is the clearance of inulin (100 ml/min here). Thus, the blood flow 1 in the efferent arteriole is 600 - 100 ml/min = 500 ml/min in this problem c. plasma flow rate in the renal veins: ANS: by the time that blood enters the veins, nearly all of the water lost during filtration has made its way back to the blood (especially if the subject is dehydrated!). If urine is being formed at a rate of 0.5 mL/min, then that represents (essentially) the volume of water lost per min. So, the renal venous plasma flow rate = RPF- urine loss = 600 - 0.5 = 599.5 ml/min d. renal blood flow rate in renal artery in ml/min ANS: 833 mL/min the hct = 40% (0.4). -

Conjugation Reactions in the Newborn Infant: the Metabolism of Para-Aminobenzoic Acid
Arch Dis Child: first published as 10.1136/adc.40.209.97 on 1 February 1965. Downloaded from Arch. Dis. Childh., 1965, 40, 97. CONJUGATION REACTIONS IN THE NEWBORN INFANT: THE METABOLISM OF PARA-AMINOBENZOIC ACID BY MARKUS F. VEST* and RENI2 SALZBERG From the Children's Hospital, University of Basel, Switzerland (RECEIVED FOR PUBLICATION JULY 8, 1964) It has been shown that the liver of the newborn The method of Deiss and Cohen (1950) was uscd for infant has a limited capacity to perform certain the estimation of PAB and para-aminohippuric acid transformation or conjugation reactions when (PAH). PAH was estimated after extraction of PAB compared to older subjects (Driscoll and Hsia, 1958; with ether. After extracting mixtures of known composi- tion, on the average I % PAB and 98 % PAH remained. Kretchmer, Levine, McNamara, and Barnett, 1956). For the estimation of acetylated PAB and PAH (aceta- This limitation is evident in the formation of mido-benzoic and acetamido-hippuric acid') in the serum glucuronides (Brown and Zuelzer, 1958; Vest, 1958) aliquots ofthe deproteinized supematant were hydrolysed and plays an important role in the genesis of by boiling with 0 * 05 volume of 4 N HC1 for 20 minutes. neonatal jaundice. There are indications that other In the case of urine better results were obtained by conjugation or detoxification mechanisms are also hydrolysing for 45 minutes. In some experiments the carried out in a different way from that of later life. hydrolysis of acetylated compounds was carried out by The observation that after administration of sodium heating at 96° C. -

Renal Effects of Atrial Natriuretic Peptide Infusion in Young and Adult ~Ats'
003 1-3998/88/2403-0333$02.00/0 PEDIATRIC RESEARCH Vol. 24, No. 3, 1988 Copyright O 1988 International Pediatric Research Foundation, Inc. Printed in U.S.A. Renal Effects of Atrial Natriuretic Peptide Infusion in Young and Adult ~ats' ROBERT L. CHEVALIER, R. ARIEL GOMEZ, ROBERT M. CAREY, MICHAEL J. PEACH, AND JOEL M. LINDEN WITH THE TECHNICAL ASSISTANCE OF CATHERINE E. JONES, NANCY V. RAGSDALE, AND BARBARA THORNHILL Departments of Pediatrics [R.L.C., A.R.G., C.E.J., B. T.], Internal Medicine [R.M.C., J.M. L., N. V.R.], Pharmacology [M.J.P.], and Physiology [J.M.L.], University of Virginia, School of Medicine, Charlottesville, Virginia 22908 ABSTRAm. The immature kidney appears to be less GFR, glomerular filtration rate responsive to atrial natriuretic peptide (ANP) than the MAP, mean arterial pressure mature kidney. It has been proposed that this difference UeC~pV,urinary cGMP excretion accounts for the limited ability of the young animal to UN,V, urinary sodium excretion excrete a sodium load. To delineate the effects of age on the renal response to exogenous ANP, Sprague-Dawley rats were anesthetized for study at 31-32 days of age, 35- 41 days of age, and adulthod. Synthetic rat A* was infused intravenously for 20 min at increasing doses rang- By comparison to the adult kidney, the immature kidney ing from 0.1 to 0.8 pg/kg/min, and mean arterial pressure, responds to volume expansion with a more limited diuresis and glomerular filtration rate, plasma ANP concentration, natriuresis (I). A number of factors have been implicated to urine flow rate, and urine sodium excretion were measured explain this phenomenon in the neonatal kidney, including a at each dose. -

Impaired Tubular Secretion of Organic Solutes in Acute Kidney Injury
Original Investigation Impaired Tubular Secretion of Organic Solutes in Acute Kidney Injury Frank J. O’Brien,1 Robert D. Mair,2,3 Natalie S. Plummer,2,3 Timothy W. Meyer,2,3 Scott M. Sutherland,4 and Tammy L. Sirich2,3 Abstract Background Impairment of kidney function is routinely assessed by measuring the accumulation of creatinine, an organic solute cleared largely by glomerular filtration. We tested whether the clearance of solutes that undergo tubular secretion is reduced in proportion to the clearance of creatinine in humans with AKI. Methods Four endogenously produced organic solutes (phenylacetylglutamine [PAG], hippurate [HIPP], indoxyl sulfate [IS], and p-cresol sulfate [PCS]) were measured in spot urine and plasma samples from ten patients with AKI and 17 controls. Fractional clearance relative to creatinine was calculated to assess tubular secretion. Fractional clearance values were calculated in terms of the free, unbound levels of HIPP, IS, and PCS that bind to plasma proteins. Results Fractional clearance values for PAG, HIPP, IS, and PCS were .1.0 in patients with AKI as well as controls, indicating that these solutes were still secreted by the tubules of the injured kidneys. Fractional clearance values were, however, significantly lower in patients with AKI than controls, indicating that kidney injury reduced tubular secretion more than glomerular filtration (AKI versus control: PAG, 2.160.7 versus 4.661.4, P,0.001; HIPP, 1065 versus 1567, P50.02; IS, 1066 versus 2867, P,0.001; PCS, 3.361.8 versus 1063, P,0.001). Free plasma levels rose out of proportion to total plasma levels for each of the bound solutes in AKI, so that calculating their fractional clearance in terms of their total plasma levels failed to reveal their impaired secretion. -

Urate-2- C Transport in the Rat Nephron
Urate-2-14C transport in the rat nephron Ronald A. Kramp, … , William E. Lassiter, Carl W. Gottschalk J Clin Invest. 1971;50(1):35-48. https://doi.org/10.1172/JCI106482. Research Article Intrarenal transport of urate-2-14C was studied in anesthetized rats using the microinjection technic. During saline diuresis, small volumes of urate-2-14C (0.24-0.48 mM) and inulin-3H were injected into surface proximal and distal convoluted tubules, and ureteral urine was collected serially. Total (74-96%) and direct (57-84%) urate recovery increased significantly the more distal the puncture site. Delayed recovery (±20%) remained approximately the same regardless of localization of the microinjection. After proximal injections, total and direct recoveries of urate-2-14C were significantly higher in rats treated with probenecid, pyrazinoate, or PAH than during saline diuresis alone, while the excretion rates were comparable after distal injection. Delayed recovery was not altered by drug administration. The decreased proximal reabsorption of urate is presumably due to an effect of the drugs on the luminal membrane of the nephron. For perfusion at high urate concentrations, nonradioactive urate was added to the injectate (0.89-1.78 mM). Urate-2-14C recovery was almost complete and there was no delayed excretion, demonstrating saturation kinetics. These findings are compatible with a carrier-mediated mechanism for urate transport probably located at the luminal border of the proximal tubular epithelium. No definitive evidence for urate secretion was found in these studies. Find the latest version: https://jci.me/106482/pdf Urate-2-14C Transport in the Rat Nephron RONALD A. -

Production of Hypertonic Urine in the Absence of Pituitary Antidiuretic Hormone
Production of Hypertonic Urine in the Absence of Pituitary Antidiuretic Hormone Robert W. Berliner, Douglas G. Davidson J Clin Invest. 1957;36(10):1416-1427. https://doi.org/10.1172/JCI103541. Research Article Find the latest version: https://jci.me/103541/pdf PRODUCTION OF HYPERTONIC URINE IN THE ABSENCE OF PITUITARY ANTIDIURETIC HORMONE 1 BY ROBERT W. BERLINER AND DOUGLAS G. DAVIDSON 2 (From the Laboratory of Kidney and Electrolyte Metabolism, National Heart Institute, National Institutes of Health, Public Health Sertice, Department of Health, Education, and Welfare, Bethesda, Md.) (Submitted for publication May 1, 1957; accepted May 23, 1957) The mechanism by which pituitary antidiuretic permeability of the tubule membrane to water. hormone (ADH) produces its renal effect has The change to hypertonicity cannot be so readily not been clearly established. Under ordinary con- attributed to an effect on water permeability with- ditions, in the absence of ADH, urine of a con- out some assumptions as to the mechanism by centration considerably below that of plasma is which the hypertonicity is produced. However, produced in large volume. With increasing it is a reasonable hypothesis that the mechanism amounts of ADH, administered or secreted, the for the production of hypertonicity is not depen- osmotic pressure of the urine rises to and above dent upon ADH but that its effects are unmasked, that of plasma. With respect to total water bal- in the presence of ADH, by 1) changes in the vol- ance, the quantitatively more important contri- ume and concentration of urine delivered to it and, bution to water economy is the change between possibly, 2) changes in the permeability of the maximally dilute and isotonic urine, since this, in membranes separating the concentrating mecha- normal man, may involve a change in water ex- nism from the urine in the tubule lumen. -

A Compendium of Research
NASA TECHNICAL NASA TM X-3308 MEMORANDUM CO CO I X c PHYSIOLOGIC RESPONSES TO WATER IMMERSION IN MAN: A COMPENDIUM OF RESEARCH James Kollias, Dena Van Derveer, Karen J. Dorchak, and John E. Greenleaf Ames Research Center Moffett Field, Calif. 94035 ^ *" /V NATIONAL AERONAUTICS AND SPACE ADMINISTRATION • WASHINGTON, D. C. • FEBRUARY 1976 1. Report No. 2. Government Accession No. 3. Recipient's Catalog No. NASA TM X-3308 4. Title and Subtitle 5. Report Date February 1976 PHYSIOLOGIC RESPONSES TO WATER IMMERSION IN MAN: 6. Performing Organization Code A COMPENDIUM OF RESEARCH 7. Author(s) 8. Performing Organization Report No. A-6038 James Kollias, Dena Van Derveer, Karen J. Dorchak, and John E. Greenleaf 10. Work Unit No. 9. Performing Organization Name and Address 970-21-14-05 NASA Ames Research Center 11. Contract or Grant No. Moffett Field, Calif. 94035 13. Type of Report and Period Covered 12. Sponsoring Agency Name and Address Technical Memorandum National Aeronautics and Space Administration 14. Sponsoring Agency Code Washington, D. C. 20546 15. Supplementary Notes 16. Abstract Since the advent of space flight programs, scientists have been searching for ways to reproduce the zero-gravity effects of weightlessness. Brief periods of weightlessness up to 1 minute were feasible using Keplerian trajectory, but comprehen- sive study of the prolonged effects of the weightless state necessitated the development of other methods. Thus far the two approaches most widely used have been complete bedrest and fluid immersion. Surprisingly, these simulated environments have produced essentially all of the symptoms found in astronauts. This compendium contains reports appearing in the literature through December 1973. -

The Effects of Losartan on Renal Function in the Newborn Rabbit
0031-3998/02/5106-0728 PEDIATRIC RESEARCH Vol. 51, No. 6, 2002 Copyright © 2002 International Pediatric Research Foundation, Inc. Printed in U.S.A. The Effects of Losartan on Renal Function in the Newborn Rabbit ANNE PRÉVOT, DOLORES MOSIG, AND JEAN-PIERRE GUIGNARD Division of Pediatric Nephrology, Department of Pediatrics, Lausanne University Medical Center, CH 1011 Lausanne, Switzerland ABSTRACT The low GFR of newborns is maintained by various factors dose can be considered as reflex vasoconstriction of afferent and including the renin-angiotensin system. We previously estab- efferent arterioles, rather than specific receptor antagonism. We lished the importance of angiotensin II in the newborn kidney, conclude that under physiologic conditions, the renin- using the angiotensin-converting enzyme inhibitor perindoprilat. angiotensin is critically involved in the maintenance of GFR in The present study was designed to complement these observa- the immature kidney. (Pediatr Res 51: 728–732, 2002) tions by evaluating the role of angiotensin-type 1 (AT1) recep- tors, using losartan, a specific AT1-receptor blocker. Increasing doses of losartan were infused into anesthetized, ventilated, Abbreviations newborn rabbits. Renal function and hemodynamic variables AII, angiotensin II were assessed using inulin and para-aminohippuric acid clear- ACE, angiotensin-converting enzyme ances as markers of GFR and renal plasma flow, respectively. ARI, acute renal insufficiency Losartan 0.1 mg/kg slightly decreased mean blood pressure AT1, angiotensin type 1 receptor Ϫ ϩ ( 11%) and increased diuresis ( 22%). These changes can be AT2, angiotensin type 2 receptor explained by inhibition of the AT1-mediated vasoconstrictive BK, bradykinin and antidiuretic effects of angiotensin, and activation of vasodi- BW, body weight lating and diuretic AT2 receptors widely expressed in the neo- EFP, effective filtration pressure natal period. -

Emerging Kidney Models to Investigate Metabolism, Transport and Toxicity of Drugs and Xenobiotics
DMD Fast Forward. Published on August 3, 2018 as DOI: 10.1124/dmd.118.082958 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 82958 1. Title page Emerging Kidney Models to Investigate Metabolism, Transport and Toxicity of Drugs and Xenobiotics Piyush Bajaj, Swapan K. Chowdhury, Robert Yucha, Edward J. Kelly, Guangqing Xiao Drug Safety Research and Evaluation, Takeda Pharmaceutical International Co., Cambridge, Massachusetts (P.B.); Drug Metabolism and Pharmacokinetics Department, Takeda Pharmaceutical International Co., Cambridge, Massachusetts (S.K.C., R.Y., G. X.); Department of Pharmaceutics, University of Washington, Seattle, Washington (E.J.K.) Downloaded from dmd.aspetjournals.org at ASPET Journals on September 26, 2021 1 DMD Fast Forward. Published on August 3, 2018 as DOI: 10.1124/dmd.118.082958 This article has not been copyedited and formatted. The final version may differ from this version. DMD # 82958 2. Running title page Running title: Emerging kidney models for investigating transport and toxicity Corresponding Author: Piyush Bajaj, PhD Global Investigative Toxicology Downloaded from Drug Safety Research and Evaluation 35 Landsdowne Street, Cambridge, MA 02139 USA Phone: 617-679-7287 Email: [email protected] dmd.aspetjournals.org Document Statistics: at ASPET Journals on September 26, 2021 Number of text pages: 27 Number of tables: 2 Number of figures: 2 Number of references: 114 Number of words in Abstract: 227 Number of words in Introduction: 665 Nonstandard abbreviations used in the paper: 3,4,5-trichloroaniline (TCA) American Type Culture Collection (ATCC) Aminopeptidase N (CD13) Aquaporin 1 (AQP-1) Area under the receiver operating characteristic curve (AUC-ROC) Aristolochic acid (AA) ATP-binding cassette (ABC) Breast cancer resistance protein (BCRP) Chinese Hamster Ovary (CHO) Conditionally immortalized proximal tubule epithelial cells (ciPTEC) Conditionally immortalized proximal tubule epithelial cells overexpressing OAT-1 (ciPTEC - OAT1) 2 DMD Fast Forward.