Mental Health Crisis Services Promoting Person-Centred and Rights-Based Approaches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
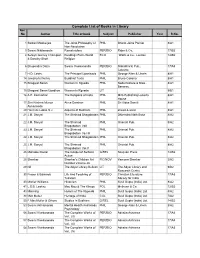
Complete List of Books in Library Acc No Author Title of Book Subject Publisher Year R.No
Complete List of Books in Library Acc No Author Title of book Subject Publisher Year R.No. 1 Satkari Mookerjee The Jaina Philosophy of PHIL Bharat Jaina Parisat 8/A1 Non-Absolutism 3 Swami Nikilananda Ramakrishna PER/BIO Rider & Co. 17/B2 4 Selwyn Gurney Champion Readings From World ECO `Watts & Co., London 14/B2 & Dorothy Short Religion 6 Bhupendra Datta Swami Vivekananda PER/BIO Nababharat Pub., 17/A3 Calcutta 7 H.D. Lewis The Principal Upanisads PHIL George Allen & Unwin 8/A1 14 Jawaherlal Nehru Buddhist Texts PHIL Bruno Cassirer 8/A1 15 Bhagwat Saran Women In Rgveda PHIL Nada Kishore & Bros., 8/A1 Benares. 15 Bhagwat Saran Upadhya Women in Rgveda LIT 9/B1 16 A.P. Karmarkar The Religions of India PHIL Mira Publishing Lonavla 8/A1 House 17 Shri Krishna Menon Atma-Darshan PHIL Sri Vidya Samiti 8/A1 Atmananda 20 Henri de Lubac S.J. Aspects of Budhism PHIL sheed & ward 8/A1 21 J.M. Sanyal The Shrimad Bhagabatam PHIL Dhirendra Nath Bose 8/A2 22 J.M. Sanyal The Shrimad PHIL Oriental Pub. 8/A2 Bhagabatam VolI 23 J.M. Sanyal The Shrimad PHIL Oriental Pub. 8/A2 Bhagabatam Vo.l III 24 J.M. Sanyal The Shrimad Bhagabatam PHIL Oriental Pub. 8/A2 25 J.M. Sanyal The Shrimad PHIL Oriental Pub. 8/A2 Bhagabatam Vol.V 26 Mahadev Desai The Gospel of Selfless G/REL Navijvan Press 14/B2 Action 28 Shankar Shankar's Children Art FIC/NOV Yamuna Shankar 2/A2 Number Volume 28 29 Nil The Adyar Library Bulletin LIT The Adyar Library and 9/B2 Research Centre 30 Fraser & Edwards Life And Teaching of PER/BIO Christian Literature 17/A3 Tukaram Society for India 40 Monier Williams Hinduism PHIL Susil Gupta (India) Ltd. -

2005 (Pdf, 4.7
2006 Global Citizenship Report Vital Responsible Ethical Global Governance Integrity Technology Product Innovative Reliable Operations Speed Agility Supply Expert Privacy Trustworthy Safety Collaborative Employee Citizenship Diversity Engaging Customer Relationship Accessible Social Meaningful Profitable Public Leadership Optimistic Forward Growth Inventive Essential Report About this report Table of contents GRI indicators* Scope 1. Introduction . 3 2.11-2.13, 2.15 This report describes HP’s HP’s global citizenship priorities . 3 3.19 global citizenship activities L e t t e r f ro m C EO M a r k H u rd . 4 1.1-1.2 worldwide. It charts HP’s progress in fiscal year 2005. H P p ro fi l e . 5 2.1-2.8, 3.7, EC1-EC2 Letter from Diana Bell . 7 1.1-1.2 Reporting year Global citizenship . 8 1.1, 3.6, 3.19 All data are for HP’s fiscal year 2005 (ending October 31, 2005), Economic value . 12 EC3, EC5, EC6, EC8, EC13 unless otherwise noted. 2. Governance and ethics . 15 Corporate governance . 15 3.1-3.2, 3.4, 3.6, 3.8 Currency and measurement All $ references in this document Business ethics . 16 3.7, HR10, SO2, SO7, PR9 are U.S. dollars, unless otherwise 3. Product environmental impacts . 18 3.19, EN14 noted. D e s i g n f o r E nvi ro n m e n t . 18 3.16-3.17, PR6 Measures used in the report are E n e rgy e f fi ci e n c y . 22 EN30 metric, except where stated. -
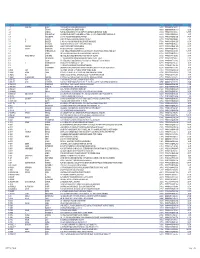
SR NO First Name Middle Name Last Name Address Pincode Folio
SR NO First Name Middle Name Last Name Address Pincode Folio Amount 1 A SPRAKASH REDDY 25 A D REGIMENT C/O 56 APO AMBALA CANTT 133001 0000IN30047642435822 22.50 2 A THYAGRAJ 19 JAYA CHEDANAGAR CHEMBUR MUMBAI 400089 0000000000VQA0017773 135.00 3 A SRINIVAS FLAT NO 305 BUILDING NO 30 VSNL STAFF QTRS OSHIWARA JOGESHWARI MUMBAI 400102 0000IN30047641828243 1,800.00 4 A PURUSHOTHAM C/O SREE KRISHNA MURTY & SON MEDICAL STORES 9 10 32 D S TEMPLE STREET WARANGAL AP 506002 0000IN30102220028476 90.00 5 A VASUNDHARA 29-19-70 II FLR DORNAKAL ROAD VIJAYAWADA 520002 0000000000VQA0034395 405.00 6 A H SRINIVAS H NO 2-220, NEAR S B H, MADHURANAGAR, KAKINADA, 533004 0000IN30226910944446 112.50 7 A R BASHEER D. NO. 10-24-1038 JUMMA MASJID ROAD, BUNDER MANGALORE 575001 0000000000VQA0032687 135.00 8 A NATARAJAN ANUGRAHA 9 SUBADRAL STREET TRIPLICANE CHENNAI 600005 0000000000VQA0042317 135.00 9 A GAYATHRI BHASKARAAN 48/B16 GIRIAPPA ROAD T NAGAR CHENNAI 600017 0000000000VQA0041978 135.00 10 A VATSALA BHASKARAN 48/B16 GIRIAPPA ROAD T NAGAR CHENNAI 600017 0000000000VQA0041977 135.00 11 A DHEENADAYALAN 14 AND 15 BALASUBRAMANI STREET GAJAVINAYAGA CITY, VENKATAPURAM CHENNAI, TAMILNADU 600053 0000IN30154914678295 1,350.00 12 A AYINAN NO 34 JEEVANANDAM STREET VINAYAKAPURAM AMBATTUR CHENNAI 600053 0000000000VQA0042517 135.00 13 A RAJASHANMUGA SUNDARAM NO 5 THELUNGU STREET ORATHANADU POST AND TK THANJAVUR 614625 0000IN30177414782892 180.00 14 A PALANICHAMY 1 / 28B ANNA COLONY KONAR CHATRAM MALLIYAMPATTU POST TRICHY 620102 0000IN30108022454737 112.50 15 A Vasanthi W/o G -

Neural Correlates of Inner Speech and Auditory Verbal Hallucinations: a Critical Review and Theoretical Integration 260
Durham E-Theses Cognitive mechanisms associated with clinical and non-clinical psychotic experiences Jones, Simon R. How to cite: Jones, Simon R. (2009) Cognitive mechanisms associated with clinical and non-clinical psychotic experiences, Durham theses, Durham University. Available at Durham E-Theses Online: http://etheses.dur.ac.uk/2053/ Use policy The full-text may be used and/or reproduced, and given to third parties in any format or medium, without prior permission or charge, for personal research or study, educational, or not-for-prot purposes provided that: • a full bibliographic reference is made to the original source • a link is made to the metadata record in Durham E-Theses • the full-text is not changed in any way The full-text must not be sold in any format or medium without the formal permission of the copyright holders. Please consult the full Durham E-Theses policy for further details. Academic Support Oce, Durham University, University Oce, Old Elvet, Durham DH1 3HP e-mail: [email protected] Tel: +44 0191 334 6107 http://etheses.dur.ac.uk 2 Gognitive meehanisms assdciated with cJinical and npn-c experiences Simon R. Jones BSe., PGDip., MA. The.cppyright of tWs thesU reste w^^^ the author or the uniyersity to which it was submitted. No quotation from, it, or iiifonnatioii derived' from it may be: published without the prior written consent of the author or university, and any inforihatioii derived from it should be aclaaowledged. Thesis isubmitted for the degree of Doctor of Philosophy Durham University, 2009 Declaration The research contained in this thesis was carried out by the author between 2005 and 2008 while a postgraduate student in the Department of Psychology at Durham University. -
Community Outreach Mental Health Services Promoting Person-Centred and Rights-Based Approaches
Technical package Technical package Community outreach mental health services Promoting person-centred and rights-based approaches I Technical package Community outreach mental health services Promoting person-centred and rights-based approaches Community outreach mental health services: promoting person-centred and rights-based approaches (Guidance and technical packages on community mental health services: promoting person-centred and rights-based approaches) ISBN 978-92-4-002580-6 (electronic version) ISBN 978-92-4-002581-3 (print version) © World Health Organization 2021 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization (http://www.wipo.int/amc/en/mediation/rules/). -

Group Housing
LIST OF ALLOTED PROPERTIES DEPARTMENT NAME- GROUP HOUSING S# RID PROPERTY NO. APPLICANT NAME AREA 1 60244956 29/1013 SEEMA KAPUR 2,000 2 60191186 25/K-056 CAPT VINOD KUMAR, SAROJ KUMAR 128 3 60232381 61/E-12/3008/RG DINESH KUMAR GARG & SEEMA GARG 154 4 60117917 21/B-036 SUDESH SINGH 200 5 60036547 25/G-033 SUBHASH CH CHOPRA & SHWETA CHOPRA 124 6 60234038 33/146/RV GEETA RANI & ASHOK KUMAR GARG 200 7 60006053 37/1608 ATEET IMPEX PVT. LTD. 55 8 39000209 93A/1473 ATS VI MADHU BALA 163 9 60233999 93A/01/1983/ATS NAMRATA KAPOOR 163 10 39000200 93A/0672/ATS ASHOK SOOD SOOD 0 11 39000208 93A/1453 /14/AT AMIT CHIBBA 163 12 39000218 93A/2174/ATS ARUN YADAV YADAV YADAV 163 13 39000229 93A/P-251/P2/AT MAMTA SAHNI 260 14 39000203 93A/0781/ATS SHASHANK SINGH SINGH 139 15 39000210 93A/1622/ATS RAJEEV KUMAR 0 16 39000220 93A/6-GF-2/ATS SUNEEL GALGOTIA GALGOTIA 228 17 60232078 93A/P-381/ATS PURNIMA GANDHI & MS SHAFALI GA 200 18 60233531 93A/001-262/ATS ATUULL METHA 260 19 39000207 93A/0984/ATS GR RAVINDRA KUMAR TYAGI 163 20 39000212 93A/1834/ATS GR VIJAY AGARWAL 0 21 39000213 93A/2012/1 ATS KUNWAR ADITYA PRAKASH SINGH 139 22 39000211 93A/1652/01/ATS J R MALHOTRA, MRS TEJI MALHOTRA, ADITYA 139 MALHOTRA 23 39000214 93A/2051/ATS SHASHI MADAN VARTI MADAN 139 24 39000202 93A/0761/ATS GR PAWAN JOSHI 139 25 39000223 93A/F-104/ATS RAJESH CHATURVEDI 113 26 60237850 93A/1952/03 RAJIV TOMAR 139 27 39000215 93A/2074 ATS UMA JAITLY 163 28 60237921 93A/722/01 DINESH JOSHI 139 29 60237832 93A/1762/01 SURESH RAINA & RUHI RAINA 139 30 39000217 93A/2152/ATS CHANDER KANTA -

OFFICE of the PRINCIPAL JUDGE, FAMILY COURTS (H.Qs)
OFFICE OF THE PRINCIPAL JUDGE, FAMILY COURTS (H.Qs), DWARKA, NEW DELHI ORDER In continuation of this office order no. 4932-4988/Cir./Admn./FC/DWK/2020 dated 31.07.2020 issued in compliance of the directions of the Hon’ble High Court of Delhi vider order No.26/DHC/2020 dated 30.07.2020 and in order to facilitate the hearing through Video Conferencing “Annexure-A” is the list of Readers of the Court of Principal Judges, Family Courts, Delhi/ New Delhi, their phone numbers and URL. Sd/- (Sanjay Garg-I) Principal Judge (H.Qs) Family Courts, Dwarka, New Delhi. No.5000-5056/Cir./Admn./FC/DWK/2020 Dated:03.08.2020 Copy forwarded for information and necessary action to:- 1. The Registrar General, High Court of Delhi, New Delhi. 2. All the Ld. Principal Judges, Ld. Additional Principal Judge, Ld. Judges, Family Courts, Delhi/ New Delhi. 3. The President/ Secretary, Dwarka Bar Association for their information. 4. Senior Administrative Officer Judicial, Family Courts (H.Qs), Dwarka, New Delhi. 5. All the Readers, Family Courts, Delhi/ New Delhi with the direction to bring this order in the notice of all the staff posted with them. 6. All the Branch In-charges, Family Courts, Delhi/ New Delhi with the direction to bring this order in the notice of all the staff posted with them. 7. Branch In-charge, Computer Branch, Family Courts (H.Qs), Dwarka, New Delhi with the direction to upload this order on official website. 8. PS to Principal Judge (H.Qs), Family Courts, Dwarka, New Delhi. Sd/- Principal Judge (H.Qs) Family Courts, Dwarka, New Delhi. -

Basicneeds: Applying Community Development Principles to Address Mental Health Challenges
Attachment G7 WORKING PAPER - DO NOT CITE OR DISTRIBUTE WITHOUT PERMISSION OF THE AUTHORS CASE STUDY: BASICNEEDS: APPLYING COMMUNITY DEVELOPMENT PRINCIPLES TO ADDRESS MENTAL HEALTH CHALLENGES Andrea Taylor, Innovations in Healthcare, Duke University Erin Escobar, Innovations in Healthcare, Duke University Krishna Udayakumar, Innovations in Healthcare, Duke University Prepared for: The Commonwealth Fund 2015 INTERNATIONAL SYMPOSIUM ON HEALTH CARE POLICY 1 Attachment G7 WORKING PAPER - DO NOT CITE OR DISTRIBUTE WITHOUT PERMISSION OF THE AUTHORS Abstract: As the burden of mental illness grows worldwide, access to treatment is not keeping pace. The need is particularly acute in low-resource communities that lack the infrastructure and trained workforce to provide comprehensive treatment. Using a community development approach, BasicNeeds’ Model for Mental Health and Development leverages existing resources in new ways to increase access to and effectiveness of mental health services. By mobilizing and coordinating government agencies, community organizations, volunteers, and people with mental illness and their families, BasicNeeds programs drive local ownership and system change. The model, which has now used in 12 low-income countries in Africa and Asia, has demonstrated many positive impacts in access to treatment, mental health outcomes, quality of life, and engagement in income-generating work. It might also prove to be a cost-effective approach in U.S. communities for addressing disparities in access and lack of care coordination in mental health management. BACKGROUND Roughly 450 million people worldwide suffer from mental illness. Seventy-five percent live in the developing world, where extreme poverty exacerbates the issue. Mental health problems represent a growing share of the global disease burden, yet access to effective treatment models is not keeping pace.i Communities often lack infrastructure to provide effective management, and the available treatment is often insufficient, expensive, poorly funded, and located far from the need. -
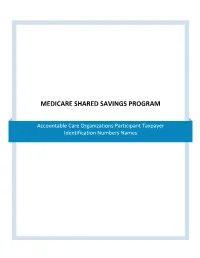
Medicare Shared Savings Program
MEDICARE SHARED SAVINGS PROGRAM Accountable Care Organizations Participant Taxpayer Identification Numbers Names MSSP ACO Participant TIN Names for 2012 and 2013 As of August 2013 TABLE OF CONTENTS A.M. Beajow, M.D. Internal Medicine Associates ACO, P.C. ..................................................................... 9 AAMC Collaborative Care Network ........................................................................................................... 9 Accountable Care Clinical Services PC ...................................................................................................... 9 Accountable Care Coalition of Caldwell County, LLC .............................................................................. 11 Accountable Care Coalition of Central Georgia, LLC ............................................................................... 11 Accountable Care Coalition of Coastal Georgia, LLC ............................................................................... 12 Accountable Care Coalition of DeKalb, LLC ............................................................................................. 12 Accountable Care Coalition of Eastern North Carolina, LLC ................................................................... 14 Accountable Care Coalition of Georgia, LLC ........................................................................................... 15 Accountable Care Coalition of Greater Athens Georgia II, LLC ............................................................... 15 Accountable Care -

Boekje Congres.Indd
PART TWO ABSTRACT BOOK 9 17 September Morning programm: Plenary session from 10.15 hours till 13.00 hours Chair: Elisa Carter , MBA (NL) CEO of GGzE Eindhoven en de Kempen (Mental Health organization, clinical, polyclinic and outreached care) Member of the advising board (RvZ) for the ministry of Health Care Netherlands Member of the board of commissioners for healthcare research (Bestuur ZoNMW) Shortly after I had accepted the CEO position at the mental heath institute Maastricht I met Professor Marius Romme. We had one hour to get acquainted. We exchanged briefl y each others career, some insights on the national heath care policy and the goals for mental health services in Maastricht. I was inspired by his passionate approach and logical reasoning while explaining his research on hearing voices. This inspiration help me to focus on an other way to organize the care in such a way that we can meet the Elisa Carter MBA demands of service users effectively. Hearing voices has been regarded by psychiatry as “auditory hallucinations” and as a symptom of schizophrenia. Traditionally the usual treatment for voice hearing has been major tranquillizers and specifi c medication administered to reduce hallucinations and other symptoms. However not everyone responds to this treatment. Ideally, most professionals would see all interventions as cooperate ventures between professionals and service user, but the perception of users is often different. Nearly always, the professional is in a position of power over the service user. In a culture where the person with a mental health problem expects the work done by a professional to be akin to arranging a ceremony with supernatural signifi cance, the power is not located in either the user or the professional. -

Er, No Harry Potter, but Plenty to Get Your Teeth Into… Great British Habitats
Spring 2018 Volume 25 Number 1 £4.00 Sales and subscriptions Tel 01600 891509 www.pccs-books.co.uk Information Asylum Collective the magazine for democratic psychiatry www.asylummagazine.org Er, no Harry Potter, but plenty to get your teeth into… Great British Habitats Two dwellings in the same area: working for everyone? Mark Bertram asylum spring 2018 page 3 The magazine for democratic psychiatry Volume 25, Number 1, Spring 2018 ISSN 0955 2030 CONTENTS Send letters, comments and submissions (including artwork, Editorial Helen Spandler 4 images etc.) to: [email protected] Big Farmer is Watching You Connie Sachs 4 Send creative writing and poetry submissions to: [email protected] “Bigger Pills to Swallow” Jeffrey Brooks 6 8 For reasons of editing and printing, please send any graphics as If it’s #MeToo, it can’t be #JustThem jpegs (or equivalent) with a resolution of at least 300dpi. Deborah A. Lee © Asylum Collective for one year after publication, and free of Letter to the Editor A disillusioned subscriber 10 copyright thereafter. Spreading the Word – 8 Years for HVN Greece 11 Managing Editor Members of HVN Greece Helen Spandler Creative Writing Poetry Andrew Jackson 14 General Editors Phil Virden, Lin Bigwood Creative Writing Prose Verity Dawn Hill 15 Creative Writing Editor William Park Outside or Inside: Two views on survivor culture 16 Business Manager William Park & Andrew Roberts Sam Taylor, PCCS Books The Other Side of Insanity Ash E. Rah 19 Members of the Asylum Collective Jill Anderson Ian Parker UNREST - film -

Space, Politics, and the Uncanny in Fiction and Social Movements
MADNESS AS A WAY OF LIFE: SPACE, POLITICS AND THE UNCANNY IN FICTION AND SOCIAL MOVEMENTS Justine Lutzel A Dissertation Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY December 2013 Committee: Ellen Berry, Advisor Francisco Cabanillas Graduate Faculty Representative Ellen Gorsevski William Albertini © 2013 Justine Lutzel All Rights Reserved iii ABSTRACT Ellen Berry, Advisor Madness as a Way of Life examines T.V. Reed’s concept of politerature as a means to read fiction with a mind towards its utilization in social justice movements for the mentally ill. Through the lens of the Freudian uncanny, Johan Galtung’s three-tiered systems of violence, and Gaston Bachelard’s conception of spatiality, this dissertation examines four novels as case studies for a new way of reading the literature of madness. Shirley Jackson’s The Haunting of Hill House unveils the accusation of female madness that lay at the heart of a woman’s dissatisfaction with domestic space in the 1950s, while Dennis Lehane’s Shutter Island offers a more complicated illustration of both post-traumatic stress syndrome and post-partum depression. Thomas Mann’s The Magic Mountain and Curtis White’s America Magic Mountain challenge our socially- accepted dichotomy of reason and madness whereby their antagonists give up success in favor of isolation and illness. While these texts span chronology and geography, each can be read in a way that allows us to become more empathetic to the mentally ill and reduce stigma in order to effect change.