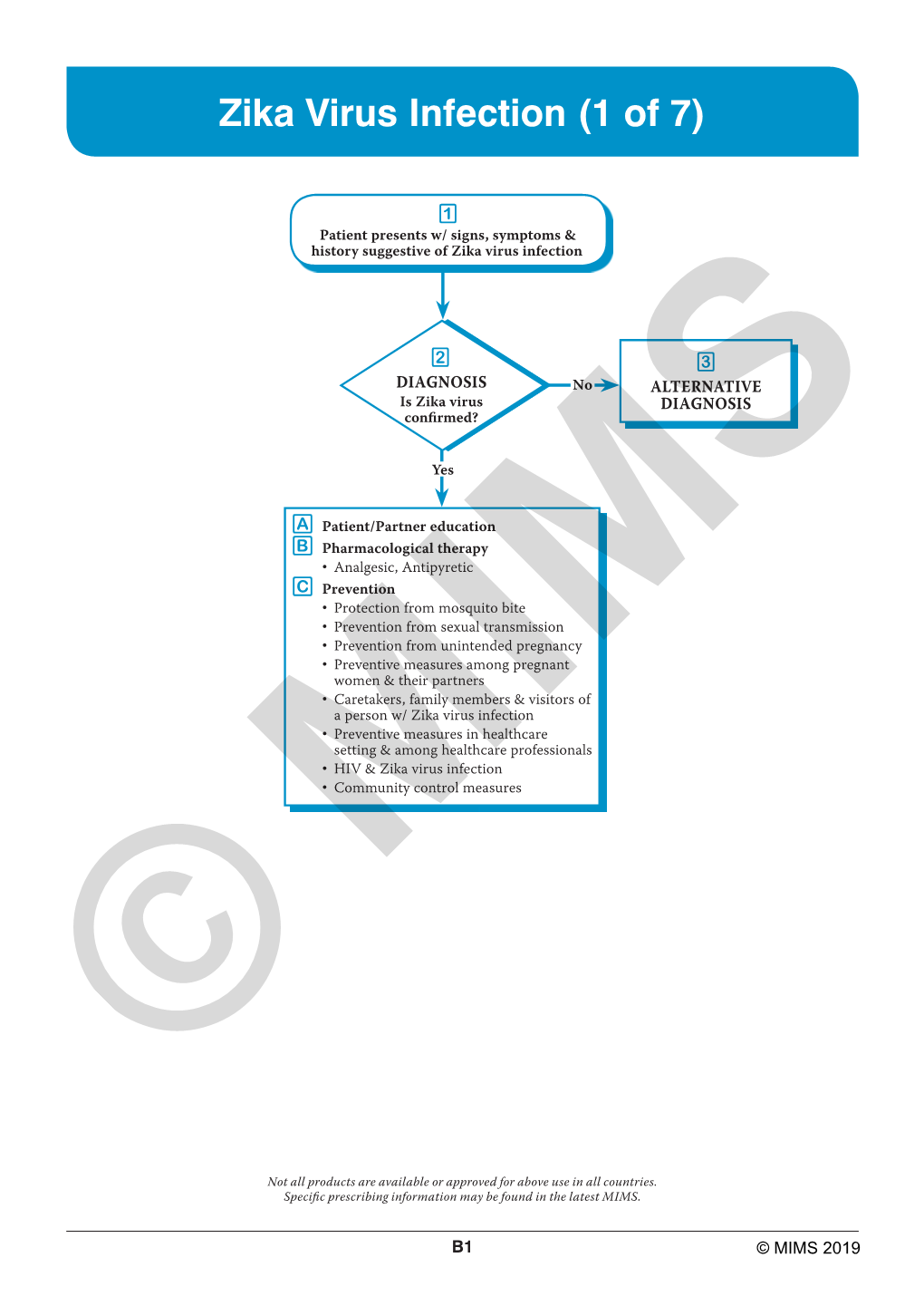
Zika Virus Infection (1 of 7)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Culicidés Et Arbovirus De Centrafrique
THÈSE présentée à l'UNIVERSITE DE PARIS SUD CENTRE D'ORSAY pour obtenir le titre de DOCTEUR D'UNIVERSITE par Bernard GEOFFROY CULICID~S ET ARBOVIRUS DE CENTRAFRIQUE Soutenue le 6 janvier 1982 devant la Commission d'Examen: Messieurs J. BERGERARD Président J. MOUCHET Y. GILLON Examinateurs M. GERMAIN J. COZ O.R.S.T.O.M. - PARIS - 1982 THE SE présentée A L'UNIVERSITE DE PARIS SUD CENTRE D'ORSAY pour obtenir Le titre de DOCTEUR D'UNIVERSITE par BERNARD GEOFFROY CULICIDES ET ARBOVIRUS DE CENTRAFRIQUE Soutenue le: 6 j anvier 1982 devant la Commission d' examen ~lessieurs BERGERARD J. Président MOUCHET J. GILLON • Y. Examinateurs GEFJvIAIN 1\1. • •••••••••••• COZ J. O.R.S.T.O.M. - PARIS - 1982 CUL ICI DES ET ARB0 Vl RUS DE CENTRAFRl QUE ETUDE BIOÉCOLOGIQUE DES MOUSTIQUES ADULTES DES STATIONS DE LA GOMOKA ET DE BOZO, ET DE LEUR ROLE DANS L'EPIDEMIOLOGIE DES ARBOVIRUS l 1 J ~ j l 1 1j SOM MAI RE page REMERCIEMENTS 1 INTRODUCTION 3 CHAP ITRE 1 . 5 1. GENERALITES SUR LA R.C.A. 7 1 • 1. Cl imatoI0 gi e 7 1. 2. Situation géographique .•...•....••••....• 8 1.3. Hydrographie............................. 8 1.4. Données démographiques .•••.••••••.......• 9 2. PRESENTATION DES ZONES D'ETUDE ..••..•••..•..•• 10 2.1. Climatologie 10 2.2. Phytogéographie 11 i 3. DONNEES RELATIVES AUX PRINCIPAUX POINTS 1 D'OBSERVATIONS ......•..................••..... 15 J 1 3.1. Station de LA GOMOKA .••........•.•.•.•... -15 1 3.2. Station de BOZO . 18 1 CHAPITRE 23 1 II l l'Éçtlli!Qllɧ _ÉI )=1ÉItiQgɧ ..•.....•••.....•.•..... 25 1 1. METHODES DE CAPTURES •.......•.........•.....•. 26 1 1 1 .1. -

Sampling Adults by Animal Bait Catches and by Animal-Baited Traps
Chapter 5 Sampling Adults by Animal Bait Catches and by Animal-Baited Traps The most fundamental method for catching female mosquitoes is to use a suit able bait to attract hungry host-seeking individuals, and human bait catches, sometimes euphemistically called landing counts, have been used for many years to collect anthropophagic species. Variations on the simple direct bait catch have included enclosing human or bait animals in nets, cages or traps which, in theory at least, permit the entrance of mosquitoes but prevent their escape. Other attractants, the most widely used of which are light and carbon dioxide, have also been developed for catching mosquitoes. In some areas, especially in North America, light-traps, with or without carbon dioxide as a supplement, have more or less replaced human and animal baits as a routine sampling method for several species (Chapter 6). However, despite intensive studies on host-seeking behaviour no really effective attractant has been found to replace a natural host, and consequently human bait catches remain the most useful single method of collecting anthropophagic mosquitoes. Moreover, although bait catches are not completely free from sampling bias they are usually more so than most other collecting methods that employ an attractant. They are also easily performed and require no complicated or expensive equipment. HUMAN BAIT CATCHES Attraction to hosts Compounds used by mosquitoes to locate their hosts are known as kairomones, that is substances from the emitters (hosts) are favourable to the receiver (mosquitoes) but not to themselves. Emanations from hosts include heat, water vapour, carbon dioxide and various host odours. -

Zika Virus Infection
SAS Journal of Medicine ISSN 2454-5112 SAS J. Med., Volume-3; Issue-7 (Jul, 2017); p-186-193 Available online at http://sassociety.com/sasjm/ Review Article Zika Virus Infection: No Longer a Public Health Emergency of International Concern, an Update and Future Trend Mubano Olivier Clément* School of Pharmaceutical Science, Jiangnan University, Jiangsu Province, P.R. China *Corresponding author Mubano Olivier clément Email: [email protected] Abstract: Zika virus (ZIKV), a flavivirus known since 1947 and spread by Aedes mosquitoes is an arbovirus responsible of ZIKV infections with normally mild clinical symptoms. It’s only since its outbreak in Brazil from when it is considered as serious problem with public health emergency and international concern; thus it appears to be associated with congenital microcephaly accompanied by grave outcomes. Fortunately, at the end of 2016 the ZIKV epidemic starts to decline, resulting in the end of World Health Organization’s zika virus consideration as a problem of public health emergency. Here, we reviewed the transmission, clinical essentials and prevention of ZIKV infection by highlighting the reason behind of zika decreasing, but also the future perspective regarding vaccine and therapy against this virus. Keywords: zika virus, aedes aegypti, World Health Organization, microcephaly, prevention. INTRODUCTION cells near the site of inoculation then spread to lymph Recently since 2015 there has been a prompt nodes and the bloodstream [5]. Although flaviviral and a quick emergence of ZIKV in different part of the replication is thought to occur in cellular cytoplasm, World especially in Americas. This outbreak has one study suggested that ZIKV antigens could be found pushed the World Health Organization (WHO) to in infected cell nuclei [6]. -

The Epidemiology of Zika Virus in the World: a Comprehensive Review Study Jamal Ahmadzadeh1*, Ghazal Akhavan Masoumi1, Mohammad Heidari2 and Kazhal Mobaraki1*
CLINICAL AND EXPERIMENTAL INVESTIGATIONS | ISSN 2674-5054 Available online at www.sciencerepository.org Science Repository Review Article The Epidemiology of Zika Virus in the World: A Comprehensive Review Study Jamal Ahmadzadeh1*, Ghazal Akhavan Masoumi1, Mohammad Heidari2 and Kazhal Mobaraki1* 1Social Determinants of Health Research Center, Urmia University of Medical Sciences, Urmia, Iran 2Department of Biostatistics and Epidemiology, School of Medicine Urmia University of Medical Sciences, Urmia, Iran A R T I C L E I N F O A B S T R A C T Article history: Zika virus is an emerging public health threat. The large outbreak related to this infection was first reported Received: 29 June, 2020 in 2007 in Yap Island. This virus is associated with microcephaly, Guillain Barre syndrome and some of the Accepted: 1 August, 2020 presentations of Zika infection include fever, maculopapular rash, arthralgia, bilateral conjunctivas, Published: 21 August, 2020 headache, arthritis/arthralgia with edema of tiny joints of feet and hands, retro-orbital pain, myalgia, asthenia Keywords: and vertigo. In most of the cases, the infection is asymptomatic and self-limited. One of the largest known Zika virus outbreaks of the virus was reported in French Polynesia, south pacific in October 2013. At the beginning of emerging infection 2016, more than 52 countries have had reported the active transmission of the Zika virus. In general, there infectious diseases are two transmission modes for the Zika infection: Vector-borne transmission and Non-vector-borne worldwide transmission. Some diagnostic tests for Zika infection are RT-PCR, ELISA, and PRNT. Up to now, there is no specific antiviral medicine for the treatment of Zika infection and also no vaccine is available for immunization. -

Zika Virus: an Updated Review of Competent Or Naturally Infected Mosquitoes Yanouk Epelboin, Stanislas Talaga, Loïc Epelboin, Isabelle Dusfour
Zika virus: An updated review of competent or naturally infected mosquitoes Yanouk Epelboin, Stanislas Talaga, Loïc Epelboin, Isabelle Dusfour To cite this version: Yanouk Epelboin, Stanislas Talaga, Loïc Epelboin, Isabelle Dusfour. Zika virus: An updated review of competent or naturally infected mosquitoes. PLoS Neglected Tropical Diseases, Public Library of Science, 2017, 11 (11), pp.e0005933. 10.1371/journal.pntd.0005933. hal-01844517 HAL Id: hal-01844517 https://hal.archives-ouvertes.fr/hal-01844517 Submitted on 19 Jul 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. REVIEW Zika virus: An updated review of competent or naturally infected mosquitoes Yanouk Epelboin1*, Stanislas Talaga1, Loïc Epelboin2,3, Isabelle Dusfour1 1 VectopoÃle Amazonien Emile Abonnenc, Vector Control and Adaptation Unit, Institut Pasteur de la Guyane, Cayenne, French Guiana, France, 2 Infectious and Tropical Diseases Unit, Centre Hospitalier AndreÂe Rosemon, Cayenne, French Guiana, France, 3 Ecosystèmes amazoniens et pathologie tropicale (EPAT), EA 3593, Universite -

Zika Virus Update
ZIKA Virus Factsheet for Health Professionals Zika virus (ZIKV) is a member of the Flaviviridae virus family and the flavivirus genus. In humans, it causes a disease known as Zika fever. It is related to dengue, yellow fever, West Nile and Japanese encephalitis, viruses that are also members of the virus family Flaviviridae. Outbreaks of Zika virus have previously been reported in tropical Africa, in some areas in Southeast Asia and more recently in the Pacific Islands and currently in Americas, especially Brazil. Zika virus infection is symptomatic in only about one out of every five cases. When symptomatic, Zika infection usually presents as an influenza-like syndrome, often mistaken for other arboviral infections like dengue or chikungunya. It is believed that Zika cuases brain damage and microcephaly in babies born with the virus after their mothers have been infected during the pregnancy. Zika virus infection is notifiable in New Zealand as an arboviral disease. It is transmitted by mosquitoes and has been isolated from a number of species in the genus Aedes - Aedes aegypti, Aedes africanus, Aedes apicoargenteus, Aedes furcifer, Aedes luteocephalus and Aedes vitattus. The mosquitoes that are able to spread zika virus are not normally found in New Zealand. AGENT Zika virus is a mosquito-borne flavivirus closely related to dengue virus. The virus was first isolated in 1947 from a sentinel rhesus monkey stationed on a tree platform in the Zika forest, Uganda. RESERVOIR The virus reservoirs are presumably monkeys. TRANSMISSION MODES Zika virus is transmitted to humans mainly by certain species of Aedes mosquitoes. Some of these species bite during the day as well as in the late afternoon/evening. -

1 Analytical Methods for Detection of Zika Virus Kai-Hung Yang1, Roger J
Analytical methods for detection of Zika virus Kai-Hung Yang1, Roger J. Narayan1,2* Department of Material Science Engineering, North Carolina State University, Box 7907, Raleigh, NC, 27695, USA Joint Department of Biomedical Engineering, University of North Carolina and North Carolina State University, Box 7115, Raleigh NC 27695, USA Corresponding author* Corresponding author: Roger J. Narayan UNC/NCSU Joint Department of Biomedical Engineering Raleigh, NC 27695-7115 USA T: 1 919 696 8488 E: [email protected] 1 Abstract Due to the recent outbreak of the Zika virus in several regions, rapid and accurate methods to diagnose Zika infection are in demand, particularly in regions that are on the frontline of a Zika virus outbreak. In this paper, three diagnostic methods for Zika virus are considered. Viral isolation is the gold standard for detection; this approach can involve incubation of cell cultures. Serological identification is based on the interactions between viral antigens and immunoglobulin G (IgG) or immunoglobulin M (IgM) antibodies; cross reactivity with other types of flaviviruses can cause reduced specificity with this approach. Molecular confirmation, such as reverse transcription polymerase chain reaction (RTPCR), involves reverse transcription of RNA and amplification of DNA. Quantitative analysis based on real time RTPCR can be undertaken by comparing fluorescence measurements against previously developed standards. A recently developed programmable paper-based detection approach can provide low-cost and rapid analysis. These viral identification and viral genetic analysis approaches play crucial roles in understanding the transmission of Zika virus. ` 2 Introduction Zika virus (ZIKV) is an arthropod-borne virus in the genus Flavivirus and the family Flaviviridae. -
Microbial Zoonoses and Sapronoses
Microbial Zoonoses and Sapronoses Zdenek Hubálek · Ivo Rudolf Microbial Zoonoses and Sapronoses 123 Dr. Zdenek Hubálek Dr. Ivo Rudolf Academy of Sciences of the Czech Academy of Sciences of the Czech Republic Republic Institute of Vertebrate Biology, v.v.i. Institute of Vertebrate Biology, v.v.i. 60365 Brno 60365 Brno Czech Republic Czech Republic [email protected] and Masaryk University Faculty of Science Institute of Experimental Biology 61137 Brno Czech Republic [email protected] ISBN 978-90-481-9656-2 e-ISBN 978-90-481-9657-9 DOI 10.1007/978-90-481-9657-9 Springer Dordrecht Heidelberg London New York © Springer Science+Business Media B.V. 2011 No part of this work may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, microfilming, recording or otherwise, without written permission from the Publisher, with the exception of any material supplied specifically for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. The authors of photographs on the cover are: Pavel Rodl (4), Zdenek Hubalek (4), Jan Erhart (2), Paul Reiter (1) and Milan Pejcoch (1). Printed on acid-free paper Springer is part of Springer Science+Business Media (www.springer.com) Acknowledgements We are grateful to Dr Silvie Šikutová for preparing several figures, and to many photographers (quoted under the figures) for supplying their photos for this book. Preparation of this book was partially funded by EU grant GOCE-2003-010284 EDEN. The paper is catalogued by the EDEN Steering Committee as EDEN 0191 (http://www.eden-fp6project.net/). -

La Transmission Du Virus Amaril En Afrique Occidentale
Cah. O.R.S.T.O.M., st:r. Enf. méd. Parasifol., vol. IS, nu 1, 1971. La transmission du virus arnaril en Afrique occidentale. Ecologie, répartition, fréquence et contrôle des vecteurs, et observations concernant l’épidémiologie de la fièvre jaune. J. HAMON *) G. PI;CHON * * M. CORNET * * + Les auteurs rr’sument rapidement les modalités de tr,ansmission de la fièvre jaune en s’attachant particulièrement aux éfudes et observations faifes en Afrique occi- dentale ef, dans une moindre mesure, en Afrique orientale et centrale. Ils étudient ensuite les enseignements que I’on peut tirer des récentes épidémies de fièvre jaune qui ont fr,appé l’Afrique occidentale en 1969. Ils soulignent qu’en dépif des recherches faites depuis une Quarant#aine d’années, la persistance clu virus amaril en Afrique occidentale au cours des périodes in ferkpidémiques reste inexpliquke et que les cycles dc transmission qui sont à l’origine des épidPmies périodiques sont essentiellement hypothc~fiqucs. Ils notenf qu’au cours cles épidémies de fièvre jaune observées en Afrique depuis trente ans le rôle des vecfeurs selvafiques semble avoir été souvent plus important que celui joué par Acdes aegypti. Les auteurs présenfenf, sous une forme condensée, les observations faites SUI l’écologie, lu répartifion ef la fréquence des priticipaux vecteurs potenfiels de fièvre jaune existant en Afrique occidentale. Un courf chapitre traite ensuite de la prlvention de la multiplication des vecteurs et de leur confrôle en période épidémique. Dans leurs conclusions, les auteurs soulignent la nécessité d’intensifier les recher- ches sur l’épidémiologie de la fièvre jaune en Afrique occidentale. -
Zika Virus: an Updated Review of Competent Or Naturally Infected Mosquitoes
REVIEW Zika virus: An updated review of competent or naturally infected mosquitoes Yanouk Epelboin1*, Stanislas Talaga1, Loïc Epelboin2,3, Isabelle Dusfour1 1 VectopoÃle Amazonien Emile Abonnenc, Vector Control and Adaptation Unit, Institut Pasteur de la Guyane, Cayenne, French Guiana, France, 2 Infectious and Tropical Diseases Unit, Centre Hospitalier AndreÂe Rosemon, Cayenne, French Guiana, France, 3 Ecosystèmes amazoniens et pathologie tropicale (EPAT), EA 3593, Universite de Guyane±Cayenne, French Guiana * [email protected] Abstract Zika virus (ZIKV) is an arthropod-borne virus (arbovirus) that recently caused outbreaks in the Americas. Over the past 60 years, this virus has been observed circulating among Afri- a1111111111 can, Asian, and Pacific Island populations, but little attention has been paid by the scientific a1111111111 community until the discovery that large-scale urban ZIKV outbreaks were associated with a1111111111 a1111111111 neurological complications such as microcephaly and several other neurological malforma- a1111111111 tions in fetuses and newborns. This paper is a systematic review intended to list all mosquito species studied for ZIKV infection or for their vector competence. We discuss whether stud- ies on ZIKV vectors have brought enough evidence to formally exclude other mosquitoes than Aedes species (and particularly Aedes aegypti) to be ZIKV vectors. From 1952 to OPEN ACCESS August 15, 2017, ZIKV has been studied in 53 mosquito species, including 6 Anopheles, 26 Aedes, 11 Culex, 2 Lutzia, 3 Coquillettidia, 2 Mansonia, 2 Eretmapodites, and 1 Uranotae- Citation: Epelboin Y, Talaga S, Epelboin L, Dusfour I (2017) Zika virus: An updated review of nia. Among those, ZIKV was isolated from 16 different Aedes species. -
Breeding Substrates and Diversity of Aedes Species in Periurban Areas
International Journal of Mosquito Research 2019; 7(4): 39-44 ISSN: 2348-5906 CODEN: IJMRK2 IJMR 2019; 7(4): 39-44 Breeding substrates and diversity of aedes species © 2019 IJMR www.dipterajournal.com in Periurban areas of Côte d’Ivoire Received: 18-05-2020 Accepted: 20-06-2020 Jean Michel Vianney Beugré, Geneviève Lydie Yao-Acapovi, Diakaridia Jean Michel Vianney Beugré Laboratoire de Biologie et Santé, Fofana, Koné Atioumounan Blaise, Konan Kouassi Lambert and UFR Biosciences, Université Sevidzem Silas Lendzele Félix Houphouët Boigny, Abidjan, Côte d’Ivoire Abstract Geneviève Lydie Yao-Acapovi As part of the arboviral disease vectors surveillance in Côte d'Ivoire, a longitudinal entomological Laboratoire de Biologie et Santé, prospection was undertaken in five stations. Mosquito larvae collections were carried out monthly from UFR Biosciences, Université March 2018 to September 2019 in breeding sites and using the WHO-type oviposition trap. These larvae Félix Houphouët Boigny, were reared till adult stage at the insectarium of the Institut National d’Hygiène Publique (INHP) in Abidjan, Côte d’Ivoire Abidjan. Adult mosquitoes were morphologically identified using standard keys. In total, 896 potential mosquito larval breeding substrates were identified. Aedes larvae were collected from 225 sites. The Diakaridia Fofana ideal breeding substrates for Aedes consisted of abandoned containers/objects (39.6%), natural breeding Institut National d’Hygiène sites (31.6%), and storage containers (22.2%). It was noticed that used tires (5.3%) and other breeding Publique (INHP) Abidjan, substrates (1.3%) were poorly represented. There was a statistically significant difference (χ2 = 48.748; Ministère de la Santé et de ddl = 16; P = 0.000) in the positive proportions of Aedes with breeding substrates. -

A Review on the Incidence, Interaction, and Future Perspective on Zika Virus
Review Article A Review on the Incidence, Interaction, and Future Perspective on Zika Virus Lukman Olalekan Afolabi, Musbahu Muhammad Sani, Wahab Oluwanisola Okunowo1 Department of Biochemistry, College of Medicine and Health Sciences, Federal University Dutse, PMB 7156, Jigawa State, 1Department of Biochemistry, College of Medicine, University of Lagos, PMB 12003, Lagos State, Nigeria ABSTRACT Zika virus (ZIKV) belongs to the family Flaviviridae and genus Flavivirus. It is a single-stranded positive-sense ribonucleic acid (RNA) virus, has its origin traced to Zika forest in Uganda. Its infection leads to ZIKV fever, characterized by arthralgia, myalgia, rash, conjunctivitis, and asthenia. Clinical presentation of the infection is nonspecific and may often be confused with symptoms of other flaviviral diseases (dengue, West Nile [WN], and chikungunya). Recently, ZIKV has been associated with congenital malformations and neurological complications such as microcephaly and Guillain–Barre’ syndrome. The viral tropism revealed an infection of the skin fibroblasts, keratinocytes, and immature dendritic cells through enhanced expression of dendritic cell‑specific intracellular adhesion molecule 3-grabbing nonintegrin or anexelecto (Greekword: 'uncontrolled’) and tyrosine protein kinase receptor 3 systems. Silencing of T-cell immunoglobulin (Ig) and mucin domain 1 (TIM-1) and AXL RNAs has shown blockage of viral entry through their anti-TIM-1 and anti-AXL antibodies, hence serving as a potential target for ZIKV drug development. Biotechnological approaches targeted toward ZIKV vector control include the development of transgenic mosquitoes to disrupt the genome pool of wild strains and use of an endosymbiotic bacterium to prevent replication of arboviruses within its vector. Other approaches include the use of gene drive and exploration of the genetic redundancy to disrupt the receptors used by the virus to gain entry into its host.