Reference Committee K
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prescription Drug Management
Check out our new site: www.acllaboratories.com Prescription Drug Management Non Adherence, Drug Misuse, Increased Healthcare Costs Reports from the Centers for DiseasePrescription Control and Prevention (CDC) say Drug deaths from Managementmedication overdose have risen for 11 straight years. In 2008 more than 36,000 people died from drug overdoses, and most of these deaths were caused by prescription Nondrugs. Adherence,1 Drug Misuse, Increased Healthcare Costs The CDC analysis found that nearly 40,000 drug overdose deaths were reported in 2010. Prescribed medication accounted for almost 60 percent of the fatalities—far more than deaths from illegal street drugs. Abuse of painkillers like ReportsOxyContin from and the VicodinCenters forwere Disease linked Control to the and majority Prevention of the (CDC) deaths, say deaths from according to the report.1 medication overdose have risen for 11 straight years. In 2008 more than 36,000 people died from drug overdoses, and most of these deaths were caused by prescription drugs. 1 A health economics study analyzed managed care claims of more than 18 million patients, finding that patients undergoing opioid therapyThe CDCfor chronic analysis pain found who that may nearly not 40,000 be following drug overdose their prescription deaths were regimenreported in 2010. Prescribed medication accounted for almost 60 percent of the fatalities—far more than deaths have significantly higher overall healthcare costs. from illegal street drugs. Abuse of painkillers like OxyContin and Vicodin were linked to the majority of the deaths, according to the report.1 ACL offers drug management testing to provide information that can aid clinicians in therapy and monitoring to help improve patientA health outcomes. -
LC-MS for Pain Management Support
LC-MS for Pain Management Support Gwen McMillin, PhD, DABCC(CC,TC) University of Utah ARUP Laboratories Outline .Overview of drug testing, as a component of the therapeutic plan, in the management of chronic pain .A mini-SWOT analysis for application of LC- MS to pain management drug testing .Considerations for optimizing utility of LC-MS results Drug testing in pain management . Baseline testing, before initiating opioid therapy . Routine testing . Periodic, based on patient risk assessment . To evaluate changes . Therapeutic plan (drugs, formulations, dosing) . Clinical response (poor pain control, toxicity) . Clinical events (disease, surgery, pregnancy) . Patient behavior Objectives of drug testing Non- Detect and encourage Adherence appropriate drug use Detect and discourage Adherence inappropriate drug use Traditional approach . Immunoassay-based screen Screen . Confirm screen positive results with mass spectrometric method (GC-MS, LC-MS) Not appropriate for pain management Confirm + . Reflex testing leads to unnecessary expenses if the results are consistent with expectations, or if results are not used to make patient care decisions Confirm + . Confirmation of negative results may be more important than confirmation of positive results . Immunoassay-based screens may not be available Confirm + for specimens and drugs of interest Drugs monitored for pain management represent ~25% of “Top 200” prescriptions filled, 2011 .Analgesics .Anxiolytics, muscle . Hydrocodone (#1, 2, 14, 139) relaxants . Oxycodone (#45, 48, 121, 129, 196) -

An Active Metabolite of Hydrocodone
JPET Fast Forward. Published on August 30, 2013 as DOI: 10.1124/jpet.113.207548 JPET FastThis articleForward. has not Publishedbeen copyedited on and August formatted. 30, The 2013final version as DOI:10.1124/jpet.113.207548 may differ from this version. JPET #207548 In vivo Activity of Norhydrocodone: An Active Metabolite of Hydrocodone Downloaded from Dipesh M. Navani and Byron C. Yoburn Department of Pharmaceutical Sciences College of Pharmacy and Health Sciences jpet.aspetjournals.org St. John's University 8000 Utopia Parkway Queens, NY 11439 at ASPET Journals on October 3, 2021 1 Copyright 2013 by the American Society for Pharmacology and Experimental Therapeutics. JPET Fast Forward. Published on August 30, 2013 as DOI: 10.1124/jpet.113.207548 This article has not been copyedited and formatted. The final version may differ from this version. JPET #207548 Running Title: Norhydrocodone: An Active Metabolite of Hydrocodone. Corresponding author: Byron C. Yoburn, Ph.D. Department of Pharmaceutical Sciences College of Pharmacy and Health Sciences St. John's University 8000 Utopia Parkway Downloaded from Queens, NY 11439 Tel: 718-990-1623 jpet.aspetjournals.org Fax: 718-990-6036 Email: [email protected] at ASPET Journals on October 3, 2021 Number of text pages: 35 Number of tables: 3 Number of figures: 5 Number of references: 34 Number of words in the abstract: 248 Number of words in the introduction: 531 Number of words in the discussion: 863 Abbreviations: HYC, Hydrocodone; HYM, Hydromorphone; NHYC, Norhydrocodone; CYP, Cytochrome P450; DMAGO, [D-Ala2,N-MePhe4,Gly-ol5]Enkephalin; DPDPE, [D-Pen2,D- Pen5]Enkephalin; CL, Confidence limit. -

169 2016 Interim Meeting Science and Public Health - 1
169 2016 Interim Meeting Science and Public Health - 1 REPORTS OF THE COUNCIL ON SCIENCE AND PUBLIC HEALTH The following reports, 1–4, were presented by S. Bobby Mukkamala, MD, Chair: 1. URINE DRUG TESTING Reference committee hearing: see report of Reference Committee K. HOUSE ACTION: RECOMMENDATIONS ADOPTED AS FOLLOWS REMAINDER OF REPORT FILED See Policies H-95.985 and D-120.936 INTRODUCTION Over the past two decades, the rate of opioid prescribing, especially for patients with chronic non-cancer pain, has increased dramatically. It is estimated that between 9.6 and 11.5 million Americans are currently being prescribed long-term opioid therapy.1 The overall increase in prescribing has been associated with a parallel increase in unintentional overdoses and deaths from prescription opioids.2 In 2014, a total of 47,055 drug overdose deaths occurred in the United States; 61% of these involved some type of opioid, including heroin. Overdose deaths from heroin have quadrupled in recent years, and the majority of past year users of heroin report they used opioids in a nonmedical fashion prior to heroin initiation; hence, the availability of pharmaceutical opioids is relevant to the national heroin use and overdose death epidemics. In the most recent available report, benzodiazepines were involved in 31% of the opioid-related overdoses.3 Despite clinical recommendations to the contrary, the rate of opioid and benzodiazepine co-prescribing also continues to rise.3-5 Identifying patients at risk for drug misuse is a challenge. There is no definitive way for physicians to predict which of their patients will develop misuse problems with controlled substances. -

New High-Resolution Targeted Opioid Screen Superior Sensitivity and Specificity to Evaluate Adherence to Prescribed Opioid Therapy
4/7/2020 New High-Resolution Targeted Opioid Screen Superior Sensitivity and Specificity to Evaluate Adherence to Prescribed Opioid Therapy © MFMER | slide-1 Presenter: Paul J. Jannetto, PhD Associate Professor of Laboratory Medicine and Pathology Director, Clinical and Forensic Toxicology, Clinical Mass Spectrometry Lab and Metals Lab Department of Laboratory Medicine and Pathology at Mayo Clinic, Rochester, Minnesota © MFMER | slide-2 1 4/7/2020 Disclosures • None © MFMER | slide-3 Objectives • Describe the clinical utility and limitations of the following urine drug tests used to support pain management/monitoring of controlled substances: • Traditional opiate immunoassays • Mass spectrometry-based targeted screening assays • Define the metabolic profiles of opioids commonly used in pain management and discuss how to interpret screening/definitive test results. © MFMER | slide-4 2 4/7/2020 Opioid Crisis in America1 • Sale of opioid pain relievers (OPR) quadrupled between 1999 and 2010 • Enough OPR were prescribed in 2010to medicate every American adult around the clock (every 4 hours) for a month • Large number of patients (>40%) still report inadequate treatment of pain • Medical examiner reports also continue to show an increase in opioid related fatalities • Chronic pain costs up to $635 billion/year in medical treatment and lost productivity © MFMER | slide-5 Why Do Clinicians Use Urine Drug Tests (UDT) to Monitor Opioids? • Clinical Practice Guidelines: • American Society of Interventional Pain Physicians (ASIPP) Guidelines2,3 -

Therapeutic Class Overview Long-Acting Opioids
Therapeutic Class Overview Long-acting Opioids Therapeutic Class • Overview/Summary: As a class, opioid analgesics encompass a group of naturally occurring, semisynthetic, and synthetic drugs that stimulate opiate receptors and effectively relieve pain without producing loss of consciousness. The long-acting opioids and their Food and Drug Administration (FDA)-approved indications are outlined in Table 2.1-17 Previously, they were prescribed for the management of moderate to severe chronic pain; however, starting in March 2014, the FDA’s required label changes were made for most of the agents, updating their indication18. Currently, long- acting opioids are indicated for the management of pain severe enough to require daily, around-the- clock, long-term opioid treatment and for which alternative treatment options are inadequate. This change was made for all long-acting opioids in an effort to help prescribers and patients make better decisions about who benefits from opioids and also to help prevent problems associated with their use.18 In addition to indication changes, the long-acting opioid label must include statements that the long-acting opioid is not for “as needed” use, that it has an innate risk of addiction, abuse and misuse even at recommended doses, and finally it must include an update to the black box warning for increased risk of neonatal opioid withdrawal syndrome (NOWS). 18 Long-acting opioids are available in a variety of different dosage forms, and currently several agents are available generically. Pain is one of the most common and debilitating patient complaints, with persistent pain having the potentially to lead to functional impairment and disability, psychological distress, and sleep deprivation. -

Drug Plasma Half-Life and Urine Detection Window | January 2019
500 Chipeta Way | Salt Lake City, UT 84108-1221 Phone: (800) 522-2787 | Fax: (801) 583-2712 www.aruplab.com | www.arupconsult.com DRUG PLASMA HALF-LIFE AND URINE DETECTION WINDOW | JANUARY 2019 URINE- PLASMA DRUG, DRUG METABOLITE(S)* COMMON TRADE AND STREET NAMES, NOTES DETECTION HALF-LIFEt WINDOWt STIMULANTS Benzedrine, dexedrine, Adderall, Vyvanse, speed; could be methamphetamine Amphetamine 7–34 hours 1–5 days metabolite; if so, typically < 30 percent of parent Cocaine Coke, crack; parent drug rarely observed due to short half-life 0.7–1.5 hours < 1 day Benzoylecgonine Cocaine metabolite 5.5–7.5 hours 1–2 days Desoxyn, methedrine, Vicks inhaler (D- and L-isomers not resolved; low concentrations Methamphetamine expected if the source is Vicks); selegeline (Atapryl, Carbex, Eldepryl, Zelapar) 6–17 hours 1–5 days metabolite Methylenedioxyamphetamine (MDA) MDA 11–17 hours 1–3 days Methylenedioxyethylamphetamine (MDEA) MDEA, MDE, Eve 6–11 hours 1–3 days Methylenedioxymethamphetamine (MDMA) MDMA, XTC, ecstasy, Molly 6–10 hours 1–3 days Methylphenidate Ritalin, Concerta, Focalin, Metadate, Methylin 1.4–4.2 hours < 1 day Ritalinic acid Methylphenidate metabolite 1.8–2.5 hours < 1 day Phentermine Adipex-P, Lomaira, Qsymia 19–24 hours 1–5 days OPIOIDS Buprenorphine Belbuca, Buprenex, Butrans, Suboxone, Subutex, Sublocade, Zubsolv 26–42 hours 1–7 days Norbuprenorphine, Glucuronides Buprenorphine metabolites 15–150 hours 1–14 days Included in many preparations; morphine metabolite; may be a contaminant if < 2 Codeine 1.9–3.9 hours 1–3 days percent of morphine Fentanyl Actiq, Duragesic, Fentora, Lazanda, Sublimaze, Subsys, Ionsys 3–12 hours 1–3 days Norfentanyl Fentanyl metabolite 9–10 hours 1–3 days Heroin Diacetylmorphine, dope, smack, dust; parent drug not detected. -

Toxicology Reference Material
toxicology Toxicology covers a wide range of disciplines, including therapeutic drug monitoring, clinical toxicology, forensic toxicology (drug driving, criminal and coroners), drugs in sport and work place drug testing, as well as academia and research. Those working in the field have a professional interest in the detection and measurement of alcohol, drugs, poisons and their breakdown products in biological samples, together with the interpretation of these measurements. Abuse and misuse of drugs is one of the biggest problems facing our society today. Acute poisoning remains one of the commonest medical emergencies, accounting for 10-20% of hospital admissions for general medicine [Dargan & Jones, 2001]. Many offenders charged with violent crimes, or victims of violent crime may have been under the influence of drugs at the time the act was committed. The use of mind-altering drugs in the work place, or whilst in control of a motor vehicle places others in danger [Drummer, 2001]. Performance enhancing drugs in sport make for an uneven playing field and distract from the core ethic of sportsmanship. Patterns of drug abuse around the world are constantly evolving. They vary between geographies; from one country to another and even from region to region or population to population within countries. With a European presence, a wide reaching network of global customers and distributors, and activate participation in relevant professional societies, Chiron is well positioned to develop and deliver relevant, and current standards to meet customer demand in this challenging field. Chiron AS Stiklestadvn. 1 N-7041 Trondheim Norway Phone No.: +47 73 87 44 90 Fax No.: +47 73 87 44 99 E-mail: [email protected] Website: www.chiron.no Org. -

Bioidentical Hormones: Sound Science Or Bad Medicine
S. HRG. 110–129 Bioidentical Hormones: Sound Science or Bad Medicine HEARING BEFORE THE SPECIAL COMMITTEE ON AGING UNITED STATES SENATE ONE HUNDRED TENTH CONGRESS FIRST SESSION WASHINGTON, DC April 19, 2007 Serial No. 110–5 Printed for the use of the Special Committee on Aging ( Available via the World Wide Web: http://www.gpoaccess.gov/congress/index.html U.S. GOVERNMENT PRINTING OFFICE 37–150 PDF WASHINGTON : 2007 For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2104 Mail: Stop IDCC, Washington, DC 20402–0001 VerDate 0ct 09 2002 09:09 Sep 28, 2007 Jkt 000000 PO 00000 Frm 00001 Fmt 5011 Sfmt 5011 H:\DOCS\37150.TXT SAGING1 PsN: JOYCE SPECIAL COMMITTEE ON AGING HERB KOHL, Wisconsin, Chairman RON WYDEN, Oregon GORDON H. SMITH, Oregon BLANCHE L. LINCOLN, Arkansas RICHARD SHELBY, Alabama EVAN BAYH, Indiana SUSAN COLLINS, Maine THOMAS R. CARPER, Delaware MEL MARTINEZ, Florida BILL NELSON, Florida LARRY E. CRAIG, Idaho HILLARY RODHAM CLINTON, New York ELIZABETH DOLE, North Carolina KEN SALAZAR, Colorado NORM COLEMAN, Minnesota ROBERT P. CASEY, Jr., Pennsylvania DAVID VITTER, Louisiana CLAIRE McCASKILL, Missouri BOB CORKER, Tennessee SHELDON WHITEHOUSE, Rhode Island ARLEN SPECTER, Pennsylvania JULIE COHEN, Staff Director CATHERINE FINLEY, Ranking Member Staff Director (II) VerDate 0ct 09 2002 09:09 Sep 28, 2007 Jkt 000000 PO 00000 Frm 00002 Fmt 5904 Sfmt 5904 H:\DOCS\37150.TXT SAGING1 PsN: JOYCE C O N T E N T S Page Opening Statement of Senator Gordon H. -
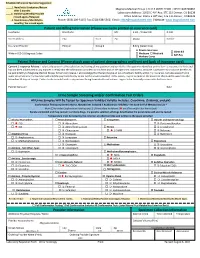
Patient and Billing Information (Please Use Name Printed on Insurance Card) Last Name First Name M.I
Schedule Adherence Specialist Suggestion: 1. New/Initial Evaluation/Return Magnolia Medical Group | CLIA # 06D2121590 | NPI# 1043769862 after 2 months. th 2. Stabilizing/Weekly/Possible Laboratory Address: 10515 E 40 Ave, STE 115 Denver, CO 80239 th missed appts./Relapsed Office Address: 10515 E 40 Ave, STE 115 Denver, CO80239 3. Maintenance/Monthly/2x Phone: (303) 209-5115| Fax: (720) 638-5562| Email: [email protected] | Website: www.magnoliamed.com monthly/ No missed appts. Patient and Billing Information (Please use name printed on insurance card) Last Name First Name M.I. S.S.N. / Patient ID D.O.B. Street Address City State Zip Phone Gender Insurance Provider Policy # Group # Billing (Select One) Private Insurance Client Bill Write in ICD-10 Diagnosis Codes Medicare Medicaid Self-Pay Workers Comp Patient Release and Consent (Please attach copy of patient demographics and front and back of insurance card) Consent / Insurance Release: I voluntarily consent to the collection and testing of my specimen and certify that the specimen identified on this form is my own; it is fresh and has not been adulterated in any manner. I certify that the information provided on this form and on the specimen container is accurate. I authorize my insurance benefits to be paid directly to Magnolia Medical Group, for service I receive. I acknowledge that the lab may be an out-of-network facility within my insurance. I am also aware that in some circumstances my insurance will send the payment directly to me for the service provided. If this occurs, I agree to endorse the insurance check and forward it to the lab within 30 days of receipt. -

WADA Technical Letter – TL15 HYDROMORPHONE
WADA Technical Letter – TL15 TL15 Document Number: Version Number: 2.0 (replaces TL2018/04) Written by: WADA LabEG Approved by: WADA LabEG* Date: 06 March 2018 Effective Date: 06 March 2018 *The approval by the WADA Executive Committee is applicable only to Technical Letters issued after November 2019. HYDROMORPHONE The World Anti-Doping Agency wishes to draw the attention of the Laboratories to the following issue that may affect Laboratory operations. This pertains, in particular, to the possible detection of the prohibited narcotic Hydromorphone in urine Samples resulting from the administration of the permitted drug Hydrocodone or resulting from the administration of high doses of either the Prohibited Threshold Substance Morphine or the permitted drug Codeine. 1. Detection of Hydromorphone as a result of the administration of Hydrocodone It is indeed reported in the literature1 that Hydrocodone is metabolized by O-demethylation to Hydromorphone and by N-demethylation to Norhydrocodone (Figure 1). In single-dose administration studies 1,2 of Hydrocodone, it was found that the levels of Norhydrocodone in urine were always higher than or equal to the parent compound, whereas the levels of Hydromorphone were lower. Additionally, Norhydrocodone was detected in urine for a longer time than Hydromorphone. In a different study involving a population of 25,200 subjects treated for chronic pain by multiple doses of hydrocodone/acetaminophen formulation3, Barakat et al. showed that the metabolic Hydromorphone/Hydrocodone ratio varied between 7.4 and 35.1%. Figure 1: Metabolic Pathway of Hydrocodone (Adapted from Valtier and Bebarta1) 1 Valtier S and Bebarta VS. Excretion Profile of Hydrocodone, Hydromorphone and Norhydrocodone in Urine Following Single Dose Administration of Hydrocodone to Healthy Volunteers. -

PPS443.V.1 Current Methodologies DOA.Indd
Current Methodologies for Drugs of Abuse Urine Testing | Page 1 Current Methodologies for Drugs of Abuse Urine Testing A White Paper from Biotage Abstract CONTENTS Analysis of drug panels in urine samples can be challenging, Section 1 Page and the trend towards larger panels including multiple drug classes compounds the issues faced during method Practical Considerations for LC/MS Method development. Development of a Comprehensive Urine Pain Panel This white paper examines a number of aspects of sample Part I Importance and Role of logP and pH 2 preparation, and their impact on the success of subsequent Part II ISOLUTE® SLE+ for Sample Preparation 3 LC-MS/MS analysis of broad urine panels. Part III EVOLUTE® EXPRESS for 3 Section 1 examines the applicability of various sample Sample Preparation preparation techniques: supported liquid extraction, reverse Part IV Properties of Analytes 4 phase SPE and mixed-mode SPE, to the various classes of drugs Part V Experiments in Hydrolysis 5 extracted. In addition, hydrolysis approaches: enzyme type and Part VI Results by Drug Class 9 protocol used (time, temperature), are compared. Part VII Removal of Conditioning and 10 Mixed-mode (reverse phase/cation exchange) SPE is widely Equilibrating Steps for EVOLUTE® used for extraction of basic drug classes from urine, but the EXPRESS ABN and CX sorbents inclusion of drugs and metabolites that exhibit ‘non-typical’ Part VIII General Recommendations 11 functionality within urine panels can be problematic. Part IX References 11 Section 2 examines the impact of various parameters (interference wash strength, elution solvent composition) on Section 2 analyte retention, elution and extract cleanliness with particular focus on zwitterionic (gabapentin, pregabalin) and non-ionic Multivariate Intermolecular Properties Analyzed by (carisoprodol, meprobamate) drugs.