Cataract Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Icare Eye Hospital Rate List 2015
ICARE EYE HOSPITAL & POST GRADUATE INSTITUTE E-3A, Sector – 26, Noida – 201301 Tel:- 0120-2477600 / 02, Counselor: 0120-2477621 Fax: 0120-2556389 / Appointments: 9811880015 Email: [email protected] / Web: www.icarehospital.org ICARE EYE HOSPITAL RATE LIST 2015 S No. PARTICULAR TARIFF (₹) I CONSULTATION NEW PATIENT VALID FOR 7 DAYS (FIRST TIME CONSULTATION : REGISTRATION + 1 ₹ 600/- CONSULTATION) 2 REVIEW CONSULTATION VALID FOR 7 DAYS ₹ 500/- 3 EMERGENCY CONSULTATION FOR 7 DAYS ₹ 800/- 4 LOW VISUAL AIDS ASSESSMENT CHARGES ₹ 600/- 5 VISION THERAPY CHARGES FOR PER SITTING ₹ 200/- 6 COST OF VISION THERAPY SOFTWARE (CD) ₹ 6,000/- 7 AMBLYOPIA (CD) ₹ 4,000/- II INVESTIGATIONS 1 Digital F.F.A (Fundus Fluoroscein Angiography)(Inclusive of Fundus photo) ₹ 2,500/- 2 Colour Fundus Photo - Digital ₹ 600/- 3 Colour Slit-lamp photo ₹ 600/- 4 Duplicate color prints (FFA/OCT/CLINICAL PHOTO) ₹ 300/- 5 Orthoptic ₹ 250/- 6 OCT (Optical Coherence Tomography) ₹ 2,500/- A Repeat OCT (within 2 months) with printout ₹ 800/- B Anterior Segment OCT ₹ 2,500/- 7 Ultrasonography (U/S) A A Scan – Single Eye ₹ 600/- B B Scan – Single Eye ₹ 1,000/- C UBM - Single Eye ₹ 1,500/- 8 Computerized field analysis A Humphrey Visual Fields (HVF) both eyes ₹ 1,500/- B Humphrey Visual Fields (HVF) One eye ₹ 750/- 9 Diurnal Variation of Tension (Day DVT ) A 5 times tension (Done in both eyes)] ₹ 500/- Page 1 10 Pachymetry (Both eyes) A Ultrasound (Central Corneal Thickness- CST) ₹ 600/- B Optical ₹ 600/- 11 Corneal Topography A Single Eye ₹ 1,000/- B Both Eyes ₹ 2,000/- 12 -

Local Coverage Determination (LCD): Diagnostic Evaluation and Medical Management of Moderate-Severe Dry Eye Disease (DED) (L36232)
Local Coverage Determination (LCD): Diagnostic Evaluation and Medical Management of Moderate-Severe Dry Eye Disease (DED) (L36232) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT NUMBER JURISDICTION STATE(S) First Coast Service Options, Inc. A and B MAC 09101 - MAC A J - N Florida First Coast Service Options, Inc. A and B MAC 09102 - MAC B J - N Florida First Coast Service Options, Inc. A and B MAC 09201 - MAC A J - N Puerto Rico Virgin Islands First Coast Service Options, Inc. A and B MAC 09202 - MAC B J - N Puerto Rico First Coast Service Options, Inc. A and B MAC 09302 - MAC B J - N Virgin Islands LCD Information Document Information LCD ID Original Effective Date L36232 For services performed on or after 11/22/2015 LCD Title Revision Effective Date Diagnostic Evaluation and Medical Management of For services performed on or after 01/08/2019 Moderate-Severe Dry Eye Disease (DED) Revision Ending Date Proposed LCD in Comment Period N/A N/A Retirement Date Source Proposed LCD N/A DL36232 Notice Period Start Date AMA CPT / ADA CDT / AHA NUBC Copyright 10/08/2015 Statement CPT codes, descriptions and other data only are Notice Period End Date copyright 2019 American Medical Association. All Rights 11/22/2015 Reserved. Applicable FARS/HHSARS apply. Current Dental Terminology © 2019 American Dental Association. All rights reserved. Copyright © 2019, the American Hospital Association, Created on 01/02/2020. Page 1 of 12 Chicago, Illinois. -

Cosmetic Lateral Canthoplasty: Lateral Topic Canthoplasty to Lengthen the Lateral Canthal Angle and Correct the Outer Tail of the Eye
Cosmetic Lateral Canthoplasty: Lateral Topic Canthoplasty to Lengthen the Lateral Canthal Angle and Correct the Outer Tail of the Eye Soo Wook Chae1, Byung Min Yun2 1BY Plastic Surgery Clinic, Seoul; 2Department of Plastic and Reconstructive Surgery, Jeju National University, Jeju, Korea There are many women who want larger and brighter eyes that will give a favorable impression. Correspondence: Soo Wook Chae Surgical methods that make the eye larger and brighter include double eyelidplasty, epican- BY Plastic Surgery Clinic, Wookyung Bldg. 5th Fl., 466 Apgujeong-ro, thoplasty, as well as lateral canthoplasty. Double eyelidplasty produces changes in the vertical Gangnam-gu, Seoul 06015, Korea dimension of the eyes, whereas epicanthoplasty and lateral canthoplasty create changes in Tel: +82-2-541-5522 the horizontal dimension of the eyes. Epicanthoplasty, a surgical procedure which enlarges Fax: +82-2-545-8743 the eye horizontally, is performed at the inner corner of the eye, whereas lateral canthoplasty E-mail: [email protected] enlarges the outer edge of the eye. In particular, if the slant of the palpebral fissure is raised and the horizontal dimension of the palpebral fissure is short, adjusting the slant of the pal- pebral fissure through lateral canthoplasty can achieve an enlargement of eye width and smoother features. Depending on the patient’s condition, even better results can be achieved if this procedure is performed in conjunction with other procedures, such as double eyelid- plasty, epicanthoplasty, eye roll formation surgery, fat graft, and facial bone contouring sur- gery. In this paper, the authors will introduce in detail their surgical method for a cosmetic lateral canthoplasty that lengthens the lateral canthal angle and corrects the outer tail of the eyes, in order to ease the unfavorable impression. -

Fixing Patients' Problems
CAN TABLETS WORK FOR EMR? P. 12 • CODING TIPS FOR CROSS-LINKING P. 16 A FRESH ANGLE ON RESIDENT TRAINING P. 68 • SIXTH CRANIAL NERVE DYSFUNCTION IN KIDS P. 72 Review of Ophthalmology Vol. XXIV, No. 4 • April 2017 • Fighting for Patient Care • Avoiding Problems Using OCT • Managing Refractive Surprises Problems • Optical Biometry Roundup Care • Avoiding No. 4 • April 2017 • Fighting for Patient Review of Ophthalmology Vol. XXIV, STEM THE TIDE OF EXCESSIVE TEARING P. 76 • POST-INJECTION IOP SPIKES P. 96 April 2017 reviewofophthalmology.com Fixing Patients’ Problems Expert surgeons give you the tools you need to succeed. ALSO INSIDE: Sizing Up Optical Biometers P. 58 001_rp0417_fc-WB.indd 1 3/24/17 12:52 PM VISIT US AT ASCRS BOOTH #1022 It’s all in CHOOSE A SYSTEM THAT EMPOWERS YOUR EVERY MOVE. Technique is more than just the motions. Purposefully engineered for exceptional versatility and high-quality performance, the WHITESTAR SIGNATURE® PRO Phacoemulsification System gives you the clinical flexibility, confidence and control to free your focus for what matters most in each procedure. How do you phaco? Join the conversation at WWW.ABBOTTPHACO.COM Rx Only INDICATIONS: The WHITESTAR SIGNATURE® PRO System is a modular ophthalmic microsurgical system that facilitates anterior segment (cataract) surgery. The modular design allows the users to configure the system to meet their surgical requirements. IMPORTANT SAFETY INFORMATION: Risks and complications of cataract surgery may include broken ocular capsule or corneal burn. This device is only to be used by a trained, licensed physician. ATTENTION: Reference the labeling for a complete listing of Indications and Important Safety Information. -

Primary External Dacryocystorhinostomy
11 Primary External Dacryocystorhinostomy Richard H. Hart, Suzanne Powrie, and Geoffrey E. Rose The watering eye may be the result of excessive tear production, abnor- malities of lid position or movement, lacrimal canalicular pump failure, or obstruction of the outfl ow tract. With external dacryocystorhinos- tomy (DCR), the lacrimal sac is directly incorporated into the lateral wall of the nose, so that the canaliculi drain directly into the nasal cavity. The aims of surgery are twofold: to eliminate fl uid and mucus reten- tion within the lacrimal sac and prevent sac enlargement (as a muco- cele) – the latter leading to intermittent viscous ocular discharge – and to bypass the higher hydraulic resistance of the nasolacrimal duct, thereby increasing tear conductance and aiding the relief of epiphora. Indications for Surgery 1. Primary acquired nasolacrimal duct obstruction 2. Secondary acquired nasolacrimal duct obstruction attributed, for example, to dacryolithiasis, endonasal surgery, infl ammatory nasal or sinus disease, or prior midfacial injury 3. Persistent congenital nasolacrimal duct obstruction, often after unsuccessful probing or intubation of the nasolacrimal duct 4. Functional obstruction of lacrimal outfl ow with decreased tear conductance as a result of: (a) Stenosis, but not occlusion, of the nasolacrimal duct (b) Lacrimal canalicular pump failure from age-related laxity of the lower eyelid, or after facial nerve palsy 5. Acute or chronic dacryocystitis; the former group requiring initial treatment with systemic antibiotics Surgical Principles External DCR should establish a low-resistance drainage pathway between the conjunctival tear sac and the nasal cavity, by conversion of the lacrimal sac into part of the lateral nasal wall. -
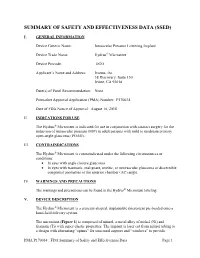
Summary of Safety and Effectivness (SSED)
SUMMARY OF SAFETY AND EFFECTIVENESS DATA (SSED) I. GENERAL INFORMATION Device Generic Name: Intraocular Pressure Lowering Implant Device Trade Name: Hydrus® Microstent Device Procode: OGO Applicant’s Name and Address: Ivantis, Inc. 38 Discovery, Suite 150 Irvine, CA 92618 Date(s) of Panel Recommendation: None Premarket Approval Application (PMA) Number: P170034 Date of FDA Notice of Approval: August 10, 2018 II. INDICATIONS FOR USE The Hydrus® Microstent is indicated for use in conjunction with cataract surgery for the reduction of intraocular pressure (IOP) in adult patients with mild to moderate primary open-angle glaucoma (POAG). III. CONTRAINDICATIONS The Hydrus® Microstent is contraindicated under the following circumstances or conditions: • In eyes with angle closure glaucoma • In eyes with traumatic, malignant, uveitic, or neovascular glaucoma or discernible congenital anomalies of the anterior chamber (AC) angle. IV. WARNINGS AND PRECAUTIONS The warnings and precautions can be found in the Hydrus® Microstent labeling. V. DEVICE DESCRIPTION The Hydrus® Microstent is a crescent-shaped, implantable microstent pre-loaded onto a hand-held delivery system. The microstent (Figure 1) is composed of nitinol, a metal alloy of nickel (Ni) and titanium (Ti) with super-elastic properties. The implant is laser cut from nitinol tubing to a design with alternating “spines” for structural support and “windows” to provide PMA P170034: FDA Summary of Safety and Effectiveness Data Page 1 outflow pathways for aqueous humor. After laser cutting, the shape of the implant is heat-set to a curvature intended to match the curvature of Schlemm’s canal and is electro- polished to create a smooth surface. The microstent is approximately 8 mm in overall length with major and minor axes of 292 µm and 185 µm, respectively. -

Operative Dictations in Ophthalmology Eric D
Operative Dictations in Ophthalmology Eric D. Rosenberg • Alanna S. Nattis Richard J. Nattis Editors Operative Dictations in Ophthalmology Editors Eric D. Rosenberg Alanna S. Nattis Ophthalmology Resident Cornea and Refractive Surgery Fellow Department of Ophthalmology Ophthalmic Consultants of Long Island New York Medical College Rockville Centre, NY, USA Valhalla, NY, USA Richard J. Nattis Chief of Ophthalmology and Clinical Professor Department of Ophthalmology Good Samaritan Hospital West Islip, NY, USA ISBN 978-3-319-45494-8 ISBN 978-3-319-45495-5 (eBook) DOI 10.1007/978-3-319-45495-5 Library of Congress Control Number: 2017932292 © Springer International Publishing Switzerland 2017 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, express or implied, with respect to the material contained herein or for any errors or omissions that may have been made. -

Curriculum Vitae
Kashkouli MB, CV CURRICULUM VITAE Mohsen Bahmani Kashkouli, MD Section Subject I Personal Information II 1. Executive Position 2. Journal Editor 3. Organizing a meeting 4. Journals’ reviewer, 5. Establishing an organization III Education IV Work Experience V Trained Fellows VI Edited Books/ Chapters VII Peer Reviewed Paper Publications VIII Courses Attended IX Directing Workshops/Courses/ Symposia X Conference Abstracts XI Invited (Guest) Speaker XII Awards XIII Innovations XIV Ongoing Research Projects XV Referees XVI Interests XVII Affiliations 1 Kashkouli MB, CV I. PERSONAL INFORMATION NAME: Mohsen Bahmani Kashkouli WORK ADDRESS University Hospital Private Office Rassoul Akram Hospital No.:49, West Brazil- South Sattarkhan-Niayesh Avenue Sheikhbahaee intersection, POBox: 14455-364 Tehran, Iran Tehran, Iran Phone: +98 21 66559595 Phone: +98 21 88065620 Fax: +98 21 66509162 Fax: +98 21 66558811 Email [email protected] DATE OF BIRTH: 09/January/1967 PLACE OF BIRTH: Gachsaran , Iran Language: Farsi, English, Turkish II. SCIENTIFIC & EXECUTIVE POSITIONS 1. Executive Positions 2. Professor, Head of Oculo-Facial Plastic Surgery, Rassoul Akram Hospital, Iran University of Medical Sciences (www.iums.ac.ir), Tehran, Iran. 3. Regional (Iran and Turkey) Vice President of Middle East African Council of Ophthalmology (MEACO).(www.meaco.org), Since Nov. 2019. 4. Vice President of Middle East African Council of Ophthalmology (MEACO) in Middle East (www.meaco.org), Since 2012. 5. Vice President, Middle East African Society of Ophthalmic Plastic and Reconstructive Surgery (MEASOPRS, www.meaco.org ), Since June 2016. 6. Scientific Coordinator, Middle East African Society of Ophthalmic Plastic and Reconstructive Surgery (MEASOPRS, www.meaco.org ), 2012-2016. 7. Scientific Director and chair of International relation section, Iranian Society of Ophthalmic Plastic and Reconstructive Suregry (IrSOPRS, www.irso.org/irsoprs), Tehran, Iran, Since 2007. -

Co-Managing Premium Iols: the Optometrist's Role COPE #26507-PO
Disclosures Walter O. Whitley, OD, MBA, FAAO has received consulting fees, honorarium or research funding from: Rapid Fire Grand Rounds • Alcon • Science Based Health COPE#52118- PO • Allergan • Shire • Bausch and Lomb • Sun Pharmaceuticals • Biotissue • TearLab Corporation • Beaver-Visitec • Tearscience Walter O. Whitley, OD, MBA, FAAO • Ocusoft Director of Optometric Services Virginia Eye Consultants • Publications Residency Program Supervisor – Advanced Ocular Care – Co-Chief Medical Editor PCO at Salus University – Review of Optometry – Contributing Editor – Optometry Times – Editorial Advisory Board Virginia Eye Consultants Pearls on Optometric Co-management Tertiary Referral Eye Care Since 1963 • John D. Sheppard, MD, MMSc • Walter Whitley, OD, MBA, FAAO • Get to know your surgeon • Stephen V. Scoper, MD • Mark Enochs, OD • David Salib, MD • Chris Kuc, OD, FAAO • Convey patient preferences, observations and • Elizabeth Yeu, MD • Cecelia Koetting, OD, FAAO • Thomas J. Joly, MD, PhD • Leanna Olennikov, OD conditions to your surgeon • Dayna M. Lago, MD • Chris Kruthoff, OD • Constance Okeke, MD, MSCE • Jillian Janes, OD • Inform your patients on your role in perioperative • Esther Chang, MD • Jay Starling, MD care • Samantha Dewundara, MD • Rohit Adyanthaya, MD • Successful co-management is the result of • Albert Cheung, MD continuous communication 1 Today’s Optometrists TODAY’S CATARACT PATIENT • In 2015, people aged 50 and older represented 45% of the US population1 “To be on the cutting edge of • There were approximately 4 million cataract procedures in 2015 and optometry, you need to be on the that number is expected to grow by 3% in 20166 cutting edge of science and Active Outgoing Still Digitally technology.” working savvy 1. -

Optical Coherence Tomography in Age-Related Macular Degeneration 1St Edition Principles 1
OPTICAL COHERENCE TOMOGRAPHY IN AGE- RELATED MACULAR DEGENERATION 1ST EDITION DOWNLOAD FREE Gabriel Coscas | 9783662505618 | | | | | Atlas of Retinal OCT: Optical Coherence Tomography Fluoroscopy Dental panoramic radiography X-ray motion analysis. Lay summary — Los Angeles Times September 4, White light is an example of a broadband source with lower power. OCT is based on low-coherence interferometry. October Any light that is outside the short coherence length will not interfere. An imaging approach to temporal OCT was developed by Claude Boccara's team in[24] with an acquisition of the images without beam scanning. Light with broad bandwidths can be generated by using superluminescent diodes or lasers with extremely short pulses femtosecond lasers. Bibcode : OExpr. April Learn how and when to remove this template message. Substances Angiogenesis Inhibitors. Synthetic array heterodyne detection offers another approach to this problem without the need for high dispersion. Free Shipping Free global shipping No minimum order. Therefore, translating one arm of the interferometer has two functions; depth scanning and a Doppler-shifted optical carrier are accomplished by pathlength variation. Optic Neuropathies and Papilledema 6. American Journal of Ophthalmology. We are always looking for ways to improve customer experience on Elsevier. Optical Coherence Tomography in Age-Related Macular Degeneration 1st edition Principles 1. Optical Coherence Tomography in Age-Related Macular Degeneration 1st edition Clinics. A wide range of fundus imaging modalities are now available, and this book explains the respective value of each technique. Intravascular OCT has been investigated for use in neurovascular applications, too, including imaging for guiding endovascular treatment of ischemic stroke and brain aneurysms. -

Leicester 14 & 15 June 2012 Programme & Abstract Book
Leicester 14 & 15 June 2012 Programme & abstract book About BOPSS BOPSS, the British Oculoplastic Surgery Society, was founded in 2000 with the aim of bringing together surgeons in the United Kingdom and Ireland who share an interest in Ophthalmic Plastic and Reconstructive Surgery, Lacrimal, Orbital and Aesthetic (cosmetic), Eyelid and Facial Surgery. Brian Leatherbarrow Richard Collin, Brian Leatherbarrow and Jane Olver, the Founding Executive Committee, President of BOPSS saw the necessity for such a society as a reflection of the interest in oculoplastic surgery as a sub-speciality of ophthalmology. Aims of BOPSS 1. To advance education, research and the quality of clinical practice in the area of ophthalmology known as oculoplastic surgery. This field comprises periocular, plastic reconstructive and aesthetic surgery, specialising in the eyelids, lacrimal system, orbit, upper and mid-face. 2. To provide an opportunity for Members to meet and discuss Oculoplastic Surgery. Ben Parkin 3. To provide information and advice to the public in order to gain a better understanding BOPSS Secretary of oculoplastic surgery. Members BOPSS has over 120 consultant oculoplastic surgeon members and holds an annual scientific meeting. In order to become a member of BOPSS, you need to send a written submission to the Executive Secretary. You can download the application form from the website (Membership > Application). Prior meetings BOPSS has organized meetings in Birmingham (2001, 2003 and 2005), Manchester (2002 David Verity BOPSS Treasurer and 2004), London (2006), Leeds (2007), Newcastle (2008), Cambridge (2009), Edinburgh (2010) and Cardiff (2011). The meeting in 2006 was co-organized by the European Society Of Ophthalmic Plastic And Reconstructive Surgery (ESOPRS). -

Aesthetic Surgery of the Face Surgical Anatomy of the Face, SMAS, Facial Spaces and Retaining Ligaments 79
SECTION I Aesthetic Surgery of the Face Surgical anatomy of the face, SMAS, facial spaces and retaining ligaments 79 6 Anatomy of the aging face Bryan Mendelson and Chin-Ho Wong intraoperative map for the surgeons to safely navigate to the SYNOPSIS area of interest to correct aging changes. This is most impor- Aging of the face is a multifactorial process that can be explained tant in addressing the overriding concern, being the course of on an anatomical basis. the facial nerve branches. An anatomical approach to surgical The face is constructed of five basic layers that are bound together rejuvenation of the face provides the way to obtaining a by a system of facial retaining ligaments. “natural” result that is lasting and with minimal morbidity. Fig. 6.1 Regions of the face. The mobile anterior face is functionally adapted for To facilitate the mobility needed for facial expression independent facial expressions and is separated from the relatively fixed lateral face (shaded), of the basic functions of the face, particularly of mastication, a which overlies masticatory structures. A vertical line of retaining ligaments (red) separates the anterior and lateral face. These ligaments are, from above: temporal, series of soft tissue spaces are incorporated into the architecture Regions of the face lateral orbital, zygomatic, masseteric, and mandibular ligaments. In the anterior Fig. 6.2 The face is constructed of five basic layers. This five-layered construct of the face. face, the mid-cheek is split obliquely into two separate functional parts by the is most evident in the scalp but exists in the rest of the face, with significant This arrangement, most clearly seen in the scalp, also exists in mid-cheek groove (dotted line) related to two cavities: the periorbital part above modification and compaction for functional adaptation.