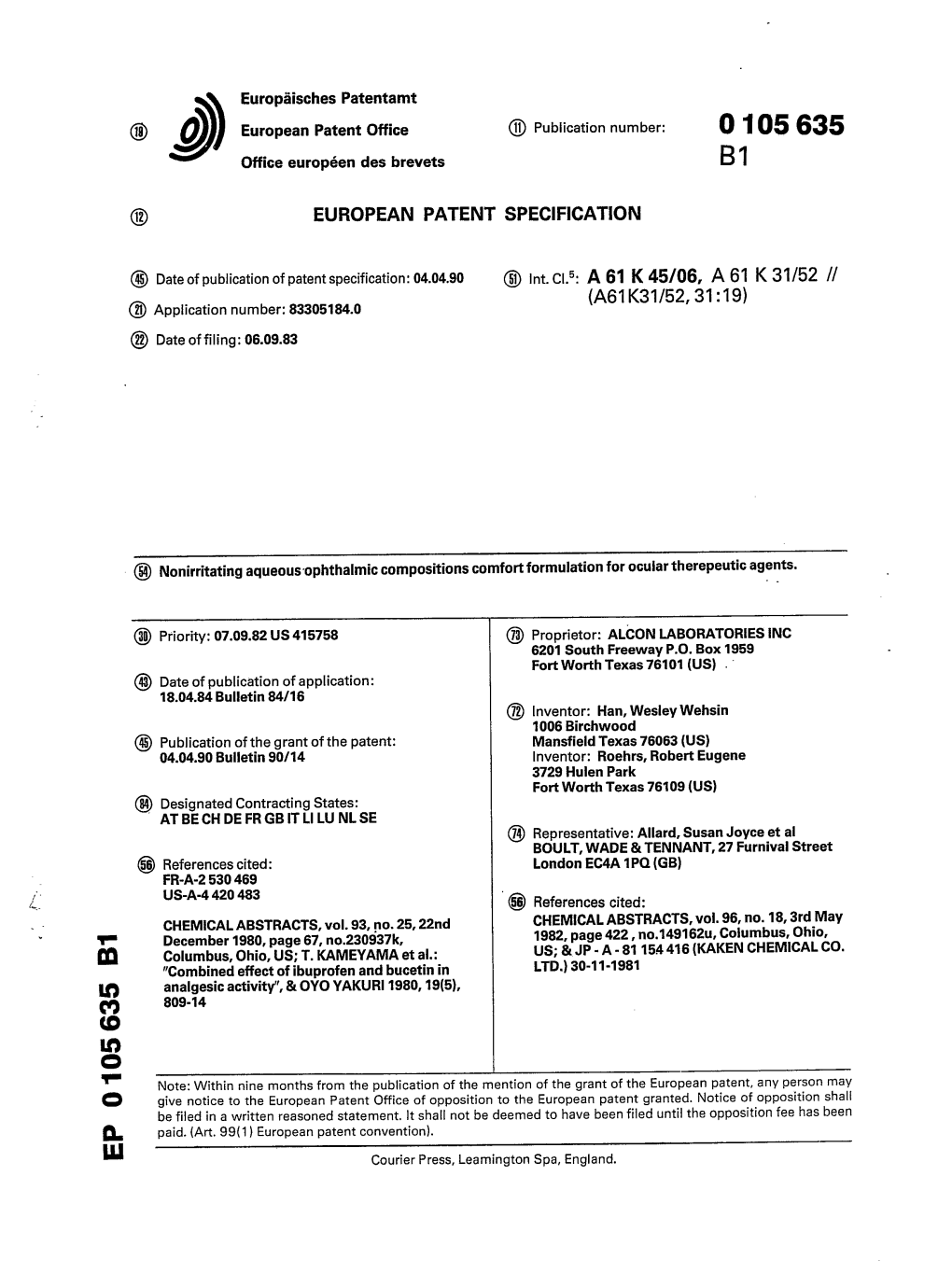
Nonirritating Aqueous Ophthalmic Compositions Comfort Formulation for Ocular Therepeutic Agents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

United States Patent (19) 11 Patent Number: 5,955,504 Wechter Et Al
USOO5955504A United States Patent (19) 11 Patent Number: 5,955,504 Wechter et al. (45) Date of Patent: Sep. 21, 1999 54 COLORECTAL CHEMOPROTECTIVE Marnett, “Aspirin and the Potential Role of Prostaglandins COMPOSITION AND METHOD OF in Colon Cancer, Cancer Research, 1992; 52:5575–89. PREVENTING COLORECTAL CANCER Welberg et al., “Proliferation Rate of Colonic Mucosa in Normal Subjects and Patients with Colonic Neoplasms: A 75 Inventors: William J. Wechter; John D. Refined Immunohistochemical Method.” J. Clin Pathol, McCracken, both of Redlands, Calif. 1990; 43:453-456. Thun et al., “Aspirin Use and Reduced Risk of Fatal Colon 73 Assignee: Loma Linda University Medical Cancer." N Engl J Med 1991; 325:1593-6. Center, Loma Linda, Calif. Peleg, et al., “Aspirin and Nonsteroidal Anti-inflammatory Drug Use and the Risk of Subsequent Colorectal Cancer.” 21 Appl. No.: 08/402,797 Arch Intern Med. 1994, 154:394–399. 22 Filed: Mar 13, 1995 Gridley, et al., “Incidence of Cancer among Patients With Rheumatoid Arthritis J. Natl Cancer Inst 1993 85:307-311. 51) Int. Cl. .......................... A61K 31/19; A61K 31/40; Labayle, et al., “Sulindac Causes Regression Of Rectal A61K 31/42 Polyps. In Familial Adenomatous Polyposis” Gastroenterol 52 U.S. Cl. .......................... 514/568; 514/569; 514/428; ogy 1991 101:635-639. 514/416; 514/375 Rigau, et al., “Effects Of Long-Term Sulindac Therapy On 58 Field of Search ..................................... 514/568, 570, Colonic Polyposis” Annals of Internal Medicine 1991 514/569, 428, 416, 375 11.5:952-954. Giardiello.et al., “Treatment Of Colonic and Rectal 56) References Cited Adenomas With Sulindac In Familial Adenomatous Poly U.S. -

Use of Aspirin and Nsaids to Prevent Colorectal Cancer
Evidence Synthesis Number 45 Use of Aspirin and NSAIDs to Prevent Colorectal Cancer Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 290-02-0021 Prepared by: University of Ottawa Evidence-based Practice Center at The University of Ottawa, Ottawa Canada David Moher, PhD Director Investigators Alaa Rostom, MD, MSc, FRCPC Catherine Dube, MD, MSc, FRCPC Gabriela Lewin, MD Alexander Tsertsvadze, MD Msc Nicholas Barrowman, PhD Catherine Code, MD, FRCPC Margaret Sampson, MILS David Moher, PhD AHRQ Publication No. 07-0596-EF-1 March 2007 This report is based on research conducted by the University of Ottawa Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 290-02-0021). Funding was provided by the Centers for Disease Control and Prevention. The findings and conclusions in this document are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This document is in the public domain and may be used and reprinted without permission except those copyrighted materials noted for which further reproduction is prohibited without the specific permission of copyright holders. -

Predicting Toxicity from Gene Expression with Neural Networks
Predicting Toxicity from Gene Expression with Neural Networks Peter Eastman1 and Vijay S. Pande1 1Department of Bioengineering, Stanford University, Stanford, CA 94305 Abstract We train a neural network to predict chemical toxicity based on gene expression data. The input to the network is a full expression profile collected either in vitro from cultured cells or in vivo from live animals. The output is a set of fine grained predictions for the presence of a variety of pathological effects in treated animals. When trained on the Open TG-GATEs database it produces good results, outperforming classical models trained on the same data. This is a promising approach for efficiently screening chemicals for toxic effects, and for more accurately evaluating drug candidates based on preclinical data. Introduction Predicting toxicity is a vital problem in many fields. One quarter of all drug candidates that reach phase II clinical trials ultimately fail because of toxicity[1]. Better methods to predict this in advance would spare patients from taking drugs that ultimately prove toxic, as well as saving enormous time and money. Toxic effects from industrial and household chemicals are also a major public health problem. Often they are tested only on animals, not humans, but animals can be a poor model for toxicity in humans[2]. Better methods to predict human toxicity would have major public health benefits. Many chemicals cause chronic rather than acute toxicity. It may take months or years for their effects to become apparent. Better methods to spot the early signs of chronic toxicity before clinical symptoms appear would allow clinical trials to be stopped sooner, and also would reduce the risk of toxic effects being missed. -

Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-Ones and 1,3,4- Oxadiazole-2-Thiones
Scientia Pharmaceutica (Sci. Pharm.) 71,331-356 (2003) O Osterreichische Apotheker-Verlagsgesellschaft m. b.H., Wien, Printed in Austria Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-ones and 1,3,4- Oxadiazole-2-thiones Aida A. ~l-~zzoun~'*,Yousreya A ~aklad',Herbert ~artsch~,~afaaA. 2aghary4, Waleed M. lbrahims, Mosaad S. ~oharned~. Pharmaceutical Sciences Dept. (Pharmaceutical Chemistry goup' and Pharmacology group2), National Research Center, Tahrir St. Dokki, Giza, Egypt. 3~nstitutflir Pharmazeutische Chemie, Pharrnazie Zentrum der Universitilt Wien. 4~harmaceuticalChemistry Dept. ,' Organic Chemistry Dept. , Helwan University , Faculty of Pharmacy, Ein Helwan Cairo, Egypt. Abstract A series of fenamate pyridyl or quinolinyl analogues of 1,3,4-oxadiazol-2-ones 5a-d and 6a-r, and 1,3,4-oxadiazole-2-thiones 5e-g and 6s-v, respectively, have been synthesized and evaluated for their analgesic (hot-plate) , antiinflammatory (carrageenin induced rat's paw edema) and ulcerogenic effects as well as plasma prostaglandin E2 (PGE2) level. The highest analgesic activity was achieved with compound 5a (0.5 ,0.6 ,0.7 mrnolkg b.wt.) in respect with mefenamic acid (0.4 mmollkg b.wt.). Compounds 6h, 61 and 5g showed 93, 88 and 84% inhibition, respectively on the carrageenan-induced rat's paw edema at dose level of O.lrnrnol/kg b.wt, compared with 58% inhibition of mefenamic acid (0.2mmoll kg b.wt.). Moreover, the highest inhibitory activity on plasma PGE2 level was displayed also with 6h, 61 and 5g (71, 70,68.5% respectively, 0.lmmolkg b.wt.) compared with indomethacin (60%, 0.01 mmolkg b.wt.) as a reference drug. -

Ibuprofen: Pharmacology, Therapeutics and Side Effects
Ibuprofen: Pharmacology, Therapeutics and Side Effects K.D. Rainsford Ibuprofen: Pharmacology, Therapeutics and Side Effects K.D. Rainsford Biomedical Research Centre Sheffield Hallam University Sheffield United Kingdom ISBN 978 3 0348 0495 0 ISBN 978 3 0348 0496 7 (eBook) DOI 10.1007/978 3 0348 0496 7 Springer Heidelberg New York Dordrecht London Library of Congress Control Number: 2012951702 # Springer Basel 2012 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifically for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provisions of the Copyright Law of the Publisher’s location, in its current version, and permission for use must always be obtained from Springer. Permissions for use may be obtained through RightsLink at the Copyright Clearance Center. Violations are liable to prosecution under the respective Copyright Law. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -

Analysis of Synthetic Chemical Drugs in Adulterated Chinese Medicines by Capillary Electrophoresis/ Electrospray Ionization Mass Spectrometry
RAPID COMMUNICATIONS IN MASS SPECTROMETRY Rapid Commun. Mass Spectrom. 2001; 15: 1473±1480 Analysis of Synthetic chemical drugs in adulterated Chinese medicines by capillary electrophoresis/ electrospray ionization mass spectrometry Hsing Ling Cheng, Mei-Chun Tseng, Pei-Lun Tsai and Guor Rong Her* Department of Chemistry, National Taiwan University, Taipei, Taiwan, R.O.C. Received 20 April 2001; Revised 20 June 2001; Accepted 21 June 2001 Sixteen synthetic chemical drugs, often found in adulterated Chinese medicines, were studied by capillary electrophoresis/UV absorbance CE/UV)and capillary electrophoresis/electrospray ioniza- tion mass spectrometry CE/ESI-MS). Only nine peaks were detected with CZE/UV, but on-line CZE/ MS provided clear identification for most compounds. For a real sample of a Chinese medicinal preparation, a few adulterants were identified by their migration times and protonated molecular ions. For coeluting compounds, more reliable identification was achieved by MS/MS in selected reaction monitoring mode. Micellar electrokinetic chromatography MEKC)using sodium dodecyl sulfate SDS)provided better separation than capillary zone electrophoresis CZE),and, under optimal conditions, fourteen peaks were detected using UV detection. In ESI, the interference of SDS was less severe in positive ion mode than in negative ion mode. Up to 20 mM SDS could be used in direct coupling of MEKC with ESI-MS if the mass spectrometer was operated in positive ion mode. Because of better resolution in MEKC, adulterants can be identified without the use of MS/MS. Copyright # 2001 John Wiley & Sons, Ltd. The use of Chinese medicines to maintain human health and provide the main basis for identification,generally lack the to cure disease has a long and rich history. -

Suprofen | Medchemexpress
Inhibitors Product Data Sheet Suprofen • Agonists Cat. No.: HY-B0270 CAS No.: 40828-46-4 Molecular Formula: C₁₄H₁₂O₃S • Molecular Weight: 260.31 Screening Libraries Target: PGE synthase Pathway: Immunology/Inflammation Storage: Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month SOLVENT & SOLUBILITY In Vitro DMSO : ≥ 100 mg/mL (384.16 mM) * "≥" means soluble, but saturation unknown. Mass Solvent 1 mg 5 mg 10 mg Concentration Preparing 1 mM 3.8416 mL 19.2079 mL 38.4157 mL Stock Solutions 5 mM 0.7683 mL 3.8416 mL 7.6831 mL 10 mM 0.3842 mL 1.9208 mL 3.8416 mL Please refer to the solubility information to select the appropriate solvent. In Vivo 1. Add each solvent one by one: 10% DMSO >> 40% PEG300 >> 5% Tween-80 >> 45% saline Solubility: ≥ 2.5 mg/mL (9.60 mM); Clear solution 2. Add each solvent one by one: 10% DMSO >> 90% (20% SBE-β-CD in saline) Solubility: ≥ 2.5 mg/mL (9.60 mM); Clear solution 3. Add each solvent one by one: 10% DMSO >> 90% corn oil Solubility: ≥ 2.5 mg/mL (9.60 mM); Clear solution BIOLOGICAL ACTIVITY Description Suprofen (TN-762) is a non-steroidal anti-inflammatory drug (NSAID). IC₅₀ & Target PGE synthase[1]. In Vitro Suprofen (TN-762) is an NSAID. Suprofen (TN-762) is an ibuprofen-type anti-inflammatory analgesic and antipyretic. It inhibits prostaglandin synthesis and has been proposed as an anti-arthritic. suprofen was clinically effective but the Page 1 of 2 www.MedChemExpress.com differential suppression of prostanoids favors 200mg which spares 6-keto PGF1a[1]. -

Computational Predictions of Glass-Forming Ability And
Article pubs.acs.org/molecularpharmaceutics Terms of Use Computational Predictions of Glass-Forming Ability and Crystallization Tendency of Drug Molecules † ‡ § † † Amjad Alhalaweh, Ahmad Alzghoul, Waseem Kaialy, Denny Mahlin, and Christel A. S. Bergström*, † Department of Pharmacy, Uppsala University, Uppsala Biomedical Centre, P.O. Box 580, SE-751 23 Uppsala, Sweden ‡ Department of Information Technology, Uppsala University, Lagerhyddsv.̈ 2, hus 1, Box 337, SE-751 05 Uppsala, Sweden § School of Pharmacy, Faculty of Science and Engineering, University of Wolverhampton, Wolverhampton WV1 1LY, United Kingdom ABSTRACT: Amorphization is an attractive formulation technique for drugs suffering from poor aqueous solubility as a result of their high lattice energy. Computational models that can predict the material properties associated with amorphiza- tion, such as glass-forming ability (GFA) and crystallization behavior in the dry state, would be a time-saving, cost-effective, and material-sparing approach compared to traditional experimental procedures. This article presents predictive models of these properties developed using support vector machine (SVM) algorithm. The GFA and crystallization tendency were investigated by melt-quenching 131 drug molecules in situ using differential scanning calorimetry. The SVM algorithm was used to develop computational models based on calculated molecular descriptors. The analyses confirmed the previously suggested cutoff molecular weight (MW) of 300 for glass-formers, and also clarified the extent to which MW can be used to predict the GFA of compounds with MW < 300. The topological equivalent of Grav3_3D, which is related to molecular size and shape, was a better descriptor than MW for GFA; it was able to accurately predict 86% of the data set regardless of MW. -

An Investigation of the Polymorphism of a Potent Nonsteroidal Anti-Inflammatory Drug Flunixin
CrystEngComm An Investigation of the Polymorphism of a Potent Nonsteroidal Anti-inflammatory Drug Flunixin Journal: CrystEngComm Manuscript ID CE-ART-10-2019-001619.R1 Article Type: Paper Date Submitted by the 09-Nov-2019 Author: Complete List of Authors: Liu, Hao; Wuhan Institute of Technology Yang, Xing; Wuhan Institute of Technology Wu, Shanyu; Nankai University Zhang, Mingtao; Purdue University System, IPPH; Nankai University, Parkin, Sean; University of Kentucky, Chemistry Cao, Shuang; Wuhan Institute of Technology Li, Tonglei; Purdue University, Yu, Faquan; Wuhan Institute of Technology Long, Sihui; Wuhan Institute of Technology, School of Chemical Engineering and Pharmacy Page 1 of 24 CrystEngComm An Investigation of the Polymorphism of a Potent Nonsteroidal Anti-inflammatory Drug Flunixin Hao Liu1, Xing Yang1, Shanyu Wu2, Mingtao Zhang2, Sean Parkin3, Shuang Cao1, Tonglei Li4, Faquan Yu1#, Sihui Long1* 1. H. Liu, X. Yang, Dr. S. Cao, Dr. F. Yu, Dr. S. Long Key Laboratory for Green Chemical Process of Ministry of Education Hubei Key Laboratory of Novel Reactor and Green Chemical Technology Hubei Engineering Research Center for Advanced Fine Chemicals School of Chemical Engineering and Pharmacy Wuhan Institute of Technology 206 1st Rd Optics Valley, East Lake New Technology Development District, Wuhan, Hubei 430205, China Phone: (027) 87194980 Email: [email protected] [email protected]; [email protected] 2. S. Wu, Dr. M. Zhang Computational Center for Molecular Science, College of Chemistry, Nankai University, Tianjin, China 3. Dr. S. Parkin Department of Chemistry, University of Kentucky, 1 CrystEngComm Page 2 of 24 Lexington, Kentucky 40506, United States 4. Dr. T. Li Department of Industrial and Physical Pharmacy, Purdue University, West Lafayette, Indiana 47907, United States H. -

Tramadol: a Review of Its Use in Perioperative Pain
Drugs 2000 Jul; 60 (1): 139-176 ADIS DRUG EVA L U AT I O N 0012-6667/00/0007-0139/$25.00/0 © Adis International Limited. All rights reserved. Tramadol A Review of its Use in Perioperative Pain Lesley J. Scott and Caroline M. Perry Adis International Limited, Auckland, New Zealand Various sections of the manuscript reviewed by: S.R. Abel, Indiana University Medical Centre, Indianapolis, Indiana, USA; S.S. Bloomfield, University of Cincinnati, Cincinnati, Ohio, USA; J.E. Caldwell, Department of Anesthesia, University of California, San Francisco, California, USA; K.A. Lehmann, Institute of Anaesthesiology and Intensive Care Medicine, University of Cologne, Cologne, Germany; L. Radbruch, Institute of Anaesthesiology and Intensive Care Medicine, University of Cologne, Cologne, Germany; K. Szymanski, Indiana University Medical Centre, Indianapolis, Indiana, USA; P. Tarkkila, Department of Anaesthesia, Helsinki University Centre Hospital, Helsinki, Finland; C.H. Wilder-Smith, Gastrointestinal Unit and Nociception Research Group, Berne, Switzerland. Data Selection Sources: Medical literature published in any language since 1993 on tramadol, identified using AdisBase (a proprietary database of Adis International, Auckland, New Zealand) and Medline. Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug. Search strategy: AdisBase search terms were ‘tramadol’ or ‘CG-315’ or ‘CG-315E’ or ‘U-26225A’. Medline search terms were ‘tramadol’. Searches were last updated 26 May 2000. Selection: Studies in patients with perioperative moderate to severe pain who received tramadol. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. -

BMJ Open Is Committed to Open Peer Review. As Part of This Commitment We Make the Peer Review History of Every Article We Publish Publicly Available
BMJ Open is committed to open peer review. As part of this commitment we make the peer review history of every article we publish publicly available. When an article is published we post the peer reviewers’ comments and the authors’ responses online. We also post the versions of the paper that were used during peer review. These are the versions that the peer review comments apply to. The versions of the paper that follow are the versions that were submitted during the peer review process. They are not the versions of record or the final published versions. They should not be cited or distributed as the published version of this manuscript. BMJ Open is an open access journal and the full, final, typeset and author-corrected version of record of the manuscript is available on our site with no access controls, subscription charges or pay-per-view fees (http://bmjopen.bmj.com). If you have any questions on BMJ Open’s open peer review process please email [email protected] BMJ Open Pediatric drug utilization in the Western Pacific region: Australia, Japan, South Korea, Hong Kong and Taiwan Journal: BMJ Open ManuscriptFor ID peerbmjopen-2019-032426 review only Article Type: Research Date Submitted by the 27-Jun-2019 Author: Complete List of Authors: Brauer, Ruth; University College London, Research Department of Practice and Policy, School of Pharmacy Wong, Ian; University College London, Research Department of Practice and Policy, School of Pharmacy; University of Hong Kong, Centre for Safe Medication Practice and Research, Department -

(12) United States Patent (10) Patent No.: US 6,472,433 B2 Wechter (45) Date of Patent: Oct
USOO6472433B2 (12) United States Patent (10) Patent No.: US 6,472,433 B2 Wechter (45) Date of Patent: Oct. 29, 2002 (54) METHOD FOR TREATMENT OF Variability of Inversion of (R)-Flurbiprofen in Different NFLAMMATION WITH R-NSAIDS Species, Sabine Menzel-Soglowek, Gerd Geisslinger, Win fried S. Beck, and Kay Brune-Journal of Pharmaceutical (75) Inventor: William J. Wechter, Ojai, CA (US) Sciences vol. 81, No. 9, Sep. 1992. Disposition and Pharmacokinetics of R-flurbiprofen in (73) Assignee: Loma Linda University Medical Three Species: Demonstration of R- to S-Flurbiprofen Center, Loma Linda, CA (US) Inversion in the Mouse, Rat and Monkey-William J. Wechter, E. David Murray, Jr. Karina M. Gibson, David D. (*) Notice: Subject to any disclaimer, the term of this Quiggle, and Douglas L. Leipold-Laboratory of Chemical patent is extended or adjusted under 35 Endocrinology, Loma Linda University School of Medicine, U.S.C. 154(b) by 0 days. 1998. Superaspirin, Jerome Groopman The New Yorker, Jun. 15, (21) Appl. No.: 09/797,022 1998 pp. 32–35. (22) Filed: Mar. 1, 2001 Building a Better Aspirin, Science, vol. 280, May 22, 1998. (65) Prior Publication Data R-Flurbiprofen Chemoprevention and Treatment of Intesti nal Adenomas in the APC Min/+ Mouse Model: Implica US 2001/0012849 A1 Aug. 9, 2001 tions for Prophylazis and Treatment of Colon Caner, Will iam Wechter, Darko Kantoci, E. David Murray, Jr. David D. Related U.S. Application Data Quiggle, Douglas D. Leipold, Karina M. Gibson, and John D. McCracker-Cancer Research 57, 4316-4324, Oct. 1, (63) Continuation of application No.