Final Report Budget Analysis of Ministry of Health And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Surveillance System in Nepal
IED threat in Nepal Geneva 16- 19, 2015 Nepal Nepal was declared minefield free in 201 IEDs continue to injure and kill people in Nepal Device-wise Casualties by Victim -activated Explosions (90% casualties from IEDs: 2006-2014) © UNICEF/NEPIMAGE 01299/ H LAURENGE IEDs – Smaller © UNICEF/NEPIMAGE 01277/ H LAURENGE IEDs replaced guns and fire arms in Nepal © UN EOC NEPAL IEDs - bigger © UN EOC NEPAL UNICEF/NEPIMAGE 01265/ H LAURENGE UNICEF/NEPIMAGE 01263/ H LAURENGE © © © UNICEF/NEPIMAGE 01237/ H LAURENGE IEDs IEDs – much bigger © UNICEF/NEPIMAGE 01283/ H LAURENGE IED – not anti-vehicle mine 38 people died and 78 were injured © SDC/NEPAL/ T NGUDUP Command Detonated Devices Surveillance system in Nepal • 2005: Development of a Media-based Surveillance System on Victim-Activated Explosions in 75 districts • 2006: Transformed into a Community-based active Surveillance System • 2008: Expanded to Intentional Explosions • 2009: Expanded to all types of Armed Violence (including: small arms, mines, ERW and other IEDs) The term 'Surveillance' as used in the public health field, refers to the ongoing and systematic collection, analysis, interpretation and dissemination of health information. Surveillance system and MRE, VA and IEDD Who Target populations How many Severity/Justification Where Geographic targeting Why Appropriate messages What Type of devices Surveillance When Time pattern Prioritization ! ISS and Mine Risk Education 2005-07 2008-2011 2008-2011 2012-13 LAURENGE UNICEF/NEPIMAGE 01260/ H UNICEF/NEPIMAGE © © ‘Socket Bomb’ ‘Sutali Bomb’ -

Feasibility Study of Kailash Sacred Landscape
Kailash Sacred Landscape Conservation Initiative Feasability Assessment Report - Nepal Central Department of Botany Tribhuvan University, Kirtipur, Nepal June 2010 Contributors, Advisors, Consultants Core group contributors • Chaudhary, Ram P., Professor, Central Department of Botany, Tribhuvan University; National Coordinator, KSLCI-Nepal • Shrestha, Krishna K., Head, Central Department of Botany • Jha, Pramod K., Professor, Central Department of Botany • Bhatta, Kuber P., Consultant, Kailash Sacred Landscape Project, Nepal Contributors • Acharya, M., Department of Forest, Ministry of Forests and Soil Conservation (MFSC) • Bajracharya, B., International Centre for Integrated Mountain Development (ICIMOD) • Basnet, G., Independent Consultant, Environmental Anthropologist • Basnet, T., Tribhuvan University • Belbase, N., Legal expert • Bhatta, S., Department of National Park and Wildlife Conservation • Bhusal, Y. R. Secretary, Ministry of Forest and Soil Conservation • Das, A. N., Ministry of Forest and Soil Conservation • Ghimire, S. K., Tribhuvan University • Joshi, S. P., Ministry of Forest and Soil Conservation • Khanal, S., Independent Contributor • Maharjan, R., Department of Forest • Paudel, K. C., Department of Plant Resources • Rajbhandari, K.R., Expert, Plant Biodiversity • Rimal, S., Ministry of Forest and Soil Conservation • Sah, R.N., Department of Forest • Sharma, K., Department of Hydrology • Shrestha, S. M., Department of Forest • Siwakoti, M., Tribhuvan University • Upadhyaya, M.P., National Agricultural Research Council -
Final Evaluation Combating Exploitive Child Labor Through Education in Nepal: Naya Bato Naya Paila Project -New Path New Steps
FINAL (AFTER COMMENTS) Independent Final Evaluation Combating Exploitive Child Labor through Education in Nepal: Naya Bato Naya Paila Project -New Path New Steps- USDOL Cooperative Agreement No: IL-19513-09-75-K Report prepared by: Dr. Martina Nicolls April 2013 Table of Contents ACKNOWLEDGMENTS ............................................................................................................ v LIST OF ACRONYMS ............................................................................................................... vi EXECUTIVE SUMMARY ........................................................................................................... 1 Country Context ................................................................................................................................................... 1 Relevance: Shifting Project Priorities ................................................................................................................... 1 Effectiveness ........................................................................................................................................................ 2 Efficiency .............................................................................................................................................................. 3 Impact .................................................................................................................................................................. 3 Sustainability ....................................................................................................................................................... -

Club Health Assessment MBR0087
Club Health Assessment for District 325A1 through April 2021 Status Membership Reports Finance LCIF Current YTD YTD YTD YTD Member Avg. length Months Yrs. Since Months Donations Member Members Members Net Net Count 12 of service Since Last President Vice Since Last for current Club Club Charter Count Added Dropped Growth Growth% Months for dropped Last Officer Rotation President Activity Account Fiscal Number Name Date Ago members MMR *** Report Reported Report *** Balance Year **** Number of times If below If net loss If no When Number Notes the If no report on status quo 15 is greater report in 3 more than of officers thatin 12 months within last members than 20% months one year repeat do not haveappears in two years appears appears appears in appears in terms an active red Clubs less than two years old SC 138770 Bansbari 07/12/2019 Active 41 15 0 15 57.69% 26 0 N 1 $600.02 P,MC 138952 Bargachhi Green City 07/12/2019 Active 25 1 0 1 4.17% 24 4 N 5 142398 Biratnagar A One 08/09/2020 Active 32 32 0 32 100.00% 0 2 N 1 M,MC,SC 138747 Biratnagar Birat Medical 07/12/2019 Active 21 1 0 1 5.00% 20 3 N 3 90+ Days P,S,T,M,VP 138954 Biratnagar Capital City 07/12/2019 Active 20 0 0 0 0.00% 20 21 1 None N/R 90+ Days MC,SC M,MC,SC 140415 Biratnagar Entrepreneur 01/06/2020 Active 18 0 0 0 0.00% 20 10 2 R 10 90+ Days M 139007 Biratnagar Greater 07/12/2019 Active 31 8 3 5 19.23% 26 1 4 3 N 3 Exc Award (06/30/2020) VP 139016 Biratnagar Health Professional 07/12/2019 Active 26 4 1 3 13.04% 23 1 0 N 3 Exc Award (06/30/2020) 138394 Biratnagar Mahanagar -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -

Impact of Climate Change on Rice Production and Local Adaptation
B.B. Khadka et al. (2020) Int. J. Soc. Sc. Manage. Vol. 7, Issue-4: 202-213 DOI: 10.3126/ijssm.v7i4.32472 Research Article Impact of Climate Change on Rice Production and Local Adaptation Practices Adopted by Farmers in Surkhet, Nepal Bakhat Bahadur Khadka1*, Hridesh Sharma2, Ananta Prakash Subedi3, Shiva Chandra Dhakal3 1Ministry of Land Management, Agriculture and Co-operative-Karnali province, Nepal 2SAFBIN project-Caritas Nepal, 3Agriculture and Forestry University- Chitwan, Nepal Article Information Abstract Received: 07 July 2020 A total of 120 sample households were randomly selected from two municipalities Revised version received: 15 October 2020 of Surkhet for this study. The primary data were collected by survey questionnaire, Accepted: 18 October 2020 direct observation, FGD whereas secondary data of rainfall temperature and rice Published: 29 October 2020 productivity were collected from different sources. Majority of farmers perceived increase in temperature, decrease in rainfall frequency, decrease in rainfall duration Cite this article as: and increase in flooding hazard during rainy season. Trends analysis of temperature B.B. Khadka et al. (2020) Int. J. Soc. Sc. Manage. and rainfall data over 35 years (1980-2015) showed, increasing trends of maximum 7(4): 202-213. DOI: 10.3126/ijssm.v7i4.32472 temperature (0.06oC/year) and minimum temperature (0.03oC/year) which were in the line with the farmer's perception. Trend analysis revealed that total annual *Corresponding author precipitation was decreasing by 3.77 mm/year while monsoon rainfall was Bakhat Bahadur Khadka, increasing by 0.051 mm/year. About 20% respondents had clear knowledge on Ministry of Land Management, Agriculture and Co- climate change. -

WRRP Annual Report 2019
Centre for Agro-Ecology and Development (CAED) Women's Reproductive Rights Program (WRRP) Discussion with women's network in Sisautia village in Sarlahi district Report # 5 July – December 2019 Women's Reproductive Rights Program (WRRP) Centre for Agro-Ecology and Development (CAED) P.O. BOX: 4555, Kathmandu, Nepal Phone: 01- 5180340, Khotang: 036-420729, Sarlahi: 046-521312 Email: [email protected], [email protected], [email protected] Website: www.wrrpnepal.org / www.Caed.org.np 1 Table of Contents 1. INTRODUCTION .............................................................................................................................. 4 2. BROADER CONTEXT ........................................................................................................................ 4 3. MAJOR ACHIEVEMENTS .................................................................................................................. 6 4. METHODOLOGY .............................................................................................................................. 8 MANAGEMENT ............................................................................................................................ 8 MCC MOBILIZATION .................................................................................................................... 8 5. LEARNINGS ..................................................................................................................................... 9 ADAPTATION OF THE LEARNINGS .................................................................................................... -

Provincial Summary Report Province 3 GOVERNMENT of NEPAL
National Economic Census 2018 GOVERNMENT OF NEPAL National Economic Census 2018 Provincial Summary Report Province 3 Provincial Summary Report Provincial National Planning Commission Province 3 Province Central Bureau of Statistics Kathmandu, Nepal August 2019 GOVERNMENT OF NEPAL National Economic Census 2018 Provincial Summary Report Province 3 National Planning Commission Central Bureau of Statistics Kathmandu, Nepal August 2019 Published by: Central Bureau of Statistics Address: Ramshahpath, Thapathali, Kathmandu, Nepal. Phone: +977-1-4100524, 4245947 Fax: +977-1-4227720 P.O. Box No: 11031 E-mail: [email protected] ISBN: 978-9937-0-6360-9 Contents Page Map of Administrative Area in Nepal by Province and District……………….………1 Figures at a Glance......…………………………………….............................................3 Number of Establishments and Persons Engaged by Province and District....................5 Brief Outline of National Economic Census 2018 (NEC2018) of Nepal........................7 Concepts and Definitions of NEC2018...........................................................................11 Map of Administrative Area in Province 3 by District and Municipality…...................17 Table 1. Number of Establishments and Persons Engaged by Sex and Local Unit……19 Table 2. Number of Establishments by Size of Persons Engaged and Local Unit….….27 Table 3. Number of Establishments by Section of Industrial Classification and Local Unit………………………………………………………………...34 Table 4. Number of Person Engaged by Section of Industrial Classification and Local Unit………………………………………………………………...48 Table 5. Number of Establishments and Person Engaged by Whether Registered or not at any Ministries or Agencies and Local Unit……………..………..…62 Table 6. Number of establishments by Working Hours per Day and Local Unit……...69 Table 7. Number of Establishments by Year of Starting the Business and Local Unit………………………………………………………………...77 Table 8. -
Nepal National Association of Rural Municipality Association of District Coordination (Muan) in Nepal (NARMIN) Committees of Nepal (ADCCN)
Study Organized by Municipality Association of Nepal National Association of Rural Municipality Association of District Coordination (MuAN) in Nepal (NARMIN) Committees of Nepal (ADCCN) Supported by Sweden European Sverige Union "This document has been financed by the Swedish "This publication was produced with the financial support of International Development Cooperation Agency, Sida. Sida the European Union. Its contents are the sole responsibility of does not necessarily share the views expressed in this MuAN, NARMIN, ADCCN and UCLG and do not necessarily material. Responsibility for its content rests entirely with the reflect the views of the European Union'; author." Publication Date June 2020 Study Organized by Municipality Association of Nepal (MuAN) National Association of Rural Municipality in Nepal (NARMIN) Association of District Coordination Committees of Nepal (ADCCN) Supported by Sweden Sverige European Union Expert Services Dr. Dileep K. Adhikary Editing service for the publication was contributed by; Mr Kalanidhi Devkota, Executive Director, MuAN Mr Bimal Pokheral, Executive Director, NARMIN Mr Krishna Chandra Neupane, Executive Secretary General, ADCCN Layout Designed and Supported by Edgardo Bilsky, UCLG world Dinesh Shrestha, IT Officer, ADCCN Table of Contents Acronyms ....................................................................................................................................... 3 Forewords ..................................................................................................................................... -
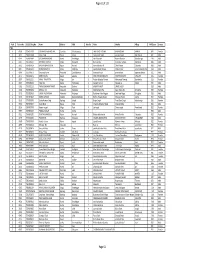
TSLC PMT Result
Page 62 of 132 Rank Token No SLC/SEE Reg No Name District Palika WardNo Father Mother Village PMTScore Gender TSLC 1 42060 7574O15075 SOBHA BOHARA BOHARA Darchula Rithachaupata 3 HARI SINGH BOHARA BIMA BOHARA AMKUR 890.1 Female 2 39231 7569013048 Sanju Singh Bajura Gotree 9 Gyanendra Singh Jansara Singh Manikanda 902.7 Male 3 40574 7559004049 LOGAJAN BHANDARI Humla ShreeNagar 1 Hari Bhandari Amani Bhandari Bhandari gau 907 Male 4 40374 6560016016 DHANRAJ TAMATA Mugu Dhainakot 8 Bali Tamata Puni kala Tamata Dalitbada 908.2 Male 5 36515 7569004014 BHUVAN BAHADUR BK Bajura Martadi 3 Karna bahadur bk Dhauli lawar Chaurata 908.5 Male 6 43877 6960005019 NANDA SINGH B K Mugu Kotdanda 9 Jaya bahadur tiruwa Muga tiruwa Luee kotdanda mugu 910.4 Male 7 40945 7535076072 Saroj raut kurmi Rautahat GarudaBairiya 7 biswanath raut pramila devi pipariya dostiya 911.3 Male 8 42712 7569023079 NISHA BUDHa Bajura Sappata 6 GAN BAHADUR BUDHA AABHARI BUDHA CHUDARI 911.4 Female 9 35970 7260012119 RAMU TAMATATA Mugu Seri 5 Padam Bahadur Tamata Manamata Tamata Bamkanda 912.6 Female 10 36673 7375025003 Akbar Od Baitadi Pancheswor 3 Ganesh ram od Kalawati od Kalauti 915.4 Male 11 40529 7335011133 PRAMOD KUMAR PANDIT Rautahat Dharhari 5 MISHRI PANDIT URMILA DEVI 915.8 Male 12 42683 7525055002 BIMALA RAI Nuwakot Madanpur 4 Man Bahadur Rai Gauri Maya Rai Ghodghad 915.9 Female 13 42758 7525055016 SABIN AALE MAGAR Nuwakot Madanpur 4 Raj Kumar Aale Magqar Devi Aale Magar Ghodghad 915.9 Male 14 42459 7217094014 SOBHA DHAKAL Dolakha GhangSukathokar 2 Bishnu Prasad Dhakal -

Download 3.58 MB
Due Diligence Report – Social Safeguards Project Number: 51190-001 February 2020 Nepal: Disaster Resilience of Schools Project Construction of Schools in Dolakha District (Reconstruction Phase II) Prepared by Central Level Project Implementation Unit (Education) of National Reconstruction Authority for the Asian Development Bank. This Due Diligence Report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. TABLE OF CONTENTS ABBREVIATIONS .................................................................................................................................. III I. INTRODUCTION ..............................................................................................................................1 II. APPROACH AND METHODOLOGY IN DUE DILIGENCE .....................................................2 III. SCOPE OF LIKELY IMPACTS OF THE PROJECTS ............................................................2 A. INVOLUNTARY RESETTLEMENT .......................................................................................................2 B. INDIGENOUS PEOPLES ........................................................... -
![आकाश स िंह राम प्रघट स िंह राकेश स िंह P]G Axfb"/ Af]Xf]/F L;Krg](https://docslib.b-cdn.net/cover/4868/p-g-axfb-af-xf-f-l-krg-1494868.webp)
आकाश स िंह राम प्रघट स िंह राकेश स िंह P]G Axfb"/ Af]Xf]/F L;Krg
खुला प्रलतयोलगता配मक परीक्षाको वीकृ त नामावली वबज्ञापन नं. : २०७७/७८/३४ (कर्ाला ी प्रदेश) तह : ३ पदः कलनष्ठ सहायक (गो쥍ड टेटर) सम्륍मललत हुन रोल नं. उ륍मेदवारको नाम उ륍मेदवारको नाम (देवनागरीमा) ललंग थायी म्ि쥍ला थायी न. पा. / गा.वव.स बािेको नाम बाबुको नाम चाहेको समूह 1 AAKASH SINGH आकाश स िंह Male ख쥍ु ला Banke Nepalgunj Sub-Metropolitian City राम प्रघट स िंह राके श स िंह 2 AIN BAHADUR BOHARA P]g axfb"/ af]xf]/f Male ख쥍ु ला Jumla Patarasi l;krGb| af]xf]/f ;fk{ nfn af]xf]/f 3 AISHWARYA SHAHI ऐश्वर् य शाही Female ख쥍ु ला Surkhet Gurbhakot असिपाल शाही बृज ब शाही 4 AJAR ALI MIYA अजार अली समर्ााँ Male ख쥍ु ला Dailekh Bhairabi आशादली समर्ााँ मर्ु यदली समर्ााँ 5 ALINA BAIGAR Plngf a}uf/ Female ख쥍ु ला, दललत Surkhet Birendranagar bn axfb"/ a}uf/ /d]z a}uf/ 6 ANIL BISHWOKARMA असिल सिश्वकमाय Male ख쥍ु ला, दललत Salyan Marke VDC ^f]k axfb'/ ;"gf/ शासलकराम सिश्वकमाय 7 ANUP BISHWOKARMA cg"k ljZjsdf{ Male ख쥍ु ला, दललत Dang Deokhuri Gadhawa alx/f sfdL t]h] sfdL 8 ARBINA THARU clj{gf yf? Female ख쥍ु ला Bardiya Geruwa dga'emfjg yf? x]jtnfn yf? 9 BABITA PANGALI alatf k+ufnL Female ख쥍ु ला Surkhet Jarbuta dlg/fd k+ufnL ofd k|;fb k+ufnL 10 BHAKTA RAJ BHATTA eSt /fh e§ Male ख쥍ु ला Doti Ranagaun 6Lsf /fd e§ nId0f k||;fb e§ 11 BHANU BHAKTA ROKAYA भािभु क्त रोकार्ा Male ख쥍ु ला Bajura Himali उसजरे रोकार्ा चन्द्र बहादरु रोकार्ा 12 BHARAT NEPALI भरर् िेपाली Male ख쥍ु ला, दललत Surkhet Gutu राम स िं दमाई गाेेपाल स िं िेपाली 13 BHARAT RAWAL भरर् रािल Male ख쥍ु ला Mugu Khatyad RM जर् रु रािल जर्लाल रािल 14 BHUPENDRA BAHADUR CHAND e"k]Gb| axfb"/ rGb Male ख쥍ु ला Dailekh sinhasain etm