National Medical Examiner's Good Practice Guidelines
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Medicolegal Death Investigation Forensic Pathology: Forensic
Medicolegal Death Investigation Forensic Pathology: Forensic pathology is a specific practice of medicine and subspecialty of pathology that directs its efforts to the examination of dead persons (and sometimes live persons) to provide an opinion concerning the: • cause, mechanism, and manner of disease, injury, or death; • identification of persons; • significance of biological and physical evidence; • correlation and/or reconstruction of wounds, wound patterns, and sequences. Forensic pathology is an integral component of comprehensive medicolegal death investigation. Forensic pathology applies techniques of pathology to the needs and protection of public health, Homeland Security (surveillance and mass disaster operations), public safety, quality assurance, education in medicine, research, jurisprudence, and the administration of justice. The highest goal of forensic pathology is the development of strategies to prevent injury, disease, and death. Forensic Pathologists: Forensic pathologists should be physicians specially trained in forensic pathology and board-certified by the American Board of Pathology or a non- USA trained pathologist with equivalent certification. The practicing forensic pathologist is licensed as a physician in one or more states and is skilled in conducting death investigations, interpreting injuries in both fatal and non-fatal cases, performing medicolegal examinations, determining disease/injury causation to an appropriate degree of medical certainty, and determining cause and manner of death. Forensic pathologists -

Views of the Commission Recognizing the Autonomy and Neutrality of Forensic Pathologists
NATIONAL COMMISSION ON FORENSIC SCIENCE Views of the Commission Recognizing the Autonomy and Neutrality of Forensic Pathologists Subcommittee Date of Current Version 13/12/16 Medicolegal Death Investigation Approved by Subcommittee 15/12/16 Status Approved by Commission 09/01/17 Adopted by the Commission Commission Action On January 9, 2017, the Commission voted to adopt this Views Document by a more than two- thirds majority affirmative vote (94% yes, 0% no, 6% abstain). Note: This document reflects the views of the National Commission on Forensic Science, and does not necessarily represent the views of the Department of Justice or the National Institute of Standards and Technology. The portion of the document directly labeled “Views of The Commission” represents the formal Views of the Commission. Information beyond that section is provided for context. Views documents do not request specific action by the Attorney General, and thus do not require further action by the Department of Justice upon their approval by the Commission. The National Commission on Forensic Science is a Federal Advisory Committee established by the Department of Justice. For more information, please visit: https://www.justice.gov/ncfs. Overview Currently, many medicolegal offices do not allow (or they restrict) forensic pathologists (FPs) from performing private work outside of their full-time employment, to include consultative work and/or locum tenens for reasons of alleged conflicts of commitment and/or interest. Because of the national shortage of forensic -

Forensic Sciences Medical Examiner - 20859
State of Alabama Personnel Department 64 North Union Street P. O. Box 304100 Montgomery, AL 36130-4100 Phone: (334) 242-3389 Fax: (334) 242-1110 www.personnel.alabama.gov Continuous Announcement FORENSIC SCIENCES MEDICAL EXAMINER - 20859 Salary: $116,277.60 – 177,266.40 Announcement Date: February 5, 2009 **Effective Thursday, February 5, 2009, this recruitment is being reannounced** JOB INFORMATION The Forensic Sciences Medical Examiner is a permanent full-time position with the Department of Forensic Sciences. Positions are located throughout the state. This is complex professional work in the field of death investigations and forensic pathology. Employees in this class perform complex professional work as physicians, skilled not only in medical and laboratory procedures, but also experienced and knowledgeable in the medicolegal investigation of death. MINIMUM REQUIREMENTS • Graduation from an accredited medical school or osteopathic school • Successful completion of a residency program in anatomic pathology or combined anatomic and clinical pathology program accredited by the American Council for Graduate Medical Education (ACGME) • Preferred board certification in anatomic pathology by the American Board of Pathology • Successful completion of a forensic fellowship program accredited by ACGME. ADDITIONAL REQUIREMENT • Applicants must obtain a valid license to practice medicine or osteopathy in the State of Alabama. Please list all certification and licensing (e.g., license #) information on your application. BENEFITS • Low-Cost Health/Dental -
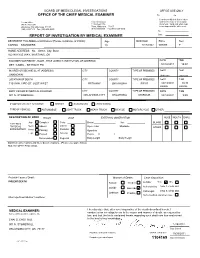
Saundersautopsy.Pdf
BOARD OF MEDICOLEGAL INVESTIGATIONS OFFICE USE ONLY OFFICE OF THE CHIEF MEDICAL EXAMINER Re Co I hereby certify that this is a true Central Office Eastern Division and correct copy of the original 901 N. Stonewall 1115 West 17th document. Valid only when copy Oklahoma City, Oklahoma 73117 Tulsa, Oklahoma 74107 bears imprint of the office seal. (405) 239-7141 Fax (405) 239-2430 (918) 582-0985 Fax (918) 585-1549 By REPORT OF INVESTIGATION BY MEDICAL EXAMINER Date DECEDENT First-Middle-Last Names (Please avoid use of initials) Age Birth Date Race Sex CARINA SAUNDERS 19 7/17/1992 WHITE F HOME ADDRESS - No. - Street, City, State 922 W KYLE WAY, MUSTANG, OK EXAMINER NOTIFIED BY - NAME - TITLE (AGENCY, INSTITUTION, OR ADDRESS) DATE TIME DET. CADEL - BETHANY PD 10/13/2011 15:07 INJURED OR BECAME ILL AT (ADDRESS) CITY COUNTY TYPE OF PREMISES DATE TIME UNKNOWN Unknown Unknown LOCATION OF DEATH CITY COUNTY TYPE OF PREMISES DATE TIME 7101 NW 23RD ST. JUST WEST BETHANY OKLAHOMA FIELD 10/13/2011 10:30 FOUND FOUND BODY VIEWED BY MEDICAL EXAMINER CITY COUNTY TYPE OF PREMISES DATE TIME 901 N. STONEWALL OKLAHOMA CITY OKLAHOMA MORGUE 10/14/2011 9:00 IF MOTOR VEHICLE ACCIDENT: DRIVER PASSENGER PEDESTRIAN TYPE OF VEHICLE: AUTOMOBILE LIGHT TRUCK HEAVY TRUCK BICYCLE MOTORCYCLE OTHER: DESCRIPTION OF BODY RIGOR LIVOR EXTERNAL OBSERVATION NOSE MOUTH EARS Jaw Complete Color Beard Hair BLOOD EXTERNAL Neck Lateral PHYSICAL Absent Eyes: Color Mustache OTHER EXAMINATION Posterior Arms Passing Opacities Legs Passed Anterior Pupils: R L Decomposed Regional Body Length Body Weight Significant observations and injury documentations - (Please use space below) SEE AUTOPSY PROTOCOL Probable Cause of Death: Manner of Death: Case disposition: VIOLENT DEATH Natural Accident Autopsy Yes No Authorized by CHAI S. -

61-12-3. Office of Chief Medical Examiner Established; Appointment, Duties, Etc., of Chief Medical Examiner; Assistants and Employees; Promulgation of Rules
11/14/2019 West Virginia Code §61-12-3. Office of chief medical examiner established; appointment, duties, etc., of chief medical examiner; assistants and employees; promulgation of rules. (a) The office of chief medical examiner is hereby established within the division of health in the Department of Health and Human Resources. The office shall be directed by a chief medical examiner, who may employ pathologists, toxicologists, other forensic specialists, laboratory technicians, and other staff members, as needed to fulfill the responsibilities set forth in this article. (b) All persons employed by the chief medical examiner shall be responsible to him or her and may be discharged for any reasonable cause. The chief medical examiner shall specify the qualifications required for each position in the office of chief medical examiner, and each position shall be subject to rules prescribed by the secretary of the Department of Health and Human Resources. (c) The chief medical examiner shall be a physician licensed to practice medicine or osteopathic medicine in the State of West Virginia, who is a diplomat of the American board of pathology in forensic pathology, and who has experience in forensic medicine. The chief medical examiner shall be appointed by the director of the division of health to serve a five-year term unless sooner removed, but only for cause, by the Governor or by the director. (d) The chief medical examiner shall be responsible to the director of the division of health in all matters except that the chief medical examiner shall operate with independent authority for the purposes of: (1) The performance of death investigations conducted pursuant to section eight of this article; (2) The establishment of cause and manner of death; and (3) The formulation of conclusions, opinions or testimony in judicial proceedings. -

Medical Examiners and Coroners
Medical Examiners and Coroners As a medical-legal officer, the coroner or medical examiner is responsible for investigating and certifying specific types of death, and the records produced by these investigations can provide valuable data. Although which deaths are investigated is governed by state law, the types of deaths usually included are:1 • Deaths as a result of an accident, suicide, or homicide • Deaths with unusual or suspicious circumstances • Deaths from disease when “the death occurred suddenly and without warning, the decedent was not being treated by a physician, or the death was unattended”2 Information is collected in different ways in each state, depending on the system in place. For example, a state may have a medical examiner system, a coroner system, or a mixed system. The system may be centralized (controlled by one state office) or decentralized (controlled by county or regional offices). The difference between coroner and medical examiner systems varies by jurisdiction. In addition, the qualifications, skills, and activities of personnel cannot necessarily be determined from the title of the office. However, some differences between coroners and medical examiners may be generalized: • Coroners are usually elected and are not required to be physicians. If an autopsy is needed, a coroner will frequently consult with a pathologist or forensic pathologist. • Medical examiners, in most cases, are appointed and must be physicians. However, they may not be required to have special training in pathology or forensic pathology. Coroner and medical examiner records generally include: • Cause and manner of death • Results of autopsies and laboratory tests for the presence of alcohol or drugs • Circumstances leading to death However, the information collected on suicides and other deaths varies by jurisdiction. -

When Someone Dies
When Someone Dies Even when the passing of someone close to you is not unexpected, the list of tasks can be overwhelming. While we at Eddy & Schein wish you and yours a happy and long life, you may want to keep this list handy. Notifications DOCTOR A doctor is needed to establish the date and time of death and, where possible, the cause. If the person dies in the hospital, the in-hospital doctor automatically does this. If the doctor who is responsible (whether in the hospital or in hospice) suspects the cause of death was other than natural, the doctor is obligated to report it to the police who make a report and will notify the medical examiner. If the doctor does not come to the home, call 911 to report the death and the police and medical examiner will be dispatched. If there is no suspicion that the deceased died of other than natural causes, the body may be released to the funeral home. Otherwise, the body will go to the morgue and an authorized person will have to go to the medical examiner’s office to fill out papers and identify the body. FAMILY, FRIENDS, AND LEGAL REPRESENTATIVES Just after calling the doctor, inform immediate family as well as legal representatives, executors, or trustees, according to the will. People who previously acted as representatives through a Health Care Proxy or a Power of Attorney no longer have that responsibility. Make a list with telephone numbers and think about what you are going to say before you call. -

2008 Annual Report OFFICE of the CHIEF MEDICAL EXAMINER
2008 Annual Report OFFICE OF THE CHIEF MEDICAL EXAMINER MAYOR FENTY CONGRATULATES THE OFFICE OF THE CHIEF MEDICAL EXAMINER FOR OBTAINING PROVISIONAL ACCREDITATION FROM THE NATIONAL ASSOCIATION OF MEDICAL EXAMINERS (NAME) The Honorable Adrian M. Fenty, Mayor Neil Albert, City Administrator Government of the District of Columbia Executive Office of the Mayor Marie Lydie Y. Pierre-Louis, MD – Chief Medical Examiner Office of the Chief Medical Examiner DISTRICT OF COLUMBIA OFFICE OF THE CHIEF MEDICAL EXAMINER MISSION: The mission of the Office of the Chief Medical Examiner (OCME), for the District of Columbia, is to investigate and certify all deaths in the District of Columbia that occur by any means of violence (injury), and those that occur without explanation or medical attention, in custody, or which pose a threat to the public health. OCME provides forensic services to government agencies, health care providers and citizens in the Washington D.C. metropolitan area to ensure that justice is served and to improve the health and safety of the public. The Executive Leadership Team Marie-Lydie Y. Pierre-Louis, MD Chief Medical Examiner Sarah M. Colvin, MD Deputy Chief Medical Examiner Beverly A. Fields, Esq. Chief of Staff Lucas W. Zarwell, MFS Deputy Chief Toxicologist Peggy J. Fogg Management Services Officer Anna D. Francis Executive Assistant PRESENTED TO: The Honorable Adrian M. Fenty, Mayor, District of Columbia and The Council of the District of Columbia December 2009 A MESSAGE FROM THE CHIEF MEDICAL EXAMINER Calendar year 2008 was a year of great achievement for the OCME with a major focus on obtaining accreditation by the National Association of Medical Examiners (NAME). -

OFFICE of the CHIEF MEDICAL EXAMINER OCME POLICY 1910 MASSACHUSETTS AVENUE, S.E., Bldg 27 WASHINGTON, DC 20003 Last Updated: 2/1/08
DISTRICT OF COLUMBIA OFFICE OF THE CHIEF MEDICAL EXAMINER OCME POLICY 1910 MASSACHUSETTS AVENUE, S.E., Bldg 27 WASHINGTON, DC 20003 Last Updated: 2/1/08 AGENCY JURISDICTION 1.1 JURISDICTION: The Office of the Chief Medical Examiner functions pursuant to District of Columbia Code, Division I, Title 5, Ch.14. (DC Law 13-172). 1.2 DEATHS DETERMINATIONS AND INVESTIGATIONS; CREMATIONS. D.C. Code Sec. 5-1405. (a) The CME, other medical examiners, and medicolegal investigators (physician assistants or advanced practice registered nurses) licensed under subchapter V of Chapter 12 of Title 3, are authorized to make determinations of death. (b) Pursuant to regulations established by the Mayor, the following types of human deaths occurring in the District of Columbia shall be investigated by the OCME: (1) BY VIOLENCE: whether apparently homicidal, suicidal or accidental including deaths due to thermal, chemical, electrical or radiation injury and death due to criminal abortion, whether apparently self-induced or not; (2) SUDDENLY, UNEXPECTED OR UNEXPLAINED: not caused by readily recognizable disease, including sudden infant deaths or apparent sudden infant death syndrome (SIDS) for infants one year of age and younger; (3) UNDER SUSPICIOUS CIRCUMSTANCES: under suspicious circumstances; (4) WHEN A BODY IS TO BE CREMATED, DISSECTED, OR BURIED AT SEA: bodies are to be cremated, dissected, buried at sea or otherwise disposed of so as to be thereafter unavailable for examination; (5) BY DISEASE, INJURY OR ILLNESS RESULTING FROM EMPLOYMENT: related to disease resulting from employment or on-the job injury or illness; (6) BY DISEASE CONSTITUTING A THREAT TO PUBLIC HEALTH: related to disease which might constitute a threat to public health; (7) WHEN WARD OF DISTRICT OF COLUMBIA: persons who are wards of the District of Columbia government (“ward” means any person in the official custody of the District government, on a temporary or permanent basis, because of neglect, abuse, mental illness or mental retardation, D.C. -

Review of Deaths Among People Experiencing Homelessness in Multnomah County in 2018 This Report Is Dedicated to Those Who Have Died, Their Families and Friends
Domicile UnknownReview of deaths among people experiencing homelessness in Multnomah County in 2018 This report is dedicated to those who have died, their families and friends. To all those working to end the epidemic of homelessness. And to those who haven’t yet found a way off the street. Cover photo: An ever-present memorial to Street Roots vendors who have passed away. deaths of people who have a physical, mental health or substance use condition so severe that they have been unable to find shelter or housing. In other words, the people who need help the most are the ones we are most likely to be stepping over on the street and then ultimately counting in this report. And that is unacceptable. Yet, a second thing struck me that December night and gave me solace and hope. It was the people who carried the candles and rang the bells, who said the names of the dead with love and reverence, who were caring neighbors, community members, and the survivors, those who made it from the street into supportive housing. Together, we are creating a community movement to confront what is truly driving and keeping people on the streets: not the failing of an individual, but the failure of a prosperous economy to provide affordable housing and services for people with disabilities, and the failure of a healthcare system to provide adequate care and treatment. We know what works: housing with wraparound services close to where people live. And so, despite all the nonsense coming out of Last December on the longest night of the year, Washington D.C. -

Snohomish County Medical Examiner
Snohomish County Medical Examiner 9509 29th Ave West Everett, WA 98204 425-438-6200 Fax 425-438-6222 About Snohomish County Medical Examiner The primary purpose of the Snohomish County Medical Examiner's Office is to determine the cause and manner of death which are of concern to the public's health, safety and welfare. The Medical Examiner is a physician and forensic pathologist who is authorized by the state statute to investigate sudden, unexpected, violent, suspicious or unnatural deaths of persons who die within the geographical boundaries of Snohomish County. An accurate determination of the cause and manner of death is essential to achieve our goals: 1. The innocent shall be exonerated 2. Homicide shall be recognized 3. Criminal and civil court proceedings will be provided with documented, sound, and impartial medical evidence 4. Unrecognized hazards to public health and safety shall be revealed 5. Industrial hazards should be exposed http://www.snohomishcountywa.gov/198/Medical-Examiner MEDICAL EXAMINERS A medical examiner is licensed physicians who has specialized training and board certification in the field of Forensic Pathology. If you are interested in becoming a Medical Examiner, the first step is to become a physician. You should consult with career counselors at your University for the best approach given your interests. A medical examiner is a forensic pathologist. A forensic pathologist is a physician (“doctor”) who has performed about three years of post-medical school specialty training in anatomic pathology (a specialty area involving the study of disease in body tissues; you can Google “Pathologist” to learn more). The forensic pathologist is different than the usual hospital pathologist, because a fellowship (usually one year) specializing in forensics must also be completed. -

Where Laughter Flees
MEDICINE man who collapsed suddenly while re- pairing a TV antenna on the roof of his apartment building might have been blamed on long-standing heart disease if a pathologist from the county coroner's office hadn't arrived and noted two tiny holes in the back of the victim's head. Snooping around the building, he found several sparrows that had been killed with .22 caliber air-gun pellets. Using the shape of the wounds in the victim's head and the position in which he was lying, the examiner was able to calculate trajec- tories that led him to a neighbor who ad- mitted plinking at birds from his window. The heart-disease death thereupon be- came a case of involuntary manslaughter. Exoneration: A skillful autopsy, how- ever, can exonerate the falsely accused as well as help pin down the case against a suspect. In an Oklahoma case, the ap- Robert PhIllips—MedicA World News parent victim of a barroom fight was New York medical examiner Helpern: From autopsy table to test tube found to have a tiny aneurysm (a defect in the wall of an artery) in his brain. Where Laughter Flees communities in most states, deaths are Bleeding from the aneurysm had made usually investigated by elected coro- the man combative and he had picked a For all the histrionics and procedural ners, many of whom are not even M.D.'s. fight with the suspect. The hemorrhage, hairsplitting by prosecution and defense The leading forensic physicians belong to not the suspect's fists, caused his death.