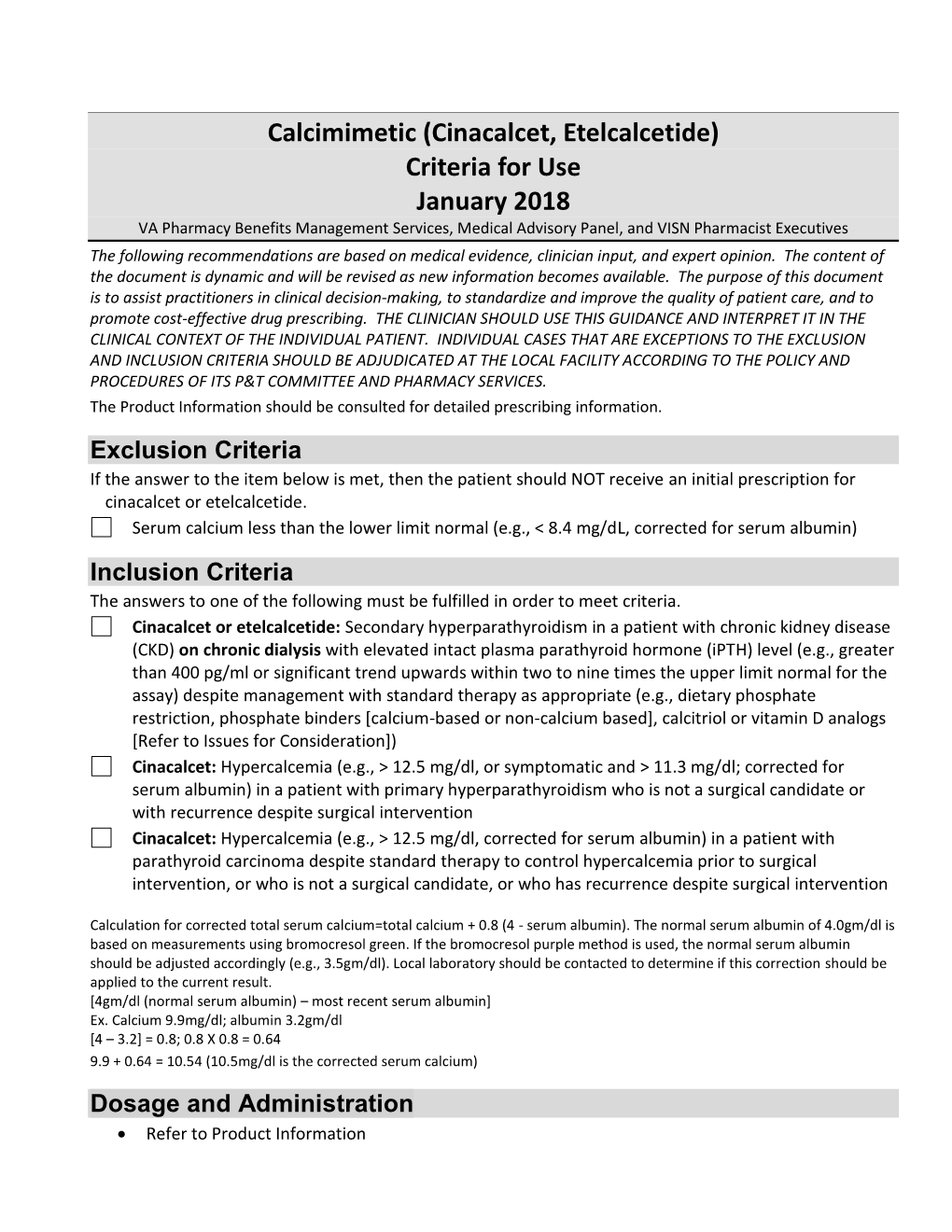
Calcimimetic (Cinacalcet, Etelcalcetide) Criteria for Use January 2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PARSABIV (Etelcalcetide) RATIONALE for INCLUSION IN
PARSABIV (etelcalcetide) RATIONALE FOR INCLUSION IN PA PROGRAM Background Parsabiv (etelcalcetide) is a calcimimetic agent that increases the sensitivity of the calcium-sensing receptor to activation by extracellular calcium. These calcium-sensing receptors are on the parathyroid hormone gland and are the principal regulators of PTH (parathyroid hormone) synthesis and secretion. By increasing the sensitivity of the calcium sensing receptors, a reduction in PTH secretion is achieved. Reductions in PTH are associated with a decrease in bone turnover and bone fibrosis in patients with CKD (chronic kidney disease) on hemodialysis and uncontrolled secondary hyperparathyroidism (HPT) (1). Regulatory Status FDA approved indication: Parsabiv is a calcium-sensing receptor agonist indicated for treatment of secondary hyperparathyroidism (HPT) in adult patients with chronic kidney disease (CKD) on hemodialysis (1). Limitation of Use: Parsabiv has not been studied in adult patients with parathyroid carcinoma, primary hyperparathyroidism, or with CKD who are not on hemodialysis and is not recommended for use in these populations (1). Initial treatment with Parsabiv is contraindicated if serum calcium is less than the lower limit of the normal range. Life threatening events and fatal outcomes were reported due to hypocalcemia. Hypocalcemia can prolong QT interval, lower the threshold for seizures, and cause hypotension, worsening heart failure, and/or arrhythmia. Monitor serum calcium carefully for the occurrence of hypocalcemia during treatment. Once the maintenance dose has been established, serum calcium should be measured monthly for patients with secondary hyperparathyroidism with CKD on hemodialysis (1). In patients with secondary hyperparathyroidism with chronic kidney disease who are on hemodialysis, serum calcium should be measured within 1 week of starting Parsabiv, and intact parathyroid hormone (iPTH) should be measured 4 weeks after initiation or dose adjustment of Parsabiv (1). -

Calcimimetic Use in Dialysis-Dependent
Kidney360 Publish Ahead of Print, published on August 25, 2020 as doi:10.34067/KID.0003042020 Calcimimetic Use in Dialysis-Dependent Medicare Fee-for-Service Beneficiaries and Implications for Bundled Payment Mark Gooding1, Pooja Desai2, Holly Owens3, Allison A. Petrilla1, Mahesh Kambhampati1, Zach Levine1, Joanna Young1, Jack Fagan1, Robert Rubin4 1. Avalere Health, Washington, DC 2. Amgen, Inc., Global Health Economics, Thousand Oaks, CA 3. Amgen, Inc., US Government Affairs and Policy, Washington, DC 4. Georgetown University, Bethesda, MD Corresponding Author: Mark Gooding Avalere Health 1201 New York Avenue, NW Suite 1000 Washington, DC 2005 202-355-6096 [email protected] Copyright 2020 by American Society of Nephrology. Abstract: Background: Dialysis-dependent patients with secondary hyperparathyroidism (SHPT) may require calcimimetics to reduce parathyroid hormone levels to treatment goals. Medicare currently utilizes the Transitional Drug Add-on Payment Adjustment (TDAPA) designation under the ESRD Prospective Payment System (“bundled payment”) to pay for calcimimetics (the first products eligible for the adjustment); this payment designation for calcimimetics is expected to conclude after 2020. This study explores variability in calcimimetic use across key patient characteristics and its potential impact on policy options for incorporating calcimimetics permanently into the bundle. Methods: This descriptive analysis used the 100% sample of Medicare FFS Part B (outpatient) 2018 claims to describe national, regional, and patient-level variation (including race, dual eligibility, and dialysis vintage) in calcimimetic utilization among dialysis-dependent beneficiaries. Results: A total of 373,874 beneficiaries were analyzed, 28% had >90 days of calcimimetic use during 2018. At the national level, the proportion of dialysis patients utilizing calcimimetics was roughly 80% higher in African-American vs. -

Parsabiv, INN-Etelcalcetide
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Parsabiv 2.5 mg solution for injection Parsabiv 5 mg solution for injection Parsabiv 10 mg solution for injection 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Parsabiv 2.5 mg solution for injection Each vial contains 2.5 mg of etelcalcetide (as hydrochloride) in 0.5 mL of solution. Each mL contains 5 mg etelcalcetide. Parsabiv 5 mg solution for injection Each vial contains 5 mg of etelcalcetide (as hydrochloride) in 1 mL of solution. Each mL contains 5 mg etelcalcetide. Parsabiv 10 mg solution for injection Each vial contains 10 mg of etelcalcetide (as hydrochloride) in 2 mL of solution. Each mL contains 5 mg etelcalcetide. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection. Clear colourless solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Parsabiv is indicated for the treatment of secondary hyperparathyroidism (SHPT) in adult patients with chronic kidney disease (CKD) on haemodialysis therapy. 4.2 Posology and method of administration Posology The recommended initial dose of etelcalcetide is 5 mg administered by bolus injection 3 times per week. Corrected serum calcium should be at or above the lower limit of the normal range prior to administration of first dose of Parsabiv, a dose increase, or reinitiation after a dose stop (see also dose adjustments based on serum calcium levels). Parsabiv should not be administered more frequently than 3 times per week. Dose titration Parsabiv should be titrated so that doses are individualised between 2.5 mg and 15 mg. -

Parsabiv® (Etelcalcetide) – Oxford Clinical Policy
UnitedHealthcare® Oxford Clinical Policy Parsabiv® (Etelcalcetide) Policy Number: PHARMACY 313.7 T2 Effective Date: April 1, 2021 Instructions for Use Table of Contents Page Related Policies Coverage Rationale ....................................................................... 1 • Drug Coverage Guidelines Prior Authorization Requirements ................................................ 2 Applicable Codes .......................................................................... 2 Background.................................................................................... 2 Clinical Evidence ........................................................................... 2 U.S. Food and Drug Administration ............................................. 3 References ..................................................................................... 3 Policy History/Revision Information ............................................. 3 Instructions for Use ....................................................................... 4 Coverage Rationale Initial Therapy Parsabiv (etelcalcetide) is proven for the treatment of secondary hyperparathyroidism with chronic kidney disease when the following criteria are met: Diagnosis of secondary hyperparathyroidism with chronic kidney disease; and Patient is on dialysis; and Patient is not receiving Parsabiv (etelcalcetide) in combination with Sensipar (cinacalcet hydrochloride); and Prescribed by or in consultation with an endocrinologist or nephrologist; and Dosing is in accordance with the United -

Clinical and Biochemical Outcomes of Cinacalcet Treatment of Familial
Rasmussen et al. Journal of Medical Case Reports 2011, 5:564 JOURNAL OF MEDICAL http://www.jmedicalcasereports.com/content/5/1/564 CASE REPORTS CASEREPORT Open Access Clinical and biochemical outcomes of cinacalcet treatment of familial hypocalciuric hypercalcemia: a case series Anne Qvist Rasmussen1*, Niklas Rye Jørgensen1,2 and Peter Schwarz1,3 Abstract Introduction: Familial hypocalciuric hypercalcemia is a rare benign autosomal-dominant genetic disease with high penetrance. In most cases, patients with familial hypocalciuric hypercalcemia experience unspecific physical discomfort or asymptomatic disease. These patients are typically characterized by mild to moderately increased blood ionized calcium and a normal to slightly elevated serum parathyroid hormone. Case presentation: Four female patients with familial hypocalciuric hypercalcemia with inactivating mutations in the CaSR gene were included in the treatment study. Three patients were related: two were siblings and one was the daughter of one of these. The ages of the related patients were 51 years, 57 years and 35 years. All three patients were carriers of the same mutation. The fourth patient, unrelated to the others, was 53 years old, and a carrier of a novel and previously unknown mutation leading to familial hypocalciuric hypercalcemia. All four patients were Caucasians of Danish nationality. Biochemically, all patients had elevated blood ionized calcium, serum parathyroid hormone, serum magnesium and total serum calcium, except one, whose serum parathyroid hormone was within the normal range prior to treatment. All patients were treated with cinacalcet in a dosage of 30 mg to 60 mg per day. Conclusion: Three months after the initiation of cinacalcet treatment, all our patients experiencing clinical signs of hypercalcemia had improved in self -reported well-being and in biochemical parameters. -

Mimpara, INN-Cinacalcet
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Mimpara 30 mg film-coated tablets Mimpara 60 mg film-coated tablets Mimpara 90 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Mimpara 30 mg film-coated tablets Each tablet contains 30 mg cinacalcet (as hydrochloride). Excipient with known effect Each tablet contains 2.74 mg of lactose. Mimpara 60 mg film-coated tablets Each tablet contains 60 mg cinacalcet (as hydrochloride). Excipient with known effect Each tablet contains 5.47 mg of lactose. Mimpara 90 mg film-coated tablets Each tablet contains 90 mg cinacalcet (as hydrochloride). Excipient with known effect Each tablet contains 8.21 mg of lactose. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). Mimpara 30 mg film-coated tablets Light green, oval (approximately 9.7 mm long and 6.0 mm wide), film-coated tablet marked “AMG” on one side and “30” on the other. Mimpara 60 mg film-coated tablets Light green, oval (approximately 12.2 mm long and 7.6 mm wide), film-coated tablet marked “AMG” on one side and “60” on the other. Mimpara 90 mg film-coated tablets Light green, oval (approximately 13.9 mm long and 8.7 mm wide), film-coated tablet marked “AMG” on one side and “90” on the other. 2 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Secondary hyperparathyroidism Adults Treatment of secondary hyperparathyroidism (HPT) in adult patients with end-stage renal disease (ESRD) on maintenance dialysis therapy. Paediatric population Treatment of secondary hyperparathyroidism (HPT) in children aged 3 years and older with end-stage renal disease (ESRD) on maintenance dialysis therapy in whom secondary HPT is not adequately controlled with standard of care therapy (see section 4.4). -

Effects of the Calcimimetic Cinacalcet Hcl on Cardiovascular Disease, Fracture, and Health-Related Quality of Life in Secondary Hyperparathyroidism
Kidney International, Vol. 68 (2005), pp. 1793–1800 Effects of the calcimimetic cinacalcet HCl on cardiovascular disease, fracture, and health-related quality of life in secondary hyperparathyroidism JOHN CUNNINGHAM,MARK DANESE,KURT OLSON,PRESTON KLASSEN, and GLENN M. CHERTOW University College London, The Middlesex Hospital, London, UK; Outcomes Insights, Inc., Newbury Park, California; Amgen, Inc., Thousand Oaks, California; and Department of Medicine, University of California, San Francisco, California Effects of the calcimimetic cinacalcet HCl on cardiovascular tion and diminished pain. These data suggest that, in addition disease, fracture, and health-related quality of life in secondary to its effects on PTH and mineral metabolism, cinacalcet had hyperparathyroidism. favorable effects on important clinical outcomes. Background. Secondary hyperparathyroidism (HPT) and ab- normal mineral metabolism are thought to play an important role in bone and cardiovascular disease in patients with chronic kidney disease. Cinacalcet, a calcimimetic that modulates the Secondary hyperparathyroidism (HPT) is a frequent calcium-sensing receptor, reduces parathyroid hormone (PTH) secretion and lowers serum calcium and phosphorus concen- component of the natural progression of chronic kidney trations in patients with end-stage renal disease (ESRD) and disease (CKD), typically developing when the glomeru- secondary HPT. lar filtration rate (GFR) drops below approximately Methods. We undertook a combined analysis of safety data 80 mL/min/1.73m2 for ≥3 months [1]. Secondary HPT (parathyroidectomy, fracture, hospitalizations, and mortality) is an adaptive response to CKD and arises from dis- from 4 similarly designed randomized, double-blind, placebo- controlled clinical trials enrolling 1184 subjects (697 cinacalcet, ruptions in the homeostatic control of serum calcium, 487 control) with ESRD and uncontrolled secondary HPT (in- serum phosphorus, and vitamin D, which are associated tact PTH ≥300 pg/mL). -

An Open0label, Single0dose Study to Evaluate the Safety, Tolerability
3URGXFW(WHOFDOFHWLGH 3URWRFRO1XPEHU 'DWH)HEUXDU\ 3DJHRI 7LWOH$Q2SHQODEHO6LQJOHGRVH6WXG\WR(YDOXDWHWKH6DIHW\7ROHUDELOLW\ 3KDUPDFRNLQHWLFVDQG3KDUPDFRG\QDPLFVRI(WHOFDOFHWLGH $0* LQ 3DHGLDWULF6XEMHFWV$JHGWROHVVWKDQ<HDUVZLWK6HFRQGDU\ +\SHUSDUDWK\URLGLVP V+37 5HFHLYLQJ0DLQWHQDQFH+DHPRGLDO\VLV $PJHQ3URWRFRO1XPEHU (WHOFDOFHWLGH (XGUD&7QXPEHU-- &OLQLFDO6WXG\6SRQVRU $PJHQ,QF 2QH$PJHQ&HQWHU'ULYH 7KRXVDQG2DNV&$ PPD .H\6SRQVRU&RQWDFW V 3K' &OLQLFDO3KDUPDFRORJ\DQG0HGLFDO6FLHQFHV 7HOPPD (PDLOPPD PPD 0'06F 0HGLFDO6FLHQFHV0HGLFDO'LUHFWRU 7HO PPD (PDLO PPD PPD 6WXG\0DQDJHU 7HOPPD (PDLOPPD 'DWH )HEUXDU\ &RQILGHQWLDOLW\1RWLFH 7KLVGRFXPHQWFRQWDLQVFRQILGHQWLDOLQIRUPDWLRQRI$PJHQ,QF 7KLVGRFXPHQWPXVWQRWEHGLVFORVHGWRDQ\RQHRWKHUWKDQWKHVLWHVWXG\VWDIIDQG PHPEHUVRIWKHLQVWLWXWLRQDOUHYLHZERDUGLQGHSHQGHQWHWKLFVFRPPLWWHHLQVWLWXWLRQDO VFLHQWLILFUHYLHZERDUGRUHTXLYDOHQW 7KHLQIRUPDWLRQLQWKLVGRFXPHQWFDQQRWEHXVHGIRUDQ\SXUSRVHRWKHUWKDQWKH HYDOXDWLRQRUFRQGXFWRIWKHFOLQLFDOLQYHVWLJDWLRQZLWKRXWWKHSULRUZULWWHQFRQVHQWRI $PJHQ,QF 1&71XPEHU 7KLV1&7QXPEHUKDVEHHQDSSOLHGWRWKHGRFXPHQW IRUSXUSRVHVRISRVWLQJRQFOLQLFDOWULDOVJRY &21),'(17,$/ 3URGXFW(WHOFDOFHWLGH 3URWRFRO1XPEHU 'DWH)HEUXDU\ 3DJHRI ,QYHVWLJDWRU¶V$JUHHPHQW ,KDYHUHDGWKHDWWDFKHGSURWRFROHQWLWOHG$Q2SHQODEHO6LQJOHGRVH6WXG\WR(YDOXDWH WKH6DIHW\7ROHUDELOLW\3KDUPDFRNLQHWLFVDQG3KDUPDFRG\QDPLFVRI(WHOFDOFHWLGH $0* LQ3DHGLDWULF6XEMHFWV$JHGWROHVVWKDQ<HDUVZLWK6HFRQGDU\ +\SHUSDUDWK\URLGLVP V+37 5HFHLYLQJ0DLQWHQDQFH+DHPRGLDO\VLVGDWHG )HEUXDU\DQGDJUHHWRDELGHE\DOOSURYLVLRQVVHWIRUWKWKHUHLQ ,DJUHHWRFRPSO\ZLWKWKH,QWHUQDWLRQDO&RQIHUHQFHRQ+DUPRQLVDWLRQ -

2017 Fda Peptide Harvest
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 10 April 2018 doi:10.20944/preprints201804.0126.v1 Peer-reviewed version available at Pharmaceuticals 2018, 11, 42; doi:10.3390/ph11020042 1 Review 2 2017 FDA PEPTIDE HARVEST 3 Othman Al Musaimi,1,2,# Danah Alshaer, 1,2,# Beatriz G. de la Torre,3,* Fernando Albericio,2,4,5.* 4 1 College of Health Sciences, University of KwaZulu-Natal, Durban 4000, South Africa 5 2 School of Chemistry, University of KwaZulu-Natal, Durban 4001, South Africa 6 3 KRISP, College of Health Sciences, University of KwaZulu-Natal, Durban 4001, South Africa 7 4 CIBER-BBN, Networking Centre on Bioengineering, Biomaterials and Nanomedicine, University of 8 Barcelona, 08028 Barcelona, Spain 9 5 Department of Organic Chemistry, University of Barcelona, 08028 Barcelona, Spain 10 * Correspondence: [email protected]; [email protected]; Tel.: +27-614009144 11 12 13 Abstract: 2017 was an excellent year in terms of new drugs (chemical entities and biologics) 14 approved by the FDA, with a total of forty-six. In turn, one of the highlights was the number of 15 peptides (six) included in this list. Here, the six peptides are analysed in terms of chemical structure, 16 synthetic strategy used for their production, source, biological target, and mode of action. 17 Keywords: pharmaceutical market; drugs; drug discovery; solid-phase peptide synthesis 18 Introduction 19 The financial investment associated with the pharmaceutical industry is one of the largest in the 20 industrial sector—surpassed only by the telecommunications sector. However, the number of new 21 products (drugs) entering the market each year is relatively low. -

Paricalcitol Versus Cinacalcet Plus Low-Dose Vitamin D for the Treatment
Nephrol Dial Transplant (2012) 27: 1942–1949 doi: 10.1093/ndt/gfr531 Advance Access publication 19 September 2011 Paricalcitol versus cinacalcet plus low-dose vitamin D for the treatment of secondary hyperparathyroidism in patients receiving haemodialysis: study design and baseline characteristics of the IMPACT SHPT study Markus Ketteler1, Kevin J. Martin2, Mario Cozzolino3, David Goldsmith4, Amit Sharma5, Samina Khan6, Emily Dumas6, Michael Amdahl6, Steven Marx6 and Paul Audhya6 1Division of Nephrology, Klinikum Coburg, Coburg, Germany, 2Department of Internal Medicine, Division of Nephrology, Saint Louis University, St Louis, MO, USA, 3Department of Medicine, Surgery and Dentistry, University of Milan, Renal Division, Hospital San Paolo, Milan, Italy, 4Renal and Transplantation Department, Guy’s Hospital, London, UK, 5Boise Kidney and Hypertension Institute, Boise, ID, USA and 6Abbott Laboratories, Abbott Park, IL, USA Correspondence and offprint requests to: Markus Ketteler; E-mail: [email protected] Abstract Introduction Background. Paricalcitol and cinacalcet are common thera- pies for patients on haemodialysis with secondary Secondary hyperparathyroidism (SHPT) is a major compli- hyperparathyroidism (SHPT). We conducted a multi-centre cation of chronic kidney disease (CKD) [1] resulting from study in 12 countries to compare the safety and efficacy of impaired calcium and phosphate homeostasis and a lack of paricalcitol and cinacalcet for the treatment of SHPT. vitamin D receptor (VDR) activation secondary to active Methods. Patients aged 18 years with Stage 5 chronic kidney disease receiving maintenance haemodialysis and vitamin D deficiency [2, 3]. SHPT is characterized by with intact parathyroid hormone (iPTH) 300–800 pg/mL, increased parathyroid hormone (PTH) synthesis and secre- calcium 8.4–10.0 mg/dL (2.09–2.49 mmol/L) and phospho- tion and progressive parathyroid gland hyperplasia [2]. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Etelcalcetide
Drug and Biologic Coverage Policy Effective Date .......................................... 12/1/2020 Next Review Date… ................................... 12/1/2021 Coverage Policy Number .................................. 1812 Etelcalcetide Table of Contents Related Coverage Resources Coverage Policy .................................................. 1 FDA Approved Indications .................................. 2 Recommended Dosing ....................................... 2 General Background ........................................... 2 Coding/ Billing Information .................................. 3 References .......................................................... 3 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion